Published online Jul 7, 2008. doi: 10.3748/wjg.14.4087
Revised: April 16, 2008
Accepted: April 23, 2008
Published online: July 7, 2008
Takayasu’s arteritis and Crohn’s disease are chronic inflammatory diseases of uncertain aetiology. They rarely occur together, with only twenty nine cases of co-existent Takayasu’s arteritis and Crohn’s disease reported in the literature. In 88% of these cases, Takayasu’s arteritis was diagnosed simultaneously or following a diagnosis of Crohn’s disease. We present a case of a young Caucasian medical student, incidentally found to have bilateral carotid bruits on auscultation by a colleague. Magnetic resonance angiography revealed stenoses of the common carotid arteries with established collaterals, and a diagnosis of Type 1 Takayasu’s arteritis was made. An 18F-fluorodeoxyglucose positron emission tomography scan revealed no active disease. Nine months later, she presented with a short history of abdominal pain, vomiting and abdominal distension. Barium follow-through and computer tomography revealed a terminal ileal stricture and proximal small bowel dilation. An extended right hemicolectomy was performed and histopathology supported a diagnosis of Crohn’s disease. This case report is presented with a particular focus on the temporal relationship between these two disease processes and explores whether their concurrence is more than just co-incidence.
- Citation: Farrant MA, Mason JC, Wong NA, Longman RJ. Takayasu’s arteritis following Crohn’s disease in a young woman: Any evidence for a common pathogenesis? World J Gastroenterol 2008; 14(25): 4087-4090
- URL: https://www.wjgnet.com/1007-9327/full/v14/i25/4087.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.4087
Takayasu’s arteritis is a granulomatous panarteritis affecting large vessels, namely the aorta and its main branches, pulmonary and coronary arteries. It is characterised by stenotic and, occasionally, aneurysmal lesions. Manifestations of the disease range from no symptoms, to bruits, hypertension, cerebrovascular events, congestive heart failure and blindness[1]. Takayasu’s arteritis classically progresses through three stages, namely a systemic non-vascular phase, a vascular inflammatory phase and a quiescent “burnt out” phase[1]. First described by Yamamoto in 1830[1], the disease has a worldwide distribution, although it is most commonly diagnosed in young women of Asian decent. The incidence in North America has been estimated at 2.6 cases per million[2].
Crohn’s disease is a chronic, relapsing, transmural inflammatory disease, affecting primarily the gastrointestinal mucosa. The incidence of Crohn’s disease is approximately 2 in 100 000, and its prevalence is 50 in 100 000[3], with geographical and ethnic variation, most commonly seen in Caucasian populations. There is a slight female preponderance, with a peak onset of disease around 20 years of age, with another peak occurring between 50 and 70 years of age[4].
Both Takayasu’s arteritis and Crohn’s disease are chronic granulomatous inflammatory processes involving different target organs, namely large elastic arteries and the gastrointestinal tract respectively. They may coexist and in 29 reported cases, Crohn’s disease preceded Takayasu’s arteritis in 88% cases, raising the possibility that it could be regarded as an extraintestinal manifestation of Crohn’s disease. In contrast, herein we present a rare case of Crohn’s disease in a patient with clinically inactive Takayasu’s arteritis.
A 24-year-old Caucasian medical student was found incidentally to have bilateral carotid bruits whilst practising for final clinical examinations. Her past medical history was unremarkable. Physical examination revealed normal peripheral pulses, equal normal blood pressure in both arms and no cardiac murmurs. A C-reactive protein of 13 mg/L, haemoglobin of 11.8 g/dL and a plasma viscosity of 1.73 mmHg were recorded.
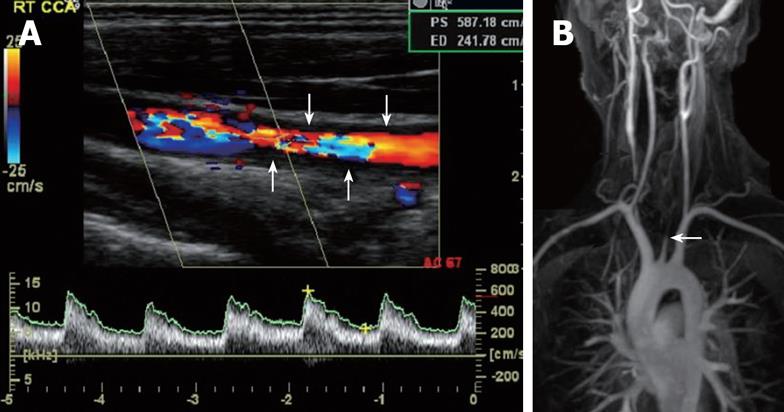
A duplex scan showed thickening of the proximal common carotid with severe stenoses in the mid common carotid arteries bilaterally (Figure 1A). Reduced internal carotid flow was compensated by retrograde flow in both external carotid arteries. Gadolinium-enhanced magnetic resonance angiography confirmed these findings along with a normal aortic arch, prominent bilateral vertebral arteries, mild irregularity in the right subclavian artery and collaterals feeding both external carotid arteries (Figure 1B). These findings led to the diagnosis of TypeITakayasu’s arteritis[1]. Subsequent echocardiography confirmed the absence of aortic regurgitation and computer tomography-angiography of the subdiaphragmatic aorta was unremarkable. A normal full body 18F-fluorodeoxyglucose positron emission tomography (18F-FDG-PET) scan revealed no active disease.
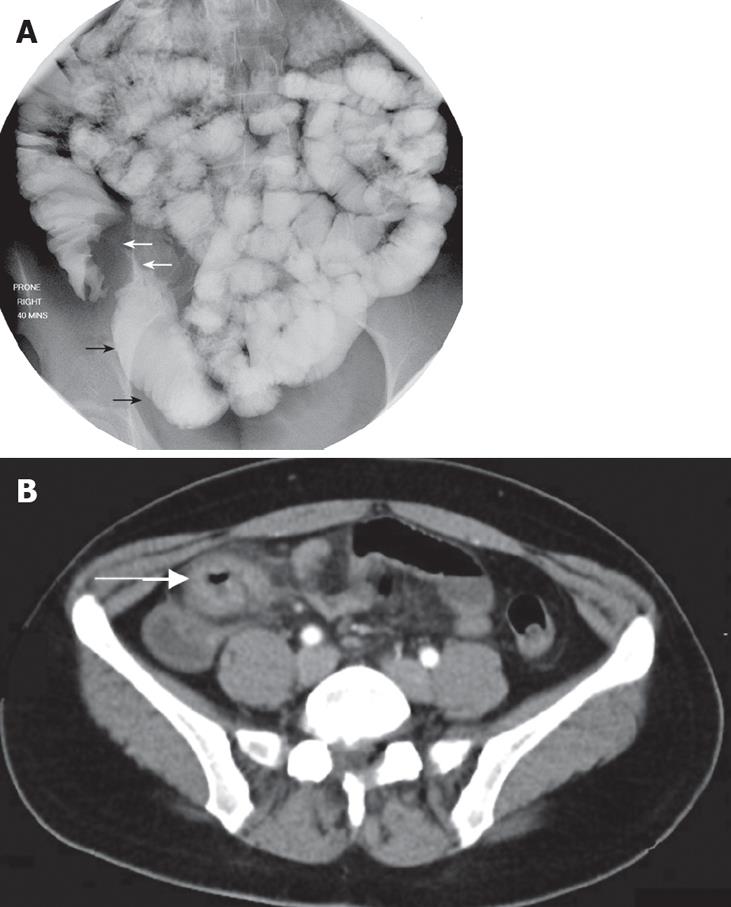
Nine months later, she presented with a short history of colicky abdominal pain, vomiting and abdominal distension. Barium studies and a computer tomography scan revealed a terminal ileal stricture and proximal small bowel dilation (Figure 2). At operation, the obstructing lesion was found to have extended to the ileocaecal valve with tethering to the proximal transverse colon. A laparoscopic extended right hemicolectomy was performed with a primary anastomosis, from which a full recovery was made and the patient remains symptom free.
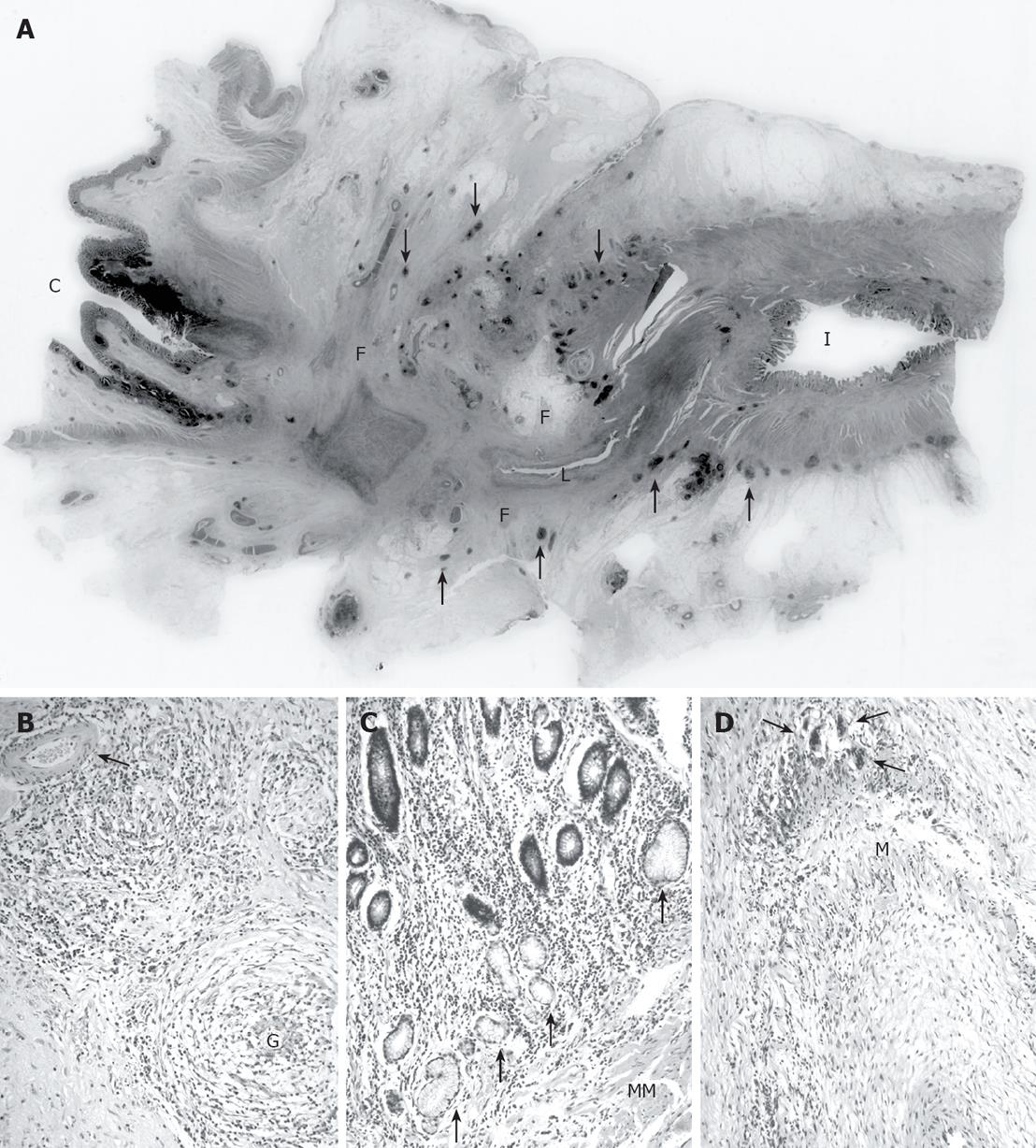
The resected specimen showed a three-centimetre long stricture at the distal ileum extending to the ileocaecal valve (Figure 3A), and the strictured bowel had a thickened wall with fat wrapping. Along the stricture, the small bowel mucosa was replaced by intensely inflamed granulation tissue and inflamed transmural fibrous tissue focally replaced the muscularis propria (Figure 3A). Within this tissue, there were scattered medium-sized blood vessels showing intramural chronic inflammation with focal obliteration. In addition, one blood vessel showed a cluster of multinucleated giant cells along the outer edge of the media (Figure 3D). However, the majority of similarly-sized vessels at and around the stricture and the ileocolic artery were normal. The ileum just proximal to the stricture showed focal ulceration, transmural chronic inflammation and ulcer-associated cell lineage (also known as gastric pyloric gland metaplasia) (Figure 3C). Well-formed granulomas were present in the caecal submucosa just distal to the stricture and in the subserosal tissues surrounding the stricture (Figure 3B). The presence of a fistula connecting the stricture to the transverse colon was confirmed histologically. Seventeen lymph nodes harvested showed reactive changes only, with no evidence of granulomas. Several features of this specimen strongly support a diagnosis of Crohn’s disease. The stricture occurred at a site classically affected by Crohn’s disease, and showed several characteristic features of this disease, namely fat wrapping, fistula formation, transmural fibrosis and inflammation, multiple granulomas (which could not be attributed to crypt rupture or extravasated intestinal contents), and widespread adjacent ulcer-associated cell lineage. By contrast, there was no evidence that Takayasu’s arteritis directly caused the ileal stricture and inflammation. Takayasu’s arteritis is a vasculitis of large vessels. If the arteritis involved a large vessel supplying the abnormal terminal ileum, namely the superior mesenteric artery or its proximal branches, the most likely intestinal manifestation would have been infarction, and a much longer segment of bowel. The largest blood vessel included in the resection specimen (i.e. the ileocolic artery) did not show vasculitis. In fact, the only abnormal vessels seen were occasionally inflamed and focally occluded medium-sized arteries around the stricture, and even these were more likely to represent endarteritis obliterans secondary to the inflammation. Finally, ‘granulomatous vasculitis’, as was seen in one medium-sized artery beside the stricture, is a recognised feature of Crohn’s disease.
Co-existence of Takayasu’s arteritis and Crohn’s disease has previously been reported in 29 cases. The expected prevalence of Crohn’s disease in patients with Takayasu’s arteritis, if present by chance alone, is approximately 0.05%-0.2%[3]. Thus, it has been suggested that this unexpected association is more than just a coincidence. The epidemiology, aetiology and pathogenesis of these two diseases point to a role of both environmental and hereditary factors, interacting to trigger the inflammatory process.
Takayasu’s arteritis and Crohn’s disease present more commonly in young females, suggesting a potential hormonal influence. To this end, the oral contraceptive pill has been reported, somewhat controversially, to increase the risk of Crohn’s disease[4]. Geographically, Takayasu’s arteritis is common in Japan, Korea and India, whereas Crohn’s disease has a much higher prevalence in Northern Europe and North America[14]. Such ethnic predilection has led to the investigation of human leucocyte antigens (HLA) in the pathophysiology. However, to date no common HLA genotype links these two disease processes. Likewise infectious agents have been implicated. In particular, mycobacterium tuberculosis (MTB) or autoimmunity evoked by this micro-organism. Although increased reactivity to, and circulating antibodies against mycobacterium heat shock protein, 65 have been identified in Takayasu’s arteritis and Crohn’s disease patients, there is no convincing evidence for a role of MTB in the pathogenesis[56].
Cell-mediated immunological mechanisms play an important role in both diseases. In Takayasu’s arteritis, autoantibodies against aortic endothelial cells may contribute to vascular dysfunction by increasing local cytokine synthesis, cellular adhesion molecule expression and endothelial cell apoptosis[7]. Pro-inflammatory cytokines such as tumour necrosis factor (TNF) α, interleukin (IL)-6, IL-8, IL-12 and IL-18, are common to both, amplifying the inflammatory process[78]. Moreover, the anti-TNFα monoclonal antibody infliximab is an effective therapeutic agent for both Takayasu’s arteritis and Crohn’s disease, suggesting the presence of common inflammatory pathways[37]. Wakefield et al[9] have found evidence of granulomatous vasculitis, also present in our case, in 15 out of 24 patients when examining resected intestine from patients with Crohn’s disease. Granulomatous inflammation is also seen in Takayasu’s arteritis[10]. Despite these similarities, the question of why the arch of the aorta is the predominant site of tissue injury in Takayasu’s arteritis, and the bowel wall in Crohn’s disease remains to be answered.
In our patient, Takayasu’s arteritis was asymptomatic and the presence of established collaterals, a negative 18F-FDG-PET scan and no MRA evidence for vascular wall inflammation, suggested that the peak activity was present some years ago. Thus, Crohn’s disease appears to have presented apparently independent of Takayasu’s arteritis. It was reported that only 3 of 24 previous cases with known details have Takayasu’s arteritis preceded Crohn’s disease[311–17]. An association between the conditions may simply reflect two diseases typically presenting in the same age group. However, a shared common cause resulting in a granulomatous vasculitis and end organ damage remains a possible explanation.
In summary, the temporal relationship between Takayasu’s arteritis and Crohn’s disease remains of interest, with the majority of cases presenting initially with Crohn’s disease. Possible explanations for their association have been explored. However, no data can confirm an aetiological link between the two diseases. We present an interesting case of Crohn’s disease arising in a patient apparently some years after Takayasu’s arteritis, as indicated by the established carotid arterial collaterals. As the active phase of Takayasu’s arteritis may be relatively short, and the disease can ‘burn out’, many cases may go undetected, as would this case had it not been for the astute medical student.
| 1. | Johnston SL, Lock RJ, Gompels MM. Takayasu arteritis: a review. J Clin Pathol. 2002;55:481-486. [Cited in This Article: ] |
| 2. | Hall S, Barr W, Lie JT, Stanson AW, Kazmier FJ, Hunder GG. Takayasu arteritis. A study of 32 North American patients. Medicine (Baltimore). 1985;64:89-99. [Cited in This Article: ] |
| 3. | Reny JL, Paul JF, Lefebvre C, Champion K, Emmerich J, Bletry O, Piette JC, Fiessinger JN. Association of Takayasu's arteritis and Crohn's disease. Results of a study on 44 Takayasu patients and review of the literature. Ann Med Interne (Paris). 2003;154:85-90. [Cited in This Article: ] |
| 4. | Karlinger K, Gyorke T, Mako E, Mester A, Tarjan Z. The epidemiology and the pathogenesis of inflammatory bowel disease. Eur J Radiol. 2000;35:154-167. [Cited in This Article: ] |
| 5. | Kumar Chauhan S, Kumar Tripathy N, Sinha N, Singh M, Nityanand S. Cellular and humoral immune responses to mycobacterial heat shock protein-65 and its human homologue in Takayasu’s arteritis. Clin Exp Immunol. 2004;138:547-553. [Cited in This Article: ] |
| 6. | Szewczuk MR, Depew WT. Evidence for T lymphocyte reactivity to the 65 kilodalton heat shock protein of mycobacterium in active Crohn's disease. Clin Invest Med. 1992;15:494-505. [Cited in This Article: ] |
| 7. | Seko Y. Giant cell and Takayasu arteritis. Curr Opin Rheumatol. 2007;19:39-43. [Cited in This Article: ] |
| 8. | Pallone F, Monteleone G. Mechanisms of tissue damage in inflammatory bowel disease. Curr Opin Gastroenterol. 2001;17:307-312. [Cited in This Article: ] |
| 9. | Wakefield AJ, Sankey EA, Dhillon AP, Sawyerr AM, More L, Sim R, Pittilo RM, Rowles PM, Hudson M, Lewis AA. Granulomatous vasculitis in Crohn’s disease. Gastroenterology. 1991;100:1279-1287. [Cited in This Article: ] |
| 10. | Noris M. Pathogenesis of Takayasu’s arteritis. J Nephrol. 2001;14:506-513. [Cited in This Article: ] |
| 11. | Baqir M, Usman MH, Adenwalla HN, Aziz S, Noor F, ul- Islam T, Ahmed M, Hotiana M. Takayasu's arteritis with skin manifestations in a patient with inflammatory bowel disease: coincidence or concurrence? Clin Rheumatol. 2007;26:996-998. [Cited in This Article: ] |
| 12. | De Simone M, Cioffi U, Quatrini M, Lemos A, Ciulla M, Botti F, Carrara A, Marconato R, Contessini Avesani E. Crohn’s disease and Takayasu’s arteritis: is this association difficult to find out? Minerva Gastroenterol Dietol. 2006;52:441-443. [Cited in This Article: ] |
| 13. | Fry LC, Rickes S, Monkemuller K, Malfertheiner P. [Crohn's disease associated with Takayasu's arteritis]. Acta Gastroenterol Latinoam. 2005;35:238-242. [Cited in This Article: ] |
| 14. | Biagi P, Castro R, Campanella G, Parisi G, Gobbini AR, Vedovini G. Takayasu's arteritis and Crohn's disease: an unusual association. Report on two cases. Dig Liver Dis. 2001;33:487-491. [Cited in This Article: ] |
| 15. | Levitsky J, Harrison JR, Cohen RD. Crohn's disease and Takayasu's arteritis. J Clin Gastroenterol. 2002;34:454-456. [Cited in This Article: ] |
| 16. | Enc F, Yorulmaz E, Pehlivanoglu V, Tuncer I, Kiziltas S, Erbahceci A. Takayasu's arteritis in a case diagnosed as Crohn's disease. Turk J Gastroenterol. 2007;18:250-253. [Cited in This Article: ] |
| 17. | Daryani NE, Habibi AN, Bashashati M, Keramati MR, Rafiee MJ, Ajdarkosh H, Azmi M. Takayasu’s arteritis associated with Crohn’s disease: a case report. J Med Case Reports. 2008;2:87. [Cited in This Article: ] |