Published online Feb 21, 2014. doi: 10.3748/wjg.v20.i7.1882
Revised: December 9, 2013
Accepted: December 12, 2013
Published online: February 21, 2014
We report here a case of pancreatic pseudocystocolic fistula that was treated without surgical or endoscopic intervention. A 76-year-old woman, presenting with a fever and epigastric pain, was referred to our institution. Three months prior to this admission, the patient had been admitted to the hospital for acute pancreatitis. Abdominal computerized tomography (CT) revealed a 9 cm pseudocyst containing air, and a fistular opening was observed via colonoscopy. After colonoscopy, the abdominal pain was slightly improved, the fever subsided and laboratory results showed decreased C-reactive protein levels. The observed improvement was likely due to the cleansing of the bowel, which induced spontaneous drainage from the pseudocyst into the colon. Antibiotic therapy was administered and daily bowel cleansing was performed using a polyethylene glycol solution. After three weeks, a follow-up CT revealed that the size of the pseudocyst had decreased significantly from 9 to 5.3 cm. In addition, laboratory tests were improved. The patient was able to resume a normal diet and was discharged in good overall health from the hospital, without aggravation of the symptoms. A colonoscopy performed 3 mo later and a follow-up CT performed 6 mo later confirmed that both the fistula and pseudocyst had completely disappeared.
Core tip: We present the case of a 76-year-old female who was admitted to our institution with epigastric pain and a fever. Abdominal computed tomography and colonoscopy revealed a pseudocystocolic fistula. The patient was treated with antibiotics and bowel cleansing was administered using a polyethylene glycol solution. Induction of spontaneous drainage into the colon, through bowel cleansing, can treat small pseudocystocolic fistulas.
- Citation: Kwon JC, Kim BY, Kim AL, Kim TH, Park MI, Jung HJ, Lim JH, Jung JK, Kim HS, Lee DW. Pancreatic pseudocystocolonic fistula treated without surgical or endoscopic intervention. World J Gastroenterol 2014; 20(7): 1882-1886
- URL: https://www.wjgnet.com/1007-9327/full/v20/i7/1882.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i7.1882
The clinical manifestation of acute pancreatitis can range from mild to severe. Most cases of acute pancreatitis are mild and improve within a few days. However, severe acute pancreatitis can lead to localized complications such as the formation of a pseudocyst, necrosis or an abscess, but it can also cause systemic complications, such as multi-organ failure or death. In acute pancreatitis complications, colonic involvement has a relatively low incidence of approximately 3%[1]. Colonic complications range from a localized pseudo-obstruction of the ileus to necrosis, hemorrhage, ischemic colitis and fistula formation[2]. Pseudocystocolic fistula formation is especially dangerous when it induces massive lower gastrointestinal bleeding and sepsis, which require rapid diagnoses and appropriate treatments[3]. Pseudocystocolic fistulas have primarily been treated by surgery, but many successful cases of nonsurgical intervention have recently been reported[4-6]. Here, we present a unique case of a patient with acute pancreatitis and a comorbid pseudocystocolic fistula complication that was treated without any surgical or endoscopic intervention. The treatment and a literature review are reported here.
A 76-year-old female patient arrived at the emergency department of our hospital with severe epigastric pain lasting for 3 d. With the exception of maintenance drugs for insulin-independent diabetes mellitus and hypertension, which she had been taking for approximately 20 years, the patient had not taken any medications at the time of admission. The patient had no history of alcohol abuse. When she was admitted, the patient’s blood pressure was 112/68 mmHg, her pulse rate was 86 beats/min, her respiratory rate was 23 breaths/min, and she had a body temperature of 38.0 °C.
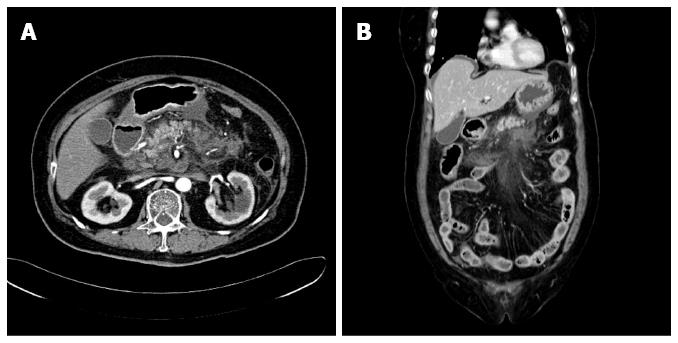
An examination of peripheral blood at the time of admission yielded the following values: white blood cell (WBC) count of 20740/mm3 (neutrophils: 92.1%); hemoglobin: 15.5 g/dL; C-reactive protein (CRP): 30.52 mg/dL; total bilirubin: 3.84 mg/dL; aspartate aminotransferase (AST): 201 U/L; alanine aminotransferase (ALT): 201 U/L; alkaline phosphatase: 127 IU/L; r-glutamyltranspeptidase: 403 IU/L; amylase: 178 U/L; lipase: 186 U/L; triglyceride: 149 mg/dL; and calcium: 10.0 mg/dL. Abdominal computerized tomography (CT) revealed extensive accumulation of extrapancreatic fluid along with peripancreatic fatty infiltration, which is typical of grade E pancreatitis, according to the Balthazar classification system (Figure 1). Because AST and ALT levels were markedly elevated, endoscopic retrograde cholangiopancreatography (ERCP) was performed for suspected gallstone pancreatitis, despite the fact that gallstones were not observed in the CT image[7]. After endoscopic sphincterotomy and nasobiliary drainage, a plastic stent (5 Fr, 3 cm) was inserted into the pancreatic duct. Seven days after the procedure, the patient no longer complained of abdominal pain and had good overall health. Cholecystectomy was recommended to prevent recurrence, but the patient refused surgical intervention and was subsequently discharged.
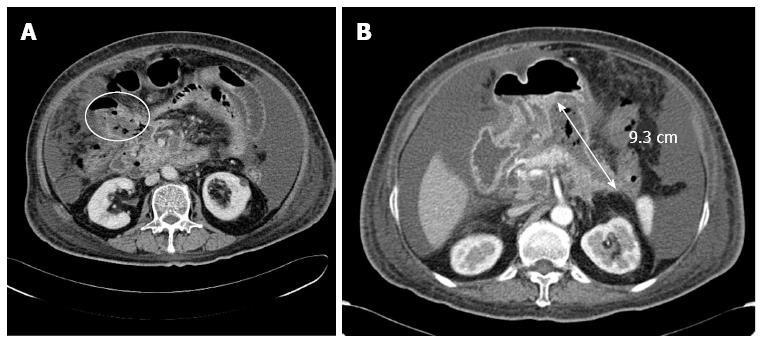
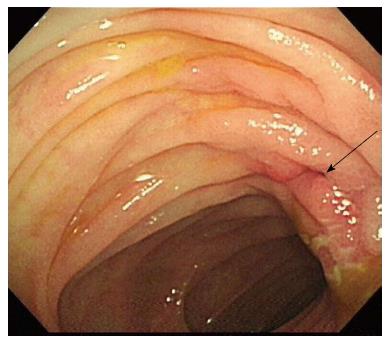
Approximately 3 mo after the previous discharge, the patient presented to the hospital again with a 2-wk history of epigastric pain and a mild fever (37.5 °C). Laboratory results showed a WBC count of 9820/mm3 (neutrophils: 74.1%) and a CRP level of 10.27 mg/dL. Amylase, lipase, and other liver function test results were within the normal ranges. An abdominal CT showed an approximately 9.3 cm long pseudocyst that contained air. The presence of air led us to suspect the presence of a fistula on the right side of the colon (Figure 2). A colonoscopy was thus performed to determine if a fistula was present and assess the outcome of the antibiotic treatment. A fistula opening was found in the hepatic flexure (Figure 3). Two days after the colonoscopy, the patient’s fever was reduced. Blood laboratory results showed improvements, with decreased CRP levels. The patient’s pain was greatly reduced without requiring any invasive treatment or additional oral medications. The antibiotic treatment was continued. To maintain a clean colon and induce colonic drainage of the pseudocyst, a bowel-cleansing regimen was implemented using a polyethylene glycol (PEG) solution. A liter of PEG solution was administered orally every morning and afternoon after which the patient was monitored for the number of bowel movements. If two or less bowel movements were observed, an additional half-liter of the PEG solution was administered in the evening.
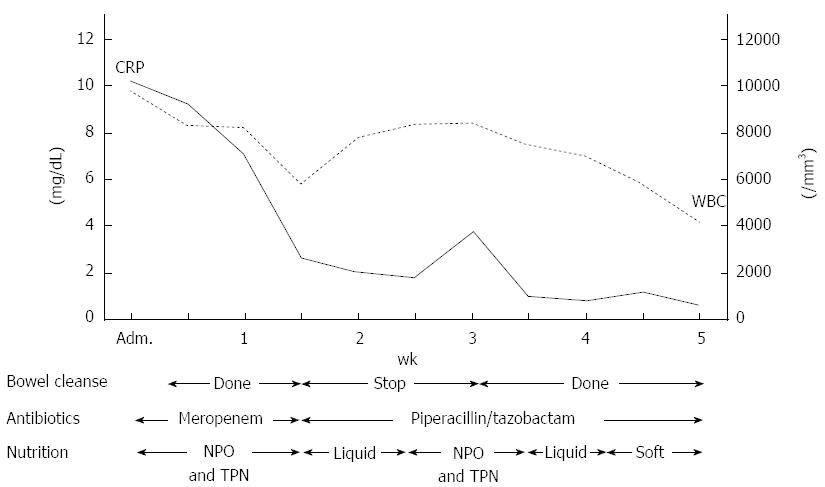
After the bowel cleansing treatment, the patient was put on a liquid diet. However, she complained of abdominal pain again and blood tests revealed an increased WBC count and CRP level (Figure 4). A follow-up CT scan showed that although the size of the pseudocyst was reduced to approximately 5.3 cm, air was still present inside. Thus, fasting and the bowel-cleansing regimen were continued for an additional 3 wk.
After the 3 wk, the patient resumed a normal diet and was discharged from the hospital in good health, without aggravation of the symptoms. After 3 mo, a follow-up colonoscopy confirmed complete disappearance of the fistula. After 6 mo, a CT confirmed the complete disappearance of the pseudocyst. The patient is currently under outpatient follow-up with subclinical conditions.
A pseudocyst, a complication of acute pancreatitis, tends to rupture in the abdominal cavity or form a fistula in the gastrointestinal tract. Pseudocysts occur most frequently in the stomach, accounting for approximately one-third of all cases, followed by the colon and duodenum[8]. The mechanism underlying fistula formation is thought to be due to elevated internal pressure from fluid accumulation within the pseudocyst and proteolytic enzymes within the fluid that invade adjacent organs or vessels, inducing ischemic changes that enable penetration of the walls of the most vulnerable organs and formation of a fistula[8]. Most pseudocystoenteric fistulas that form in the upper gastrointestinal tract can be treated conservatively and have a relatively good prognosis. In contrast, fistulas that form in the colon rarely heal spontaneously and tend to be associated with fatal complications, with a reported mortality of approximately 17%-67%[9,10]. Such poor prognosis can be attributed to the high possibility of bleeding or sepsis induced by necrosis in peripancreatic tissues and vessels caused by activated pancreatic enzymes mediated by bacteria in the colon[3].
A CT colonography, performed with water-soluble contrast agents, is a relatively safe and conventional method to diagnose pseudocystocolic fistulas[1]. However, because colonography has low sensitivity in detecting a fistulous tract compared with ERCP, it is no longer widely used[11]. Diagnosis can also be achieved using a radiograph obtained after contrast agent injection via a nasocystic drainage catheter or percutaneous catheter inserted for pseudocyst drainage[10,12]. With the recent advent of medical imaging technologies, noninvasive radiologic modalities, such as abdominal CT or magnetic resonance imaging, have also been used for diagnosis[10,13]. In the present case, the final diagnosis was made based on colonoscopic findings under the impression of a pseudocyst-associated fistula in the right side of the colon, as determined by a 64-channel multidetector CT.
In the past, surgical interventions, such as debridement, wide drainage or externalization of the fistula via a temporary colostomy, were the treatment of choice for pseudocystocolic fistulas[5]. Recent reports, however, have described cases where large fistulas were successfully treated using endoscopic tools, such as an endoloop, clips, and fibrin glue[6], or fibrin glue alone to treat small fistulas[14]. Indications for such nonsurgical treatments have not yet been clearly established. Although endoscopic treatments are considered for patients with well-defined pseudocysts that have been complicated by infection, close follow-up and repetitive interventions may be needed and surgical treatments are recommended when sepsis cannot be controlled[5]. Because the patient in the case described herein had a well-defined pseudocyst with non-life-threatening conditions and a small fistula opening, we chose to treat the patient with a PEG solution. The patient’s symptoms and laboratory findings improved after administration of the PEG solution during the colonoscopy. The bowel-cleansing regimen was continued alongside antibiotic therapy without the need for any invasive treatment.
Complete recovery of a pseudocystocolic fistula can be confirmed by the disappearance of the pseudocyst and fistula with a follow-up CT scan and improved clinical symptoms in the patient[4-6,12]. In this case, the complete disappearance of the fistula was confirmed by follow-up colonoscopy performed 3 mo after treatment. The disappearance of the pseudocyst was confirmed by CT imaging, 6 mo after the patient was admitted.
The present case indicates that when the fistula size is small and the patient’s overall health status is good, a pseudocystocolic fistula can be treated by inducing spontaneous drainage to the colon through a bowel-cleansing regimen, without additional surgical intervention or fistula closure.
A 76-year-old female, previously hospitalized for gallstones and pancreatitis 3 mo prior, complained of epigastric pain and fever.
The patient was diagnosed with a large pseudocyst with a fistula in the right side of the colon.
Abdominal computerized tomography (CT) was performed to identify the cause of the pain and fever.
Elevated C-reactive protein was seen in the laboratory results, suggesting an acute inflammatory condition.
Pseudocyst and fistula in the right of the side colon was seen in an abdominal CT and a fistular opening at the hepatic flexure was confirmed with the colonoscope.
Antibiotics were given to treat the systemic inflammation and polyethylene glycol was administered for colon cleansing.
Two previous reports by Will et al and Karvonen et al showed treatment of a pseudocystocolic fistula using an endoscopic method.
In patients with good overall health and a small fistula size, a pseudocystocolic fistula can be treated by inducing spontaneous drainage to the colon through bowel cleansing, without additional surgical intervention or fistula closure.
This case report by Kwon et al of a 76-year-old woman presented with acute pancreatitis and as a complication pseudocysttocolic fistula was successfully treated with antibiotics and 3-wk bowel cleansing using polyethylene glycol solution. The disappaearance of the pseudocyst and fistula was confirmed by abdominal CT scan and colonoscopy.
P- Reviewers: Said SAM, Sumi S S- Editor: Song XX L- Editor: A E- Editor: Wang CH
| 1. | Mohamed SR, Siriwardena AK. Understanding the colonic complications of pancreatitis. Pancreatology. 2008;8:153-158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 2. | De Backer AI, Mortelé KJ, Vaneerdeweg W, Ros PR. Pancreatocolonic fistula due to severe acute pancreatitis: imaging findings. JBR-BTR. 2001;84:45-47. [PubMed] [Cited in This Article: ] |
| 3. | Santos JC, Feres O, Rocha JJ, Aracava MM. Massive lower gastrointestinal hemorrhage caused by pseudocyst of the pancreas ruptured into the colon. Report of two cases. Dis Colon Rectum. 1992;35:75-77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Wolfsen HC, Kozarek RA, Ball TJ, Patterson DJ, Traverso LW, Freeny PC. Pancreaticoenteric fistula: no longer a surgical disease? J Clin Gastroenterol. 1992;14:117-121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Howell DA, Dy RM, Gerstein WH, Hanson BL, Biber BP. Infected pancreatic pseudocysts with colonic fistula formation successfully managed by endoscopic drainage alone: report of two cases. Am J Gastroenterol. 2000;95:1821-1823. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Will U, Meyer F, Hartmeier S, Schramm H, Bosseckert H. Endoscopic treatment of a pseudocystocolonic fistula by band ligation and endoloop application: case report. Gastrointest Endosc. 2004;59:581-583. [PubMed] [Cited in This Article: ] |
| 7. | Tenner S, Dubner H, Steinberg W. Predicting gallstone pancreatitis with laboratory parameters: a meta-analysis. Am J Gastroenterol. 1994;89:1863-1866. [PubMed] [Cited in This Article: ] |
| 8. | Shatney CH, Sosin H. Spontaneous perforation of a pancreatic pseudocyst into the colon and duodenum. Am J Surg. 1973;126:433-438. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 33] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Wille-Jørgensen P, Frederiksen HJ. Colonic necrosis or fistula following pancreatitis or gastric surgery. Eur J Surg. 1991;157:137-139. [PubMed] [Cited in This Article: ] |
| 10. | Suzuki A, Suzuki S, Sakaguchi T, Oishi K, Fukumoto K, Ota S, Inaba K, Takehara Y, Sugimura H, Uchiyama T. Colonic fistula associated with severe acute pancreatitis: report of two cases. Surg Today. 2008;38:178-183. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Shim KS, Suh JM, Yang YS, Choi JY, Park YH. Three-dimensional demonstration and endoscopic treatment of pancreaticoperitoneal fistula. Am J Gastroenterol. 1993;88:1775-1779. [PubMed] [Cited in This Article: ] |
| 12. | Urakami A, Tsunoda T, Hayashi J, Oka Y, Mizuno M. Spontaneous fistulization of a pancreatic pseudocyst into the colon and duodenum. Gastrointest Endosc. 2002;55:949-951. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Tüney D, Altun E, Barlas A, Yegen C. Pancreatico-colonic fistula after acute necrotizing pancreatitis. Diagnosis with spiral CT using rectal water soluble contrast media. JOP. 2008;9:26-29. [PubMed] [Cited in This Article: ] |
| 14. | Karvonen J, Gullichsen R, Salminen P, Grönroos JM. Endoscopic treatment of pseudocystocolonic fistula with fibrin glue. Gastrointest Endosc. 2010;72:664-665. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |