Published online May 7, 2005. doi: 10.3748/wjg.v11.i17.2570
Revised: August 22, 2004
Accepted: October 18, 2004
Published online: May 7, 2005
AIM: There is some evidence of functional superiority of colonic J-pouch over straight coloanal anastomosis (CAA) in ultralow anterior resection (ULAR) or intersphincteric resection. On the assumption that colonic J-pouch anal anastomosis is superior to straight CAA in ULAR with upper sphincter excision (USE: excision of the upper part of the internal sphincter) for low-lying rectal cancer, we compare functional outcome of colonic J-pouch vs the straight CAA.
METHODS: Fifty patients of one hundred and thirty-three rectal cancer patients in whom lower margin of the tumors were located between 3 and 5 cm from the anal verge received ULAR including USE from September 1998 to January 2002. Patients were randomized for reconstruction using either a straight (n = 26) or a colonic J-pouch anastomosis (n = 24) with a temporary diverting-loop ileostomy. All patients were followed-up prospectively by a standardized questionnaire [Fecal Inco-ntinence Severity Index (FISI) scores and Fecal Incontinence Quality of Life (FIQL) scales].
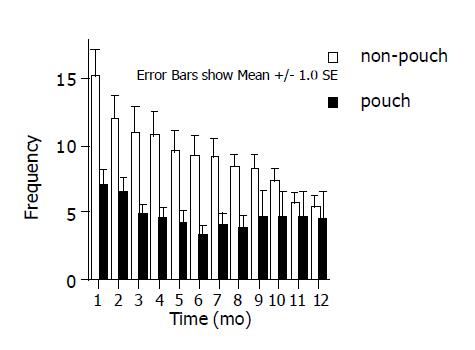
RESULTS: We found that, compared to straight anastomosis patients, the frequency of defecation was significantly lower in J-pouch anastomosis patients for 10 mo after ileostomy takedown. The FISI scores and FIQL scales were significantly better in J-pouch patients than in straight patients at both 3 and 12 mo after ileostomy takedown. Furthermore, we found that FISI scores highly correlated with FIQL scales.
CONCLUSION: This study indicates that colonic J-pouch anal anastomosis decreases the severity of fecal incontinence and improves the quality of life for 10 mo after ileostomy takedown in patients undergoing ULAR with USE for low-lying rectal cancer.
- Citation: Park JG, Lee MR, Lim SB, Hong CW, Yoon SN, Kang SB, Heo SC, Jeong SY, Park KJ. Colonic J-pouch anal anastomosis after ultralow anterior resection with upper sphincter excision for low-lying rectal cancer. World J Gastroenterol 2005; 11(17): 2570-2573
- URL: https://www.wjgnet.com/1007-9327/full/v11/i17/2570.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i17.2570
The incidence of colorectal cancer has increased 200% from the 1980s to the year 2000 in Korea[1]. Advances in stapling technology have allowed restoration of bowel continuity after resection of low-lying rectal cancers. In some lower rectal cancers, for which the DS technique is not feasible, coloanal anastomosis (CAA) has been used to achieve bowel continuity[2]. However, efforts to preserve the sphincter muscle may compromise the application of a classical CAA. Several groups have attempted partial excision of the upper part of the internal sphincter muscle to achieve a tumor-free resection margin, thereby increasing the application for using CAA[3-6].
A further problem in resection of low-lying rectal cancers is the so-called anterior resection syndrome, which is characterized by functional problems related to defecation. To solve this problem, Lazorthes et al, and Parc et al, designed a J-shaped colonic pouch which reportedly reduced the severity of the syndrome[7,8]. As a result, the colonic J-pouch has been widely used in treatments involving anastomosis following ultralow anterior resection (ULAR) for low-lying rectal cancer.
We reported that the appropriate application of ULAR technique preserves anal sphincters in over 90% of patients with very low-lying rectal cancers, in which the lower margin located 3-5 cm from the anal verge, without increased morbidity or decreased oncologic results[9]. In our hospital, the sphincter preservation rate increased significantly over the 10 years, from 16.4% in Period I (January 1991 to February 1994), to 53.0% in Period II (March 1994 to March 1997), to 86.5% in Period III (April 1997 to December 2000), thanks to the introduction of ULAR with double stapling in March 1994 and ULAR with upper sphincter excision (USE) and CAA in April 1997.
On the assumption that colonic J-pouch anal anastomosis is superior to straight CAA in ULAR with USE, the procedure applied to Period III, we compare functional outcome of colonic J-pouch vs the straight CAA.
From September 1998 to January 2002 at the Seoul National University Hospital and National Cancer Center, one colorectal surgeon (J-G Park) operated on 133 rectal cancer patients in whom lower margin of the tumors were located between 3 and 5 cm from the anal verge, with all cases measured by the surgeon’s digital rectal examination. During the same period, the surgeon operated 601 patients with colon cancer and 423 patients with rectal cancer. Fifty of these one hundred and thirty-three patients were enrolled into this prospective study, for which the inclusion criteria were: (1) the presence of rectal adenocarcinoma located 3-5 cm from the anal verge, and no evidence of distant metastasis, (2) CAA after ULAR with USE performed with curative intent, and a tumor-free distal resection margin confirmed in frozen tissue sections, (3) the absence of any preoperative radiotherapy or chemotherapy, and (4) no history of hereditary colorectal cancer. After the period of this study, preoperative chemoradiotherapy was performed at the hospitals in most cases of low-lying rectal cancer.
Informed consent was obtained from all patients before surgery. We performed a standardized surgical procedure for rectal cancer in all 50 patients, which included high ligation of the inferior mesenteric artery with node dissection and total mesorectal excision. Dissection beyond the peritoneal reflection was continued to the level of the pelvic floor. After double ligation using two 7-0 silks below the tumor and/or closing with Satinsky clamp, and transanal irrigation with povidone-iodine solution, we performed ULAR with USE. USE involved excision of the upper part of the internal sphincter. In order to obtain a sufficient distal resection margin, further excision of the internal sphincter was performed below the tumor site. The resection of the mucosal layer was down to the level of the dentate line. After confirming a clear distal margin in frozen tissue sections, CAA was performed at the level of the dentate line by a transanal hand-sewing method. At the time of anastomosis, patients were also randomized using preformed random table to receive either a straight reconstruction or an anastomosis with a colonic J-pouch.
We performed a temporary diverting-loop ileostomy in all cases. The ileostomy takedown was performed after 6 mo.
All 50 patients were followed-up prospectively with a standardized questionnaire validated by the American Society of Colon and Rectal Surgeons (ASCRS)[10,11]. The Fecal Incontinence Severity Index (FISI) is based on a type×frequency matrix. The matrix includes four types of leakage commonly found in the fecal incontinent population: gas, mucus, and liquid and solid stool and five frequencies: 1-3 times per month, once per week, twice per week, once per day, and twice per day[10]. The Fecal Incontinence Quality of Life (FIQL) scale is composed of a total of 29 items; these items form four scales: lifestyle (10 items), coping/behavior (9 items), depression/self-perception (7 items), and embarrassment (3 items)[11]. Questionnaire-based interviews were performed preoperatively, and at 3, 6, 9 and 12 mo after ileostomy takedown by three surgeons.
The Mann-Whitney U-test and Fisher’s exact test were used to assess statistical significance. A linear regression model was used to determine the relationship of FISI scores with FIQL scales. Kaplan-Meier analysis with the log-rank test was used to obtain overall and disease-free survival rates. A two-sided probability level of 0.05 was accepted as significant.
Fifty patients were enrolled for this study (24 J-pouch vs 26 nonpouch). Clinicopathologic findings did not differ between patients in J-pouch and nonpouch subgroups. The median follow-up period was 43 mo.
Three complications-intestinal obstruction, urinary incontinence, defecation difficulty-occurred in 24 J-pouch cases (12.5%) and five complications-two intestinal obstructions, incisional hernia, urinary incontinence, pneumonia-occurred in 26 nonpouch cases (19.2%) (P>0.05) (Table 1).
| Nonpouch (n = 26) | J-pouch (n = 24) | |
| Sex (M:F) | 18:8 | 11:03 |
| Age (years, median) | 59 (32-76) | 57 (37-68) |
| Tumor size (cm, median) | 4.9 (2.5-7.5) | 3.2 (2.1-8.0) |
| Distance of tumor | 4.0 (3.5-4.5) | 3.9 (3.5-4.5) |
| from anal verge (cm, mean) | ||
| Distal resection | 0.7 (0.3-1.5) | 0.8 (0.3-1.4) |
| margin (cm, median)1 | ||
| Number of ileostomies (%) | 26 (100) | 24 (100) |
| Time of ileostomy | 7 (3-16) | 7 (3-18) |
| takedown (mo, median) | ||
| Differentiation | 3:20:1:2 | 5:17:2:0 |
| (WD:MD:PD:mucinous) | ||
| pT stage (T1:T2:T3) | 3:7:16 | 2:08:14 |
| pN stage (N0:N1:N2) | 14:8:4 | 10:11:3 |
| Postoperative radiotherapy (%) | 17 (65) | 12 (50) |
| Complications (%) | 5 (19.2) | 3 (12.5) |
| Recurrences | 4 (15.4) | 2 (8.3) |
| Local recurrence (2) | Local recurrence (2) | |
| Liver (1), lung (1) |
There were two cases of local recurrence in the J-pouch subgroup. One case developed recurrence at the anastomosis after 11 mo. This patient was treated by APR and is still alive after 43 mo. The other case had a recurrence at iliac lymph node after 8 mo postoperatively. This patient underwent conservative management due to general condition, and died 4 mo after the recurrence was diagnosed. In nonpouch subgroup, there were two local recurrences and two systemic recurrences. The first locally recurred case underwent APR but died 5 mo later. The other locally recurred case had a lesion at iliac lymph node 14 mo later. The two patients with lung and liver metastasis died at 17 mo and 1 mo after the diagnosis of metastasis.
We also compared the disease-free survival rate after USE with the rate after curative APR. Forty-five patients received APR by the same surgeon during the study period. This patient group had the following characteristics: median age of 59 years (range 29-79 years), 33 males, 12 females, and a Dukes’ stage distribution of 9:8:28 (A:B:C). Statistical analysis showed that the disease-free survival rates after USE and APR were not different (3-year disease-free survival rate after USE: Dukes A 90.9%, B 88.4%, C 82.6%; 3-year disease-free survival rate after APR: Dukes A 100%, B 83.3%, C 55.8%; P>0.05).
Bowel frequency The frequency of defecations was significantly lower in the J-pouch subgroup than in the nonpouch subgroup. This finding was observed for 10 mo after ileostomy takedown (Figure 1).
FISI scores and FIQL scales Statistical analysis showed that FISI scores and FIQL scales in the J-pouch subgroup were significantly better than those in the nonpouch subgroup (Table 2). A linear regression model was used to determine the correlation between FISI scores and FIQL scales. At 3 mo after ileostomy takedown, only the FIQL scales of lifestyle and embarrassment correlated with FISI scores. However, at 12 mo, all four scales highly correlated with FISI scores (P<0.05) (Table 3).
| FISI score | |||||
| Nonpouch | J-pouch | P | 1-β2 | ||
| 3 | mo | 38.9 | 31.2 | 0.017 | 0.7677 |
| 12 | mo | 27.7 | 18.6 | 0.032 | 0.7747 |
| FIQL scales | |||||
| Nonpouch | J-pouch | P | 1-β2 | ||
| 3 | mo | (n = 22) | (n = 21) | ||
| Lifestyle | 1.96 | 2.61 | 0.011 | 0.8223 | |
| Coping | 1.74 | 2.41 | 0.004 | 0.8961 | |
| Depression | 2.24 | 2.91 | 0.016 | 0.7786 | |
| Embarrassment | 2.05 | 2.73 | 0.018 | 0.7717 | |
| 12 | mo | (n = 22) | (n = 19) | ||
| Lifestyle | 2.67 | 3.37 | 0.015 | 0.8312 | |
| Coping | 2.59 | 3.18 | 0.040 | 0.7011 | |
| Depression | 2.83 | 3.64 | 0.004 | 0.9154 | |
| Embarrassment | 2.98 | 3.23 | 0.267 | 0.2663 | |
The techniques of ULAR[12] and intersphincteric resection[3,6] are now more widely applied in the treatment of low-lying rectal cancer, due to safety for a distal resection margin of 1cm[13].
The distal resection margin of present study was about 0.7-0.8 cm. In general, no less than 1-cm margin was accepted. In patients with very low-lying rectal cancer, we accepted the margin of less than 10 mm by assistance of pathologic findings. If the margin was tumor-positive on frozen section, the cases underwent APR and were excluded from the present study. Four cases with tumor-positive distal margin underwent APR. We previously reported that the appropriate application of ULAR technique preserves anal sphincters in over 90% of patients with very low-lying rectal cancers, located 3-5 cm from the anal verge, without increased morbidity or decreased oncologic results[9,14].
Despite conservation of the anus, some functional problems involving frequency, urgency and incontinence are inevitable after sphincter-preserving operations for very low-lying rectal cancers[2]. These problems gradually improves over time[15], but in about 30% of patients the problems continues beyond a year[16], and these functional problems become the main issue in postoperative quality of life. Lazorthes et al, and Parc et al, reported that the defecation frequency could be reduced by using a colonic J-pouch[7,8]. A subsequent randomized study concluded that an anastomosis using a colonic J-pouch after resection for rectal cancer could reduce the frequency of defecations and laxative use[17]. The results from the present study demonstrate that a colonic J-pouch significantly reduces the defecation frequency during 10 mo after ileostomy takedown.
The effect of the colonic J-pouch on frequency disappears after a long follow-up[18]. Our results show that the difference between the two groups was no longer apparent after 10 mo. However, because most patients undergoing such procedures have cancer and many will have a limited longevity, quality of this limited life span becomes paramount for the affected patient[19].
It has been suggested that functional improvement when using the colonic J-pouch is attributable to the capacity of the neorectum. Recently, Furst et al[20], presented the alternative possibility that bowel function is improved by reduced bowel motility. One further advantage claimed for the colonic J-pouch is that it reduces anastomotic leakage[17,18,21,22]. Proposed mechanisms for this were better blood supply to the anastomosis site[23] and reduced ‘dead space’ in the pelvic cavity due to the J-pouch[24]. In contrast to these advantages, inefficient evacuation has been a concern with the colonic J-pouch. Parc et al[8], reported that 25% of patients with colonic J-pouches needed medication for evacuation. This problem appeared to be related to the size of the pouch. Hida et al[25], appeared to have solved this problem by using a smaller, 5-6 cm pouch and this size is currently recommended in general. A randomized, isotope-based study revealed improved fluid retention in small colonic pouches[26]. The size of the pouch in the present study was 5-6 cm, and although two patients did complain of defecation difficulty (1/24 pouch group, 4.2%), their symptoms were mild and relieved by medication.
In conclusions, following ULAR with USE, the frequency of defecation was significantly lower in patients with colonic J-pouch for 10 mo after ileostomy takedown. The FISI scores and FIQL scales were significantly better in J-pouch patients than in nonpouch patients. On the basis of these findings, we recommend CAA using a colonic J-pouch in patients with rectal cancer located 3-5 cm from the anal verge undergoing ULAR with USE.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Shin HR, Jung KW, Won YJ, Park JG. 2002 annual report of the Korea Central Cancer Registry: based on registered data from 139 hospitals. Cancer Res Treat. 2004;36:103-114. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 150] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 2. | Parks AG. Transanal technique in low rectal anastomosis. Proc R Soc Med. 1972;65:975-976. [PubMed] [Cited in This Article: ] |
| 3. | Braun J, Treutner KH, Winkeltau G, Heidenreich U, Lerch MM, Schumpelick V. Results of intersphincteric resection of the rectum with direct coloanal anastomosis for rectal carcinoma. Am J Surg. 1992;163:407-412. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 80] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Rullier E, Zerbib F, Laurent C, Bonnel C, Caudry M, Saric J, Parneix M. Intersphincteric resection with excision of internal anal sphincter for conservative treatment of very low rectal cancer. Dis Colon Rectum. 1999;42:1168-1175. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 136] [Cited by in F6Publishing: 145] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 5. | Willis S, Kasperk R, Braun J, Schumpelick V. Comparison of colonic J-pouch reconstruction and straight coloanal anastomosis after intersphincteric rectal resection. Langenbecks Arch Surg. 2001;386:193-199. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 37] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Takase Y, Oya M, Komatsu J. Clinical and functional comparison between stapled colonic J-pouch low rectal anastomosis and hand-sewn colonic J-pouch anal anastomosis for very low rectal cancer. Surg Today. 2002;32:315-321. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Lazorthes F, Fages P, Chiotasso P, Lemozy J, Bloom E. Resection of the rectum with construction of a colonic reservoir and colo-anal anastomosis for carcinoma of the rectum. Br J Surg. 1986;73:136-138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 339] [Cited by in F6Publishing: 307] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 8. | Parc R, Tiret E, Frileux P, Moszkowski E, Loygue J. Resection and colo-anal anastomosis with colonic reservoir for rectal carcinoma. Br J Surg. 1986;73:139-141. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 320] [Cited by in F6Publishing: 287] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 9. | Lim SB, Heo SC, Lee MR, Kang SB, Park YJ, Park KJ, Choi HS, Jeong SY, Park JG. Changes in outcome with sphincter preserving surgery for rectal cancer in Korea, 1991-2000. Eur J Surg Oncol. 2005;31:242-249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Rockwood TH, Church JM, Fleshman JW, Kane RL, Mavrantonis C, Thorson AG, Wexner SD, Bliss D, Lowry AC. Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: the fecal incontinence severity index. Dis Colon Rectum. 1999;42:1525-1532. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 597] [Cited by in F6Publishing: 553] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 11. | Rockwood TH, Church JM, Fleshman JW, Kane RL, Mavrantonis C, Thorson AG, Wexner SD, Bliss D, Lowry AC. Fecal Incontinence Quality of Life Scale: quality of life instrument for patients with fecal incontinence. Dis Colon Rectum. 2000;43:9-16; discussion 16-17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 929] [Cited by in F6Publishing: 807] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 12. | Shirouzu K, Isomoto H, Kakegawa T. Distal spread of rectal cancer and optimal distal margin of resection for sphincter-preserving surgery. Cancer. 1995;76:388-392. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 6] [Reference Citation Analysis (0)] |
| 13. | Williams N, Seow-Choen F. Physiological and functional outcome following ultra-low anterior resection with colon pouch-anal anastomosis. Br J Surg. 1998;85:1029-1035. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 50] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Park YJ, Youk EG, Choi HS, Han SU, Park KJ, Lee KU, Choe KJ, Park JG. Experience of 1446 rectal cancer patients in Korea and analysis of prognostic factors. Int J Colorectal Dis. 1999;14:101-106. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 33] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Lazorthes F, Chiotasso P, Gamagami RA, Istvan G, Chevreau P. Late clinical outcome in a randomized prospective comparison of colonic J pouch and straight coloanal anastomosis. Br J Surg. 1997;84:1449-1451. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 135] [Cited by in F6Publishing: 134] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 16. | Williamson ME, Lewis WG, Finan PJ, Miller AS, Holdsworth PJ, Johnston D. Recovery of physiologic and clinical function after low anterior resection of the rectum for carcinoma: myth or reality? Dis Colon Rectum. 1995;38:411-418. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 127] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 17. | Hallböök O, Påhlman L, Krog M, Wexner SD, Sjödahl R. Randomized comparison of straight and colonic J pouch anastomosis after low anterior resection. Ann Surg. 1996;224:58-65. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 356] [Cited by in F6Publishing: 309] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 18. | Joo JS, Latulippe JF, Alabaz O, Weiss EG, Nogueras JJ, Wexner SD. Long-term functional evaluation of straight coloanal anastomosis and colonic J-pouch: is the functional superiority of colonic J-pouch sustained? Dis Colon Rectum. 1998;41:740-746. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 135] [Cited by in F6Publishing: 120] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 19. | Brown SR, Seow-Choen F. Preservation of rectal function after low anterior resection with formation of a neorectum. Semin Surg Oncol. 2000;19:376-385. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Fürst A, Burghofer K, Hutzel L, Jauch KW. Neorectal reservoir is not the functional principle of the colonic J-pouch: the volume of a short colonic J-pouch does not differ from a straight coloanal anastomosis. Dis Colon Rectum. 2002;45:660-667. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 76] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 21. | Nicholls RJ, Lubowski DZ, Donaldson DR. Comparison of colonic reservoir and straight colo-anal reconstruction after rectal excision. Br J Surg. 1988;75:318-320. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 156] [Cited by in F6Publishing: 142] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 22. | Ortiz H, De Miguel M, Armendáriz P, Rodriguez J, Chocarro C. Coloanal anastomosis: are functional results better with a pouch? Dis Colon Rectum. 1995;38:375-377. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 120] [Cited by in F6Publishing: 113] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 23. | Hallböök O, Johansson K, Sjödahl R. Laser Doppler blood flow measurement in rectal resection for carcinoma--comparison between the straight and colonic J pouch reconstruction. Br J Surg. 1996;83:389-392. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 108] [Cited by in F6Publishing: 100] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 24. | Dehni N, Schlegel RD, Cunningham C, Guiguet M, Tiret E, Parc R. Influence of a defunctioning stoma on leakage rates after low colorectal anastomosis and colonic J pouch-anal anastomosis. Br J Surg. 1998;85:1114-1117. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 198] [Cited by in F6Publishing: 206] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 25. | Hida J, Yasutomi M, Fujimoto K, Okuno K, Ieda S, Machidera N, Kubo R, Shindo K, Koh K. Functional outcome after low anterior resection with low anastomosis for rectal cancer using the colonic J-pouch. Prospective randomized study for determination of optimum pouch size. Dis Colon Rectum. 1996;39:986-991. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 145] [Cited by in F6Publishing: 133] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 26. | Ho YH, Yu S, Ang ES, Seow-Choen F, Sundram F. Small colonic J-pouch improves colonic retention of liquids--randomized, controlled trial with scintigraphy. Dis Colon Rectum. 2002;45:76-82. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |