- 1Center for Infectious Diseases, Beijing You'an Hospital, Capital Medical University, Beijing, China
- 2The Aaron Diamond AIDS Research Center, The Rockefeller University, New York, NY, United States
- 3Infectious Diseases Department, Peking Union Medical College Hospital, Beijing, China
- 4Infectious Diseases Department, Yunnan AIDS Care Center, Kunming, China
- 5Institute of Infectious Diseases, The Eighth People's Hospital of Guangzhou, Guangzhou, China
- 6Infectious Diseases Department, The Third People's Hospital of Kunming, Kunming, China
- 7Department of Infectious Diseases, Chongqing Infectious Disease Medical Center, Chongqing, China
- 8Department of Infectious Diseases, Guiyang Public Health Clinical Center, Guiyang, China
- 9Department of Clinical AIDS Research, The Third People's Hospital of Shenzhen, Shenzhen, China
- 10Department of Hematology, The Third People's Hospital of Hengyang, Hengyang, China
- 11Department of Infectious Disease, The Second Affiliated Hospital of Medical School of the Southeast University, Tianjin, China
- 12Department of Infectious Diseases, The Sixth People's Hospital of Hangzhou, Hangzhou, China
- 13Department of Infectious Diseases, The First Hospital of Changsha, Changsha, China
- 14Shanghai Public Health Clinical Center, Shanghai, China
- 15Department of Psychiatric and Neurology and Department of Epidemiology and Statistics, University of California, San Francisco, San Francisco, CA, United States
- 16School of Biomedical Engineering, Capital Medical University, Beijing, China
Background: Anxiety and depression continue to be significant comorbidities for people with HIV infection. We investigated the prevalence of and factors associated with anxiety and depression among adult HIV-infected patients across China.
Methods: In this cross-sectional study, we described clinical and psychosocial variables related to depression and anxiety in 4103 HIV-infected persons. Doctors assessed anxiety and depression by asking patients whether they had experienced anxiety or depression in the prior month. Patients also self-administered the Hospital Anxiety and Depression (HAD) scale; those with score ≥8 on HAD-A/D were considered to be at high risk of anxiety or depression.
Results: Associations between socio-demographic, psychosocial, and ART-related clinical factors and risk of depression or anxiety were investigated using multivariable logistic regression. Among patients assessed between 9/2014 and 11/2015, 27.4% had symptoms of anxiety, 32.9% had symptoms of depression, and 19.0% had both. Recentness of HIV diagnoses (P = 0.046) was associated with elevated odds of anxiety. Older age (P = 0.004), higher educational attainment (P < 0.001), employment (P = 0.001), support from family / friends (P < 0.001), and sleep disturbance (P < 0.001), and number of ART regimen switches (P = 0.046) were associated with risk of depression, while neither sex nor transmission route showed any associations. There were no significant associations with HIV-specific clinical factors including current CD4+ T cell count and current viral load.
Conclusions: Prevalence of symptoms of anxiety and depression is high in this cohort of treatment-experienced HIV patients. Psychological and social-demographic factors, rather than HIV disease status, were associated with risk of depression and anxiety. This finding highlights the need to deliver interventions to address the mental health issues affecting HIV-infected persons with fully successful immune restoration across China.
Introduction
Over half of all HIV-1-infected individuals suffer from mental health disorders (1–3) and anxiety and depression are common comorbidities in HIV-infected populations (4–6). The impact of mental health issues on HIV patients in resource-limited settings is often underestimated due to a lack of education and awareness both among physicians and patients, resulting in insufficient and ad-hoc screening and diagnosis of mental health conditions in this population (4, 7). The pathophysiology of anxiety/depression among HIV-infected patients is unclear, but may be related to clinical factors (e.g., the ability of HIV to infect the central nervous system (CNS) or impact of antiretroviral medications) or psychosocial in nature (e.g., availability of social support, issues related to substance abuse) (8–10). Recent studies have largely focused on the impact of specific antiretroviral agents (e.g., efavirenz) on mental health (11, 12). Regardless of its etiology, anxiety and depression is clinically important in this population and has the potential to impact quality of life, adherence to anti-retroviral medications, cognition, cause sleep disturbance and may weaken patients' immune system (13–16).
