Visual Perception, Fine Motor, and Visual-Motor Skills in Very Preterm and Term-Born Children before School Entry–Observational Cohort Study
Abstract
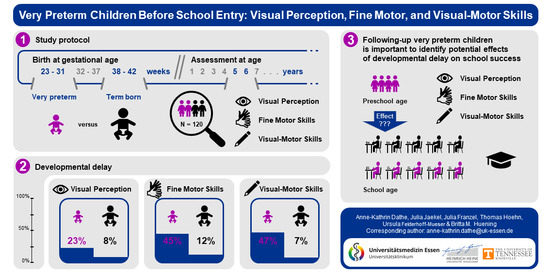
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Standard Protocol Approvals and Patient Consents
2.3. Clinical Characteristics
2.4. Parental Education
2.5. Outcome Measures
2.6. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Pierrat, V.; Marchand-Martin, L.; Arnaud, C.; Kaminski, M.; Resche-Rigon, M.; Lebeaux, C.; Bodeau-Livinec, F.; Morgan, A.S.; Goffinet, F.; Marret, S.; et al. Neurodevelopmental outcome at 2 years for preterm children born at 22 to 34 weeks’ gestation in France in 2011: EPIPAGE-2 cohort study. BMJ 2017, 358, j3448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santhakumaran, S.; Statnikov, Y.; Gray, D.; Battersby, C.; Ashby, D.; Modi, N. Survival of very preterm infants admitted to neonatal care in England 2008–2014: time trends and regional variation. Arch. Dis. Child. Fetal Neonatal Ed. 2018, 103, F208–F215. [Google Scholar] [CrossRef] [PubMed]
- Van Haastert, I.C.; Groenendaal, F.; Uiterwaal, C.S.P.; Termote, J.U.; Van Der Heide-Jalving, M.; Eijsermans, M.J.; Gorter, J.W.; Helders, P.J.M.; Jongmans, M.J.; De Vries, L.S. Decreasing Incidence and Severity of Cerebral Palsy in Prematurely Born Children. J. Pediatr. 2011, 159, 86–91.e1. [Google Scholar] [CrossRef] [PubMed]
- Potharst, E.S.; Van Wassenaer, A.G.; Houtzager, B.A.; Van Hus, J.W.; Last, B.F.; Kok, J.H. High Incidence of Multi-Domain Disabilities in Very Preterm Children at Five Years of Age. J. Pediatr. 2011, 159, 79–85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woodward, L.J.; Clark, C.A.C.; Bora, S.; Inder, T.E. Neonatal White Matter Abnormalities an Important Predictor of Neurocognitive Outcome for Very Preterm Children. PLoS ONE 2012, 7, e51879. [Google Scholar] [CrossRef] [PubMed]
- Løhaugen, G.C.C.; Gramstad, A.; I Evensen, K.A.; Martinussen, M.; Lindqvist, S.; Indredavik, M.; Vik, T.; Brubakk, A.-M.; Skranes, J. Cognitive profile in young adults born preterm at very low birthweight. Dev. Med. Child Neurol. 2010, 52, 1133–1138. [Google Scholar] [CrossRef]
- Twilhaar, E.S.; Wade, R.M.; De Kieviet, J.F.; Van Goudoever, J.B.; Van Elburg, R.M.; Oosterlaan, J. Cognitive Outcomes of Children Born Extremely or Very Preterm Since the 1990s and Associated Risk Factors. JAMA Pediatr. 2018, 172, 361–367. [Google Scholar] [CrossRef]
- Bos, A.F.; van Braeckel, K.N.J.A.; Hitzert, M.M.; Tanis, J.C.; Roze, E. Development of fine motor skills in preterm infants. Dev. Med. Child Neurol. 2013, 55 (Suppl. 4), 1–4. [Google Scholar] [CrossRef] [Green Version]
- De Kieviet, J.F.; Piek, J.P.; Aarnoudse-Moens, C.S.; Oosterlaan, J. Motor development in very preterm and very low-birth-weight children from birth to adolescence: A meta-analysis. JAMA 2009, 302, 2235–2242. [Google Scholar] [CrossRef]
- Marlow, N.; Hennessy, E.M.; Bracewell, M.A.; Wolke, D. Motor and executive function at 6 years of age after extremely preterm birth. Pediatrics 2007, 120, 793–804. [Google Scholar] [CrossRef] [Green Version]
- Pritchard, V.E.; Bora, S.; Austin, N.C.; Levin, K.J.; Woodward, L.J. Identifying very preterm children at educational risk using a school readiness framework. Pediatrics 2014, 134, e825–e832. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feder, K.P.; Majnemer, A. Handwriting development, competency, and intervention. Dev. Med. Child Neurol. 2007, 49, 312–317. [Google Scholar] [CrossRef] [PubMed]
- Geldof, C.J.A.; van Wassenaer, A.G.; de Kieviet, J.F.; Kok, J.H.; Oosterlaan, J. Visual perception and visual-motor integration in very preterm and/or very low birth weight children: A meta-analysis. Res. Dev. Disabil. 2012, 33, 726–736. [Google Scholar] [CrossRef] [PubMed]
- Jaekel, J.; Baumann, N.; Wolke, D. Effects of gestational age at birth on cognitive performance: A function of cognitive workload demands. PLoS ONE 2013, 8, e65219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bolk, J.; Padilla, N.; Forsman, L.; Broström, L.; Hellgren, K.; Åden, U. Visual-motor integration and fine motor skills at 6½ years of age and associations with neonatal brain volumes in children born extremely preterm in Sweden: A population-based cohort study. BMJ Open 2018, 8, e020478. [Google Scholar] [CrossRef] [Green Version]
- Kadar, M.; Wan Yunus, F.; Tan, E.; Chai, S.C.; Razaob Razab, N.A.; Mohamat Kasim, D.H. A systematic review of occupational therapy intervention for handwriting skills in 4–6 year old children. Aust. Occup. Ther. J. 2019, 67, 1–10. [Google Scholar] [CrossRef]
- Kokštejn, J.; Musálek, M.; Tufano, J.J. Are sex differences in fundamental motor skills uniform throughout the entire preschool period? PLoS ONE 2017, 12, e0176556. [Google Scholar] [CrossRef]
- Maeda, Y.; Yoon, S.Y. A meta-analysis on gender differences in mental rotation ability measured by the Purdue Spatial Visualization Tests: Visualization of Rotations (PSVT:R). Educ. Psychol. Rev. 2013, 25, 69–94. [Google Scholar] [CrossRef]
- Peyre, H.; Hoertel, N.; Bernard, J.Y.; Rouffignac, C.; Forhan, A.; Taine, M.; Heude, B.; Ramus, F. EDEN Mother—Child Cohort Study Group. Sex differences in psychomotor development during the preschool period: A longitudinal study of the effects of environmental factors and of emotional, behavioral, and social functioning. J. Exp. Child Psychol. 2019, 178, 369–384. [Google Scholar] [CrossRef]
- Josman, N.; Abdallah, T.M.; Engel-Yeger, B. A comparison of visual-perceptual and visual-motor skills between Palestinian and Israeli children. Am. J. Occup. Ther. 2006, 60, 215–225. [Google Scholar] [CrossRef] [Green Version]
- Goyen, T.-A.; Lui, K. Developmental coordination disorder in "apparently normal" schoolchildren born extremely preterm. Arch. Dis. Child 2009, 94, 298–302. [Google Scholar] [CrossRef] [PubMed]
- Volpe, J.J. (Ed.) Volpe’s Neurology of the Newborn, 6th ed.; Elsevier: Philadelphia, PA, USA, 2018; p. 1189. ISBN 9780323428767. [Google Scholar]
- Jobe, A.H. The new bronchopulmonary dysplasia. Curr. Opin. Pediatr. 2011, 23, 167–172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evans, N. Diagnosis of patent ductus arteriosus in the preterm newborn. Arch. Dis. Child 1993, 68, 58–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldstein, B.; Giroir, B.; Randolph, A. International pediatric sepsis consensus conference: Definitions for sepsis and organ dysfunction in pediatrics. Pediatr. Crit. Care Med. 2005, 6, 2–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quinn, G.E. The international classification of retinopathy of prematurity revisited. Arch. Ophthalmol. 2005, 123, 991–999. [Google Scholar] [CrossRef]
- ISCED. International Standard Classification of Education: ISCED 2011; UNESCO Institute for Statistics: Montreal, QC, Canada, 2012; p. 84. ISBN 978-92-9189-123-8. [Google Scholar]
- Büttner, G.; Dacheneder, W.; Schneider, W.; Weyer, K. Frostigs Test der Visuellen Wahrnehmung—2 (FEW-2); Hogrefe: Göttingen, Germany, 2008. [Google Scholar]
- Hammill, D.D.; Pearson, N.A.; Voress, J.K. Developmental Test of Visual Perception, 2nd ed.; Pro-Ed: Austin, TX, USA, 1993. [Google Scholar]
- Brown, T.; Hockey, S.C. The validity and reliability of developmental test of visual perception-2nd edition (DTVP-2). Phys. Occup. Ther. Pedaitr. 2013, 33, 426–439. [Google Scholar] [CrossRef]
- Beery, K.E.; Buktenica, N.A.; Beery, N.A. The Beery-Buktenica Developmental Test of Visual-Motor Integration: Administration, Scoring and Teaching Manual, 6th ed.; Pearson: Minneapolis, MN, USA, 2010. [Google Scholar]
- Petermann, F.; Bös, K.; Kastner, J. Movement Assessment Battery for Children-2: (Movement ABC-2); deutschsprachige Adaptation nach S. E. Henderson, D. A. Sudgen und A. L. Barnett; Manual. 2nd ed. Frankfurt am Main: Pearson Assessment & Information. 2009; 177p, ISBN 978-3-9812353-2-6. [Google Scholar]
- Henderson, S.E.; Sugden, D.A.; Barnett, A.L.; Smits-Engelsman, B. Movement Assessment Battery for Children-2, 2nd ed.; The Psychological Corporation: London, UK, 2007. [Google Scholar]
- Slater, L.M.; Hillier, S.L.; Civetta, L.R. The clinimetric properties of performance-based gross motor tests used for children with developmental coordination disorder: A systematic review. Pediatr. Phys. Ther. 2010, 22, 170–179. [Google Scholar] [CrossRef]
- Piek, J.P.; Hands, B.; Licari, M.K. Assessment of motor functioning in the preschool period. Neuropsychol. Rev. 2012, 22, 402–413. [Google Scholar] [CrossRef]
- Geldof, C.J.; Oosterlaan, J.; Vuijk, P.J.; de Vries, M.J.; Kok, J.H.; van Wassenaer-Leemhuis, A.G. Visual sensory and perceptive functioning in 5-year-old very preterm/very-low-birthweight children. Dev. Med. Child Neurol. 2014, 56, 862–868. [Google Scholar] [CrossRef] [Green Version]
- Jenni, O. Wie Kinder die Welt abbilden—und was man daraus folgern kann. Pädiatrie Up2date 2013, 8, 227–253. [Google Scholar] [CrossRef] [Green Version]
- Bolk, J.; Fredriksson Kaul, Y.; Hellström-Westas, L.; Stjernqvist, K.; Padilla, N.; Serenius, F.; Hellgren, K.; Åden, U. National population-based cohort study found that visual-motor integration was commonly affected in extremely preterm born children at six-and-a-half years. Acta Paediatr. 2018, 107, 831–837. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karolis, V.R.; Froudist-Walsh, S.; Kroll, J.; Brittain, P.J.; Tseng, C.J.; Nam, K.; Reinders, A.A.T.S.; Murray, R.M.; Williams, S.C.R.; Thompson, P.M. Volumetric grey matter alterations in adolescents and adults born very preterm suggest accelerated brain maturation. Neuroimage 2017, 163, 379–389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Young, J.M.; Vandewouw, M.M.; Mossad, S.I.; Morgan, B.R.; Lee, W.; Smith, M.L.; Sled, J.G.; Taylor, M.J. White matter microstructural differences identified using multi-shell diffusion imaging in six-year-old children born very preterm. Neuroimage Clin. 2019, 23, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kelly, C.E.; Thompson, D.K.; Chen, J.; Leemans, A.; Adamson, C.L.; Inder, T.E.; Cheong, J.L.Y.; Doyle, L.W.; Anderson, P.J. Axon density and axon orientation dispersion in children born preterm. Hum. Brain Mapp. 2016, 37, 3080–3102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolke, D.; Baumann, N.; Busch, B.; Bartmann, P. Very preterm birth and parents’ quality of life 27 years later. Pediatrics 2017, 140, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Mulder, H.; Pitchford, N.J.; Marlow, N. Processing speed and working memory underlie academic attainment in very preterm children. Arch. Dis. Child Fetal Neonatal Ed. 2010, 95, F267–F272. [Google Scholar] [CrossRef]
- Blöte, A.W.; Hamstra-Bletz, L. A longitudinal study on the structure of handwriting. Percept. Mot. Skills 1991, 72, 983–994. [Google Scholar] [CrossRef]
- McHale, K.; Cermak, S.A. Fine motor activities in elementary school: Preliminary findings and provisional implications for children with fine motor problems. Am. J. Occup. Ther. 1992, 46, 898–903. [Google Scholar] [CrossRef] [Green Version]
- Perez-Roche, T.; Altemir, I.; Giménez, G.; Prieto, E.; González, I.; Peña -Segura, J.L.; Castillo, O.; Pueyo, V. Effect of prematurity and low birth weight in visual abilities and school performance. Res. Dev. Disabil. 2016, 59, 451–457. [Google Scholar] [CrossRef]
- Leung, M.P.; Thompson, B.; Black, J.; Dai, S.; Alsweiler, J.M. The effects of preterm birth on visual development. Clin. Exp. Optom. 2018, 101, 4–12. [Google Scholar] [CrossRef] [Green Version]
- Dadson, P.; Brown, T.; Stagnitti, K. Relationship between screen-time and hand function, play and sensory processing in children without disabilities aged 4-7 years: A exploratory study. Aust. Occup. Ther. J. 2020, 67, 297–308. [Google Scholar] [CrossRef] [PubMed]



| Very Preterm (n = 60) | Term (n = 60) | pa | |
|---|---|---|---|
| Clinical characteristics | |||
| Gestational age, weeks (range) | 28.7 (23.9–31.7) | 39.5 (38.0–42.0) | <0.001 |
| Birth weight, gram (range) | 1126.0 (430–1860) | 3414.3 (2380–4895) | <0.001 |
| Female, n | 30 | 30 | 1.0 |
| Follow-up characteristics | |||
| Age at assessment, years | 5.9 (0.3) | 5.9 (0.3) | 0.681 |
| Parental education (high, n (%)) | 36 (60) | 41 (68) | 0.341 |
| Visual perception, standard score | 8.8 (3.2) | 10.4 (2.8) | 0.004 |
| Fine motor skills, standard score | 7.1 (2.5) | 9.4 (2.0) | <0.001 |
| Visual-motor skills, standard score | 7.4 (2.3) | 9.6 (1.8) | <0.001 |
| Visual Perception | Fine Motor Skills | Visual-Motor Skills | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | 95% CI | β | p | b | 95% CI | β | p | b | 95% CI | β | p | |
| Step 1 | ||||||||||||
| Very preterm | −1.60 | −2.68 to −0.52 | −0.26 | 0.004 | −2.23 | −3.06 to −1.40 | −0.44 | <0.001 | −2.24 | −2.99 to −1.49 | −0.48 | <0.001 |
| Total R2 | 0.07 | 0.20 | 0.23 | |||||||||
| Step 2 | ||||||||||||
| Very preterm | −1.53 | −2.61 to −0.45 | −0.25 | 0.006 | −2.19 | −3.02 to −1.37 | −0.44 | <0.001 | −2.17 | −2.91 to −1.43 | −0.46 | <0.001 |
| Female | −0.11 | −1.21 to 0.99 | −0.02 | 0.841 | 0.59 | −0.26 to 1.42 | 0.12 | 0.170 | −0.10 | −0.86 to 0.66 | −0.02 | 0.793 |
| Education high | 0.85 | −0.30 to 2.00 | 0.13 | 0.147 | 0.45 | −0.43 to 1.33 | 0.09 | 0.316 | 0.91 | 0.12 to 1.70 | 0.19 | 0.025 |
| Total R2 (∆ R2) a | 0.09 * (0.02) | 0.21 *** (0.02) | 0.27 *** (0.04) | |||||||||
| Very Preterm | Term | Unadjusted OR (95% CI) | Adjusted OR a (95% CI) | |
|---|---|---|---|---|
| Visual perception | 23.3 | 8.3 | 3.35 (1.12–9.99) | 3.45 (1.12–10.64) |
| Fine motor skills | 45.0 | 11.7 | 6.20 (2.43–15.83) | 6.24 (2.42–16.04) |
| Visual-motor skills | 46.7 | 6.7 | 12.25 (3.94–38.08) | 13.48 (4.13–44.00) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dathe, A.-K.; Jaekel, J.; Franzel, J.; Hoehn, T.; Felderhoff-Mueser, U.; Huening, B.M. Visual Perception, Fine Motor, and Visual-Motor Skills in Very Preterm and Term-Born Children before School Entry–Observational Cohort Study. Children 2020, 7, 276. https://doi.org/10.3390/children7120276
Dathe A-K, Jaekel J, Franzel J, Hoehn T, Felderhoff-Mueser U, Huening BM. Visual Perception, Fine Motor, and Visual-Motor Skills in Very Preterm and Term-Born Children before School Entry–Observational Cohort Study. Children. 2020; 7(12):276. https://doi.org/10.3390/children7120276
Chicago/Turabian StyleDathe, Anne-Kathrin, Julia Jaekel, Julia Franzel, Thomas Hoehn, Ursula Felderhoff-Mueser, and Britta M. Huening. 2020. "Visual Perception, Fine Motor, and Visual-Motor Skills in Very Preterm and Term-Born Children before School Entry–Observational Cohort Study" Children 7, no. 12: 276. https://doi.org/10.3390/children7120276