There are currently no guidelines to manage psychiatric disorders in the HIV clinic setting in China, despite the reality that these disorders adversely affect the course of HIV infection (17). Major anxiety and depression frequently go unrecognized and untreated and may foster severe consequences, such as rapid disease progression, suicide, high-risk behaviors and immune system impairment (18–20). In this study, we characterized the prevalence of symptoms of anxiety and depression in Chinese HIV-infected patients, identified risk factors, and sought to assess clinical impacts of anxiety and/or depression on treatment outcomes. We also investigated the utility of the Hospital Anxiety and Depression (HAD) instrument to identify missed-diagnoses when compared to a clinician-initiated one-item question asking patients to self-report anxiety and depression in the previous month.
Methods
We conducted a cross-sectional study among 4724 HIV-infected adults on treatment, collecting data from patients at 20 HIV treatment clinics across China. All participants provided written informed consent to complete a survey and have their medical data abstracted from their medical records. The study was approved by the Beijing You'an Hospital institutional review board.
Each participant completed the Hospital Anxiety and Depression (HAD) scale questionnaire, which consists of seven items each relating to depression (HAD-D) and anxiety (HAD-A) respectively. High risk of anxiety and depression was defined as a HAD score ≥8 on each subscale (21). Before self-administration of the HAD, clinicians asked patients if they had experienced any depressed mood or anxiety in the previous month and results were coded yes vs. no.
Demographic, behavioral, and psychosocial data were collected through self-administered survey. Clinical data was abstracted from medical records. This included HIV-specific data, including date of HIV diagnosis, history of medical conditions, current CD4+ cell counts and HIV RNA levels, and antiretroviral therapy (ART) regimen. The Pittsburgh Sleep Quality Index (PSQI) questionnaire, a 19-item questionnaire that assesses seven sleep components, was completed by each participant to evaluate sleep disturbance during the prior month. We used the PSQI cut off of a global score >5 on the PSQI instrument (15) (sensitivity of 90% and specificity of 87%) to define sleep disturbance in this cohort (22).
Statistical Analysis
Descriptive statistics are presented as means with standard deviations (SDs), or counts with proportions, as appropriate. Two sample t-tests were used to compare means, and χ2-tests were used to compare proportions. Logistic regression analysis was used to investigate associations between demographic, behavioral, psychosocial, and clinical factors and anxiety or depression. Odds ratios (ORs) for depression or anxiety were estimated with 95% confidence intervals (CIs). Factors with a P-value < 0.10 in univariate Logistic models were initially included in the multivariate Logistic model and were then eliminated using backward selection. Crude ORs are reported from univariate analysis; adjusted ORs are reported from multivariable logistic regression. All P-values were 2-sided, and P-values < 0.05 were considered significant. Analyses were conducted using SPSS 21.0.
Results
Characteristics of Study Population
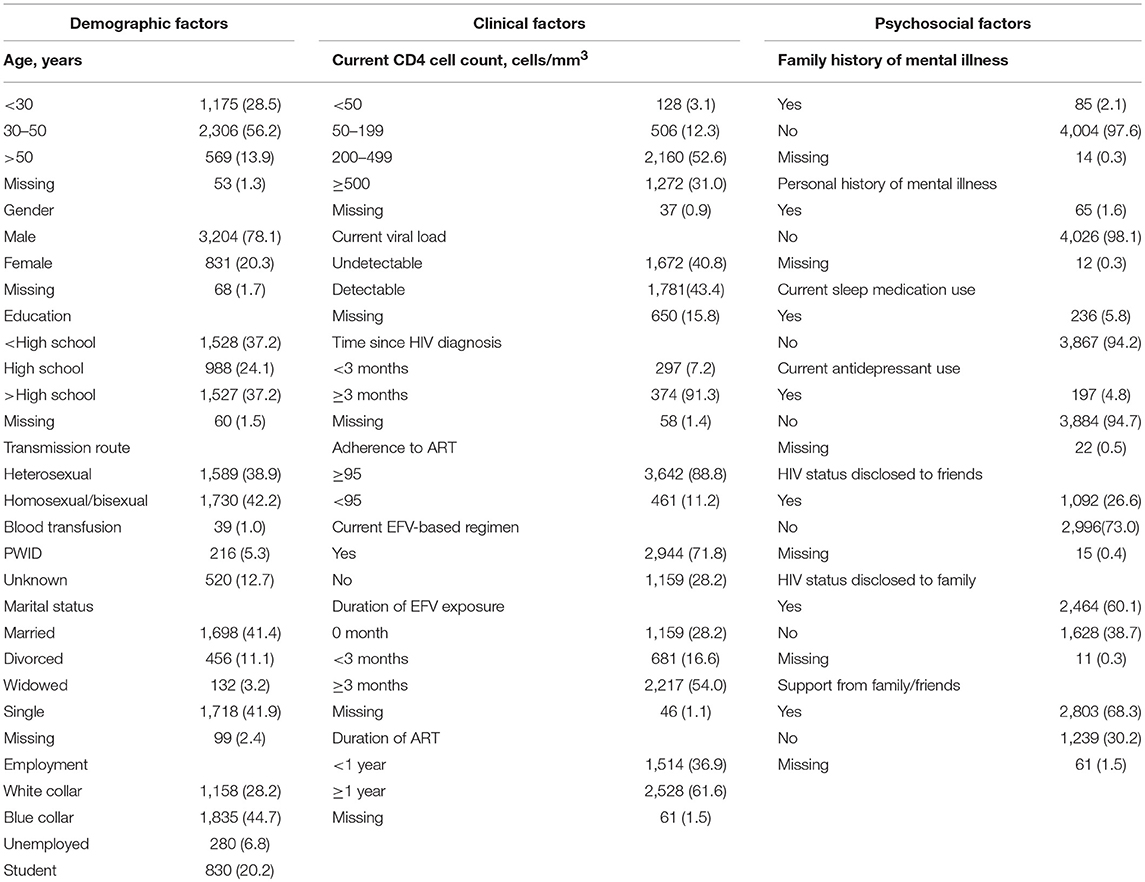
4103 HIV-infected persons were eligible for data anlaysis with the mean age being 37.6 ± 11.7 years (Table 1). Over three-quarters of the cohort were male patients. The cohort represented a diverse sample of educational achievement and employment status. Over 40% were infected through anal sex. The median time from HIV diagnosis to study enrollment was 27 months (interquartile range [IQR], 11–58 months); median duration of ART was 18 months (IQR, 6–43 months); 15.5% had a current CD4+ T cell count below 200 cells/mm3, and 40.8% were virally-suppressed. Three-quarters of patients were on first-line ART regimen (Table 1). Over 60% had disclosed their HIV status to their family members and close to 70% expressed feeling supported by their family members. In contrast, just over one quarter had disclosed their status to a friend.
Prevalence of Depression and Anxiety
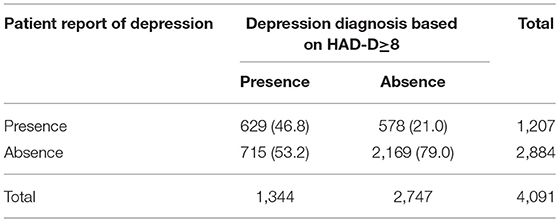
1,349 (32.9%) and 1,125 (27.4%) HIV-infected persons had symptoms of depression and anxiety based on the HAD-D and HAD-A, respectively, among whom 779 persons (19.0%) had symptoms consistent with both depression and anxiety. Out of 1,344 patients whose HAD-D score indicated likely depression, 715 (53.2%) did not report feeling depressed in the previous month in response to the clinician-initiated question (Table 2). Meanwhile, 578 (21.0%) of those whose HAD-D score suggested that they were not depressed responded that they had in fact experienced depressed mood in the last month.
Factors Associated With Depression and Anxiety
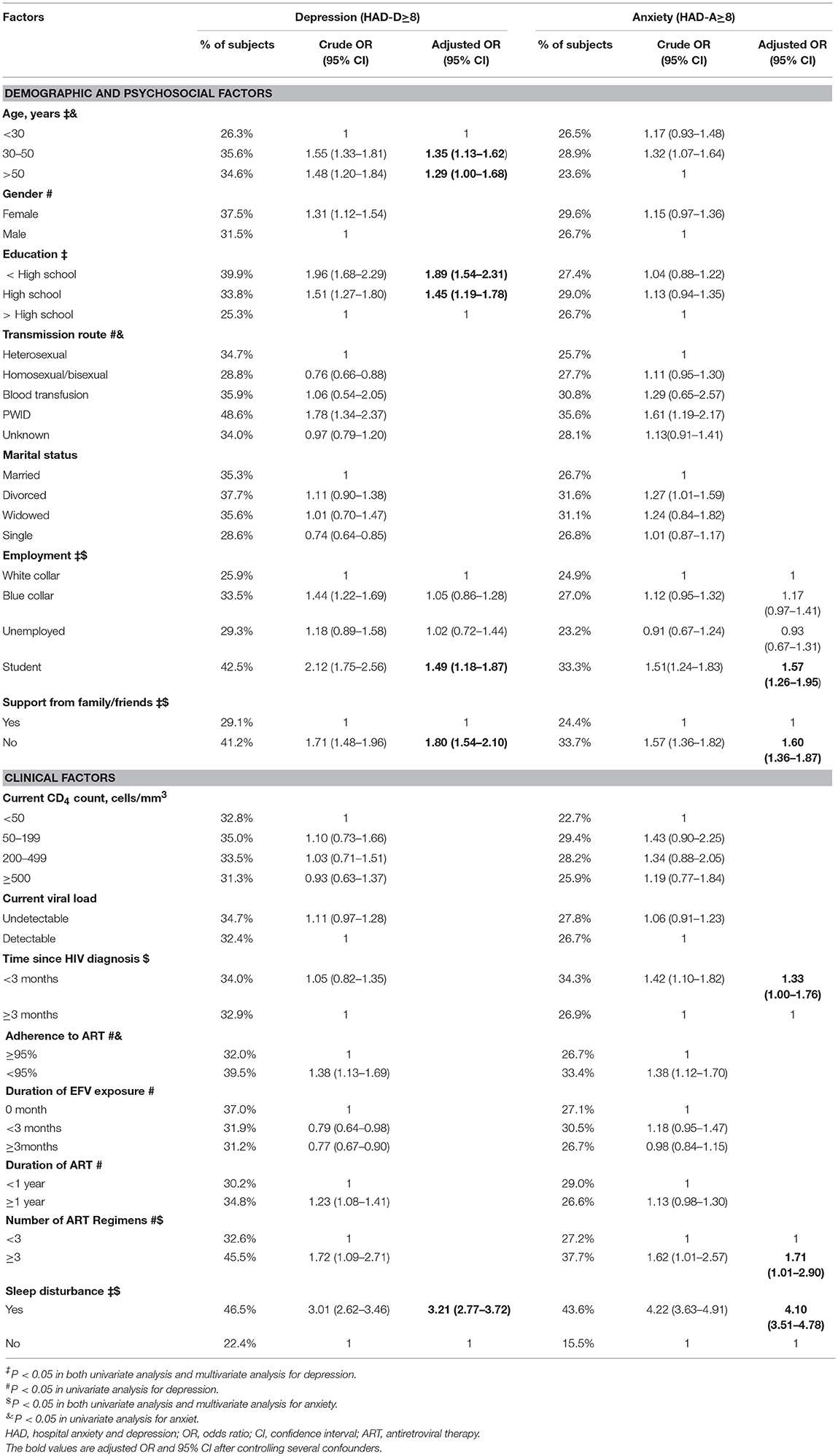
In univariate analyses, factors associated with likely depression (HAD-D ≥ 8) or anxiety (HAD-A ≥ 8) included age, sex, education, transmission route, employment, support from family/friends, time of diagnosed with HIV infection, drug adherence, duration of EFV exposure, duration of ART, number of ART regimens, and sleep disturbance. There were no significant associations with HIV-specific clinical factors including current CD4+ T cell count and current viral load.
In the final multivariate model, factors associated with depression based on the HAD included age (P = 0.004), education (P < 0.001), and employment (P = 0.001), while factors associated with anxiety included time since HIV diagnosis (P = 0.046), number of ART regimen (P = 0.046), employment (P < 0.001), support from family/friends (P < 0.001), and sleep disturbance (P < 0.001) (Table 3).
Discussion
This study represents one of the largest epidemiologic studies of the prevalence of symptoms of anxiety and depression among HIV-infected persons in the ART era as measured by the validated and frequently-used HAD scale (22–25). Our estimates of 32.9% prevalence of depressive symptoms and 27.4% prevalence of anxiety symptoms are lower than those reported in a systematic review of studies measuring mental health burden among people living with HIV in China that reported median prevalence of depression and anxiety of 60.4 and 43.1% respectively (2). However the authors of that review caution that their data may not be generalizable due to low quality of studies and high risk of bias in the samples (2) as many of these studies were conducted among former plasma donors and injecting drug users who were infected in the first waves of the HIV epidemic in China and may not be representative of more recently diagnosed individuals who tend to be infected through sexual contact (2). In addition, our study was conducted among patients currently accessing ART whereas earlier studies included both treated and untreated patients. A recent study of current depression among recently-diagnosed men who have sex with men (MSM) found 36% prevalence of depression, (26) in line with our finding of 34% depression prevalence among recently-diagnosed patients. People who inject drugs had the highest prevalence of depression and anxiety, in line with a rich literature documenting the comorbidities of mental health and substance use (4, 27, 28).
Students had higher rates of both anxiety and depression, an effect that remained even after controlling for age. As infections among young people and students continue to rise in China (29), it will become increasingly important to develop mental health interventions that have been shown to be effective for young people in other contexts, including ones that could be group-based, web-based, dyadic or individual (30, 31). Age older than 30 and less education were also associated with increased odds of depression in this cohort, a trend that has been seen in other studies as well (32).
In our study the length of time since HIV diagnosis was found to be associated with high anxiety symptoms, with a significant association between shorter duration since diagnosis and anxiety. Anxiety can be considered a normal emotional response to the reality of living with HIV and this may explain the higher rate of anxiety in the first several months after diagnosis (20). This finding is in line with that of another study that found high rates of depression in relation to duration of infection (6), suggesting that the provision of mental health services at the time of diagnosis could be critical to manage the risk of depression and anxiety among recently-diagnosed individuals. Positive-affect skills interventions to support recently-diagnosed individuals have been shown to improve psychological health, decrease the use of anti-depressants, and support adjustment to HIV-positive status (33) and could be piloted in Chinese patient populations.
Consistent with other studies, we found the patients who reported high levels of support from family or friends had lower rates of symptoms of anxiety and depression (10, 34). This suggests that interventions designed to build the capacity of family and friends to support newly-diagnosed patients in the acceptance of their disease and in developing positive coping strategies could have mental health benefits.
Despite a high prevalence of anxiety and depression among HIV-infected persons, less than 5% of patients with borderline or likely depression were regularly using anti-depressants. Prior studies have also noted that most patients in China with anxiety or depression remain untreated and often have a poor understanding of available treatment options (20, 35). This is perhaps not surprising given the chronic and severe undersupply of mental health services in China (36, 37).
We did not find a relationship between high likelihood of depression and anxiety and clinical factors like immune function. However frequent switching of ART regimens was associated with higher proportion of depression, which makes sense: someone who has had trouble achieving or maintaining viral suppression is likely to experience anxiety and depression related to anticipated downward progression of their disease. Unlike in other studies (11, 19), patients on EFV-based regimens did not have elevated odds of anxiety or depression. However, this is likely due to a bias in the sample in that patients who had suffered CNS side effects like anxiety/depression from EFV may have switched regimens prior to this cross-sectional study, leaving only patients who did not suffer EFV-related side effects in the sample.
Asking patients to report experience of anxiety or depression in the previous month resulted in significant under-reporting of depression when compared to the HAD scales. Low recognition of mental health needs have been well studied in the US and Western Europe (8) and leads to under-utilization of mental health services. Fewer studies have been conducted in China, though two recent studies among rural residents reported low recognition of depression and anxiety (38) and low awareness of where to access mental health services (39). While introducing an initial screening question could be one way to identify a proportion of people who self-identify as experiencing mental health issues and these could be referred to mental health services, the low recognition of depression and anxiety in the population suggests that relying on such a question alone would miss a large proportion of patients who are identified as at risk of depression and anxiety through the HAD screening instrument. The introduction of a standardized assessment of mental health into HIV services could be done at hospitals where patients access ART or through the Center for Disease Control system that manages follow up and could be an effective way to identify patients who could benefit from clinical evaluation given that these mental health issues are treatable.
Our study had several potential limitations. The cross-sectional study design did not allow for assessment of the temporal relationship between anxiety/depression and factors (e.g., depression improvement over time or pre- and post- ART), the direction of causality, or assessment of whether anxiety/depression were transient or chronic in nature. Among our study's strengths is its large size and geographic diversity across 14 provinces in China and inclusion of many sub-populations. Also important was its use of validated measures to assess risk for anxiety and depression and that could easily be integrated into routine clinical practice (9, 22, 40).
In summary, the high prevalence of anxiety and depression symptoms among treatment-experienced HIV-infected individuals suggests that routinely administering a standardized mental health assessment to newly-diagnosed individuals and perhaps students would be a useful first step to identify those in need of further clinical evaluation. In order for the introduction of such an assessment to translate to better mental health outcomes, HIV clinics would need to identify optimal models for the provision of mental health interventions to their patients, whether through on-site service provision or a strong referral system to mental health professionals and other social support services.
Author Contributions
XH, HC, KM, and XinL led the analysis and writing of this manuscript. XH, KM, HaW, YC, KY, HC, and JH contributed to the final version. HaW is the Principle Investigator of and designed the study. XiaL, TZ, WX, HH, CL, SH, WC, HZ, CH, SL, HuW, XuL, PM, RY, GX, TL, DD, HC, YC, AS were involved in managing the data collection. All authors reviewed and approved the final version of the manuscript.
Funding
This work was supported by the Chinese Government 13th Five-Year Plan (2017ZX10201101, 2018ZX10302104-001, 2018ZX10302104), Major Project of Beijing Municipal Science and Technology Committee (D161100000416003, D171100000517003), the National Natural Science Foundation of China (No. 81571973), the NSFC-NIH Biomedical collaborative research program (81761128001), The Capital Health Research and Development of Special Fund (2016-1-2182), and Beijing Key Laboratory (No. BZ0089).
Conflict Of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank the site leaders and other SAD study group members, Dr. Zhihao Meng (Longtan Hospital of Guangxi), Jinsong Bai (the Third People's Hospital of Kunming), XuL (the Third People's Hospital of Hengyang), Daling Tan (the People's Hospital of Luzhai), Fuxiang Wang (the First Affiliated Hospital of Harbin Medical University), Lianguo Ruan (Wuhan Medical Treatment Center), Hongxin Zhao (Beijing Ditan Hospital), Hongxia Wei (the Second Hospital of Nanjing Affiliated to Southeast University Medical College), Yanfen Liu (the Fourth People's Hospital of Nanning), JianhuaYu (the Sixth People's Hospital of Hangzhou), Hongzhou Lu (Shanghai Public Health Clinical Center Affiliated to Fudan University), Min Wang (the First People's Hospital of Changsha), whom they acknowledge as critical in the development, implementation, and analysis of this study.
References
1. Whetten K, Reif S, Whetten R, and Murphy-McMillan LK. Trauma, mental health, distrust, and stigma among HIV-positive persons: implications for effective care. Psychosom Med. (2008) 70:531–8. doi: 10.1097/PSY.0b013e31817749dc
2. Niu L, Luo D, Liu Y, Silenzio VM, Xiao S. The mental health of people living with HIV in China, 1998-2014: a systematic review. PLoS ONE (2016) 11:e0153489. doi: 10.1371/journal.pone.0153489
3. Li J, Mo PK, Kahler CW, Lau JT, Du M, Dai Y, et al. Prevalence and associated factors of depressive and anxiety symptoms among HIV-infected men who have sex with men in China. AIDS Care (2016) 28:465–70. doi: 10.1080/09540121.2015.1118430
4. Charlson FJ, Baxter AJ, Cheng HG, Shidhaye R, Whiteford HA. The burden of mental, neurological, and substance use disorders in China and India: a systematic analysis of community representative epidemiological studies. Lancet (2016) 388:376–89. doi: 10.1016/S0140-6736(16)30590-6
5. Olagunju AT, Adeyemi JD, Ogbolu RE, Campbell EA. A study on epidemiological profile of anxiety disorders among people living with HIV/AIDS in a sub-Saharan Africa HIV clinic. AIDS Behav. (2012) 16:2192–7. doi: 10.1007/s10461-012-0250-x
6. Pappin M, Wouters E, Booysen FL. Anxiety and depression amongst patients enrolled in a public sector antiretroviral treatment programme in South Africa: a cross-sectional study. BMC Public Health (2012) 12:244. doi: 10.1186/1471-2458-12-244
7. Ian E, Gwen CL, Soo CT, Melissa C, Chun-Kai H, Eosu K, et al. The burden of HIV-associated neurocognitive disorder (HAND) in the Asia-Pacific region and recommendations for screening. Asian J Psychiatr. (2015) 22:182–9. doi: 10.1016/j.ajp.2015.10.009
8. Heaton RK, Franklin DR Jr, Deutsch R, Letendre S, Ellis RJ, Casaletto K, et al. Neurocognitive change in the era of HIV combination antiretroviral therapy: the longitudinal CHARTER study. Clin Infect Dis. (2015) 60:473–80. doi: 10.1093/cid/ciu862
9. Heywood W, Lyons A. HIV and elevated mental health problems: diagnostic, treatment, and risk patterns for symptoms of depression, anxiety, and stress in a national community-based cohort of gay men living with HIV. AIDS Behav (2016) 20:1632–45. doi: 10.1007/s10461-016-1324-y
10. Familiar I, Murray S, Ruisenor-Escudero H, Sikorskii A, Nakasujja N, Boivin MJ, et al. Socio-demographic correlates of depression and anxiety among female caregivers living with HIV in rural Uganda. AIDS Care (2016) 28:1–5. doi: 10.1080/09540121.2016.1191609
11. Gaida R, Truter I, Grobler C, Kotze T, Godman B. A review of trials investigating efavirenz-induced neuropsychiatric side effects and the implications. Expert Rev Anti Infect Ther. (2016) 14:377–88. doi: 10.1586/14787210.2016.1157469
12. Kelly CM, van Oosterhout JJ, Ngwalo C, Stewart RC, Benjamin L, Robertson KR, et al. HIV associated neurocognitive disorders (HAND) in Malawian adults and effect on adherence to combination anti-retroviral therapy: a cross sectional study. PLoS ONE (2014) 9:e98962. doi: 10.1371/journal.pone.0098962
13. Miners A, Phillips A, Kreif N, Rodger A, Speakman A, Fisher M, et al. Health-related quality-of-life of people with HIV in the era of combination antiretroviral treatment: a cross-sectional comparison with the general population. Lancet HIV (2014) 1:e32–40. doi: 10.1016/S2352-3018(14)70018-9
14. Shacham E, Onen NF, Donovan MF, Rosenburg N, Overton ET. Psychiatric diagnoses among an HIV-infected outpatient clinic population. J Int Assoc Provid AIDS Care (2016) 15:126–30. doi: 10.1177/2325957414553846
15. McGuire JL, Kempen JH, Localio R, Ellenberg JH, Douglas SD. Immune markers predictive of neuropsychiatric symptoms in HIV-infected youth. Clin Vaccine Immunol. (2015) 22:27–36. doi: 10.1128/CVI.00463-14
16. Huang X, Li H, Meyers K, Xia W, Meng Z, Li C, et al. Burden of sleep disturbances and associated risk factors: a cross-sectional survey among HIV-infected persons on antiretroviral therapy across China. Sci Rep (2017) 7:3657. doi: 10.1038/s41598-017-03968-3
17. Sun W, Wu M, Qu P, Lu C, Wang L. Psychological well-being of people living with HIV/AIDS under the new epidemic characteristics in China and the risk factors: a population-based study. Int J Infect Dis. (2014) 28:147–52. doi: 10.1016/j.ijid.2014.07.010
18. Garey L, Bakhshaie J, Sharp C, Neighbors C, Zvolensky MJ, Gonzalez A. Anxiety, depression, and HIV symptoms among persons living with HIV/AIDS: the role of hazardous drinking. AIDS Care (2015) 27:80–5. doi: 10.1080/09540121.2014.956042
19. Yehia BR, Cui W, Thompson WW, Zack MM, McKnight-Eily L, DiNenno E, et al. HIV testing among adults with mental illness in the United States. AIDS Patient Care STDS (2014) 28:628–34. doi: 10.1089/apc.2014.0196
20. Nacher M, Adriouch L, Godard Sebillotte C, Hanf M, Vantilcke V, El Guedj M, et al. Predictive factors and incidence of anxiety and depression in a cohort of HIV-positive patients in French Guiana. AIDS Care (2010) 22:1086–92. doi: 10.1080/09540121003599232
21. Christodoulou C, Michopoulos J, Tournikioti K, Douzenis A, Bouras G, Seretis D, et al. Hospital anxiety and depression scale. a quantitative analysis in medical outpatients, psychiatric outpatients and normal subjects. Psychiatriki (2010) 21:279–86.
22. Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
23. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
24. Darko DF, McCutchan JA, Kripke DF, Gillin JC, Golshan S. Fatigue, sleep disturbance, disability, and indices of progression of HIV infection. Am J Psychiatry (1992) 149:514–20. doi: 10.1176/ajp.149.4.514
25. Di Riso D, Bobbio A, Chessa D, Lis A, Mazzeschi C. Analysis of the interplay between depression, anxiety, and psychological resources in adolescence using self-report measures. Int J Psychiatry Clin Pract. (2014) 18:103–11. doi: 10.3109/13651501.2014.890227
26. Tao J, Vermund SH, Lu H, Ruan Y, Shepherd BE, Kipp AM, et al. Impact of depression and anxiety on initiation of antiretroviral therapy among men who have sex with men with newly diagnosed HIV infections in China. AIDS Patient Care STDs (2017) 31:96–104. doi: 10.1089/apc.2016.0214
27. Chibanda D, Benjamin L, Weiss HA, Abas M. Mental, neurological, and substance use disorders in people living with HIV/AIDS in low- and middle-income countries. J Acquir Immune Defic Syndr. (2014) 67(Suppl 1):S54–67. doi: 10.1097/QAI.0000000000000258
28. Ali MM, Dean D Jr, Lipari R, Dowd WN, Aldridge AP, Novak SP. The mental health consequences of nonmedical prescription drug use among adolescents. J Ment Health Policy Econ. (2015) 18:3–15.
29. McLaughlin K. HIV infections are spiking among young gay Chinese. Science (2017) 355:1359. doi: 10.1126/science.355.6332.1359
30. Li HH, Holroyd E, Lau J, Li X. Stigma, subsistence, intimacy, face, filial piety, and mental health problems among newly HIV-diagnosed men who have sex with men in China. J Assoc Nurses AIDS Care (2015) 26:454–63. doi: 10.1016/j.jana.2015.02.004
31. Chen L, Wang L, Qiu XH, Yang XX, Qiao ZX, Yang YJ, et al. Depression among Chinese university students: prevalence and socio-demographic correlates. PLoS ONE (2013) 8:e58379. doi: 10.1371/journal.pone.0058379
32. Thielke SM, Diehr P, Unutzer J. Prevalence, incidence, and persistence of major depressive symptoms in the Cardiovascular Health Study. Aging Ment Health (2010) 14:168–76. doi: 10.1080/13607860903046537
33. Moskowitz JT, Carrico AW, Duncan LG, Cohn MA, Cheung EO, Batchelder A, et al. Randomized controlled trial of a positive affect intervention for people newly diagnosed with HIV. J Consul Clin Psychol. (2017) 85:409–23. doi: 10.1037/ccp0000188
34. Cederbaum JA, Rice E, Craddock J, Pimentel V, Beaver P. Social networks of HIV-positive women and their association with social support and depression symptoms. Women Health (2016) 57:1–15. doi: 10.1080/03630242.2016.1157126
35. Rodkjaer L, Laursen T, Balle N, Sodemann M. Depression in patients with HIV is under-diagnosed: a cross-sectional study in Denmark. HIV Med. (2010) 11:46–53. doi: 10.1111/j.1468-1293.2009.00741.x
36. Qian J. Mental health care in China: providing services for under-treated patients. J Mental Health Policy Econom. (2012) 15:179–86.
37. Wu P, Li LP, Jin J, Yuan XH, Liu X, Fan B, et al. Need for mental health services and service use among high school students in China. Psychiatric Serv. (2012) 63:1026–31. doi: 10.1176/appi.ps.201200090
38. Li J, Li X, Hu S, Yu Y, Yan XF, Jiang LX. ST-segment elevation myocardial infarction in the eastern urban China: from 2001 to 2011. Chin J Cardiol (2016) 44:303–8. doi: 10.3760/cma.j.issn.0253-3758.
39. Yu Y, Liu ZW, Hu M, Liu HM, Yang JP, Zhou L, et al. Mental health help-seeking intentions and preferences of rural Chinese adults. PLoS ONE (2015) 10:e0141889. doi: 10.1371/journal.pone.0141889
Keywords: HIV-1, anxiety, depression, Hospital Anxiety and Depression (HAD) scale, mental health, prevalence, risk factors
Citation: Huang X, Meyers K, Liu X, Li X, Zhang T, Xia W, Hou J, Song A, He H, Li C, He S, Cai W, Zhong H, Huang C, Liu S, Wang H, Ling X, Ma P, Ye R, Xiao G, Li T, Ding D, Yaffe K, Chen H, Chen Y and Wu H (2018) The Double Burdens of Mental Health Among AIDS Patients With Fully Successful Immune Restoration: A Cross-Sectional Study of Anxiety and Depression in China. Front. Psychiatry 9:384. doi: 10.3389/fpsyt.2018.00384
Received: 02 March 2018; Accepted: 30 July 2018;
Published: 24 August 2018.
Edited by:
Jutta Lindert, University of Applied Sciences Emden Leer, GermanyReviewed by:
Victor Lasebikan, University of Ibadan, NigeriaCostin Roventa, Spitalul Clinic Colentina, Romania
Copyright © 2018 Huang, Meyers, Liu, Li, Zhang, Xia, Hou, Song, He, Li, He, Cai, Zhong, Huang, Liu, Wang, Ling, Ma, Ye, Xiao, Li, Ding, Yaffe, Chen, Chen and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hao Wu, whdoc@sina.com
Yaokai Chen, yaokaichen@hotmail.com
Hui Chen, chenhui@ccmu.edu.cn
†These authors have contributed equally to this work
 Xiaojie Huang
Xiaojie Huang Kathrine Meyers2†
Kathrine Meyers2† Xinchao Liu
Xinchao Liu Jiahua Hou
Jiahua Hou Aixin Song
Aixin Song Shuiqing Liu
Shuiqing Liu Kristine Yaffe
Kristine Yaffe Hao Wu
Hao Wu