Published online Feb 7, 2006. doi: 10.3748/wjg.v12.i5.760
Revised: August 9, 2005
Accepted: August 26, 2005
Published online: February 7, 2006
AIM: To objectively evaluate the effect of TJ-68 on colonic spasms during colonoscopy.
METHODS: One hundred and one patients subjected to screening colonoscopy were randomly assigned to two groups: TJ-68 in 51 subjects and saline as the control in 50. The endoscope was inserted into the sigmoid colon, then a spastic region was identified and the tip of the colonoscope was positioned at a distance of about 10 mm from the spastic region. The endoscopic view was recorded before and after direct spraying of the TJ-68 solution or warm saline. The intraluminal area of the spastic region was serially measured using a computer image analyzer and expressed as pixel counts. The area under the curve (AUC) was calculated from the pixel curve. Statistical significance was assessed by Wilcoxon’s test and Mann-Whitney U test.
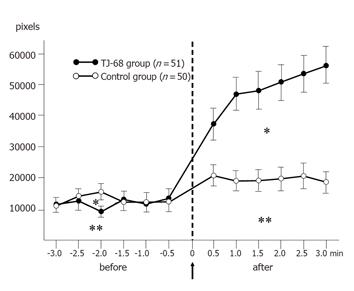
RESULTS: The mean AUC of the spastic region before and after TJ-68 spraying was 29 128 and 121 943 pixels, respectively, while with saline, it was 31 635 pixels and 48 617 pixels, respectively. Thus, the AUC significantly increased after TJ-68 spraying compared with the spraying of saline (P<0.001).
CONCLUSION: Direct spraying of TJ-68 on the colonic mucosa suppressed colonic spasm and it may be useful during colonoscopy when anticholinergic agents are contraindicated.
- Citation: Ai M, Yamaguchi T, Odaka T, Mitsuhashi K, Shishido T, Yan J, Seza A, Saisho H. Objective assessment of the antispasmodic effect of Shakuyaku-kanzo-to (TJ-68), a Chinese herbal medicine, on the colonic wall by direct spraying during colonoscopy. World J Gastroenterol 2006; 12(5): 760-764
- URL: https://www.wjgnet.com/1007-9327/full/v12/i5/760.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i5.760
In colonoscopy, it is often difficult to insert the endoscope and observation tends to be hampered because of colonic spasms. In patients with colonic spasm sometimes excess air is used to get a good view of the colonic mucosa causing discomfort and pain in the patient, and resulting in an unsuccessful colonoscopy.
Hyoscine n-butyl bromide (Hyoscine) is usually and widely used as an antispasmodic agent in colonoscopy and it is administered by intramuscular or intravenous injection. However, systemic use of Hyoscine sometimes causes many adverse reactions; namely palpitation, dry mouth, urinary retention, orthostatic hypotension, anaphylactic reactions, and temporary visual impairment. Hyoscine, in addition, often causes serious complications in patients with heart disease and it is contraindicated in such cases. For this reason, a safer means to obtain the necessary antispasmodic effect is required for colonoscopy. In this regard, peppermint oil and warm water have been investigated by directly spraying them onto the colonic wall, however, there are some limitations for their clinical use[1,2].
Shakuyaku-kanzo-to (TJ-68), a Chinese herbal medicine, is traditionally used in China and Japan, to treat patients with convulsions, spasms, a pain in the limb, etc. Recently, the analgesic and sedative effects of TJ-68 as a premedication have been reported in endoscopy[3]. Although the antispasmodic effects of TJ-68 during barium enema examination was studied, the usefulness of TJ-68 as an antispasmodic agent in colonoscopy has not been examined[4].
The aim of this study was to objectively evaluate the antispasmodic effect of TJ-68 by direct intraluminal spraying of TJ-68 solution during colonoscopy.
A total of 531 patients were registered for endoscopy between July 2002 and March 2004. Exclusion criteria were as follows: suspected intestinal bleeding, severe abdominal pain accompanied by acute colitis and inflammatory bowel disease, history of abdominal surgery, and habitual user of drugs which may affect bowel motility. Of these, 110 patients who fulfilled the eligibility criteria were allocated at random to either the TJ-68 group or the control (saline) group. Of them, 9 patients - 5 in the TJ-68 group and 4 in the control group - were excluded from this study: due to loss of sight of the endoscopic view because of influx of residual irrigation solution from the oral side. The background characteristics of all the subjects are shown in Table 1. There was no significant difference in gender, mean age, or the reason for colonoscopy between the two groups.
| TJ-68 | Control | |
| No. of cases | 51 | 50 |
| Male/female | 34/17 | 35/15 |
| Age (yr) (mean±SD) | 60.0±14.8 | 61.0±11.7 |
| Indication of colonoscopy | ||
| Polyp surveillance | 15 | 13 |
| Post EMR surveillance | 0 | 3 |
| Fecal occult blood positive | 13 | 6 |
| Abdominal pain | 3 | 6 |
| Constipation | 4 | 3 |
| Diarrhea | 2 | 5 |
| Anemia | 1 | 0 |
| Screening | 5 | 5 |
| Hematochezia | 4 | 6 |
| Bloody stool | 4 | 2 |
| Soft stool | 0 | 1 |
This study was a prospective, randomized trial performed from July 2002 to March 2004 to compare the effects of TJ-68 solution (Tsumura Co., Tokyo, Japan) with those of saline, administered by intraluminal spraying on a colonic spastic area during colonoscopy. Colonoscopy was performed by one endoscopist (MA) using a standard colonoscope (CF-Q240I; Olympus Optical Co., Ltd, Tokyo). All patients were given a routine bowel preparation including 59 g of magnesium citrate in 250 mL (Magcorol P, Horii Pharmaceutical Ind., Ltd, Osaka, Japan) on the day before the procedure and ingestion of 2 L of a balanced solution of electrolytes with 137.155 g of polyethyleneglycol (Niflec, Ajinomoto Pharma Co., Ltd, Tokyo) before the procedure. The TJ-68 solution contained; 0.5 g of TSUMURA Shakuyaku-kanzo-to Extract Granules for Ethical Use dissolved in 50 mL saline (10-2 g/mL) at 36 °C. Normal saline was also prepared at 36 °C. In our experimental observations, we found that this concentration of TJ-68 solution significantly relaxed guinea pig colonic smooth muscle (unpublished), therefore we used TJ-68 at this concentration in the present study. During the procedure, we did not use any sedative agents.
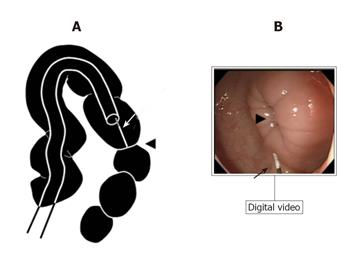
With the patient in the left decubitus position, the endoscope was advanced to about 20-25 cm from the anal canal into the sigmoid colon and then, a spastic region was identified. With the tip of the colonoscope positioned at about 10 mm from the surface of the spastic area, endoscopic views were recorded for 6 min on digital videotape before and after spraying TJ-68 solution or saline through a working channel. During the examination, no air was used. Distance between the region and the tip of the endoscope was confirmed regularly using a measured guide-wire (Figure 1).
Informed consent was obtained from all the patients and the protocol was reviewed and approved by the Institutional Review Board of our hospital.
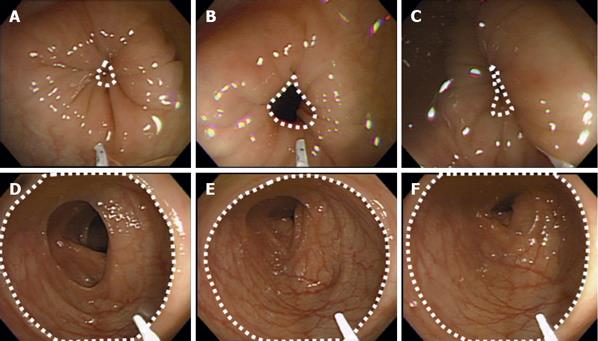
On the personal computer (VAIO PCG-GR5F, Sony), 12 spot images (3.0, 2.5, 2.0, 1.5, 1.0, and 0.5 min before and after spraying the solution) were captured every 30 s to assess luminal changes using a computer software (DVgate Still, Sony) from the recorded digital videotapes. The intraluminal spastic area was measured using a computer image analyzer (Adobe Photoshop 7.0, Adobe Systems Co., San Jose, CA, USA) and expressed as pixel counts (Figure 2). Then the mean pixel counts were used to construct a pixel curve in each group. The mean area under the curve (AUC) was calculated from the pixel curve obtained before and after spraying the TJ-68 solution or saline in each group.
Normally distributed continuous data are presented as the mean plus standard deviation and differences between the groups were evaluated by Student’s t test. Categorical data were compared with the χ2 test and Fisher’s exact test.
Wilcoxon’s test was used to compare the AUCs before and after spraying the TJ-68 solution or saline in each group. Mann-Whitney U test was used to compare the AUCs before or after spraying, A P value of <0.01 was considered statistically significant. Data were analyzed using a statistical software package (Stat Mate III, ATMS Co., Ltd, Tokyo).
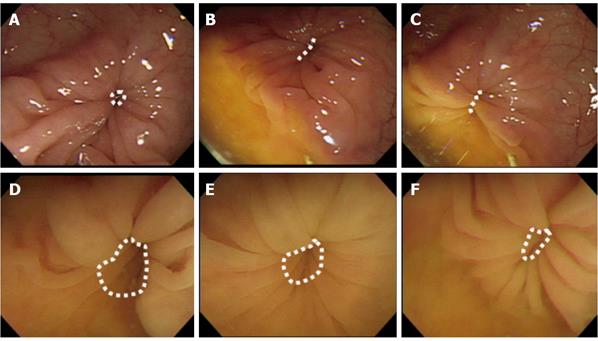
Representative endoscopic photographs of the spastic area in the sigmoid colon taken from one patient in each group before and after spraying of TJ-68 solution and normal saline are shown in Figures 3 and 4.
The mean changes of intraluminal spastic area before and after spraying of the agents are shown in Figure 5. In the TJ-68 group, the intraluminal area varied from 8 954 to 13 181 pixels at each point during 3 min before spraying, showing no difference, but after spraying, an obvious increase was observed. The intraluminal area rapidly increased 1 min after spraying and the mean area 3 min after it was 56 063 pixels. The mean AUC before and after TJ-68 spraying was 29 127 and 121 942 pixels/min, respectively, showing significant difference (P<0.001).
The mean intraluminal spastic area in the control group varied from 10 696 to 15 246 pixels at each point during 3 min before spraying, showing no difference. Spraying of saline did not significantly affect the mean intraluminal spastic area, and there was no significant increase of the mean AUC after spraying: 31 635 and 48 617 pixels/min, respectively. Thus, the AUC significantly increased after TJ-68 spraying compared with the spraying of saline (P<0.001, Table 2).
| Mean AUC (pixels×min) | ||
| Before | After | |
| TJ-68 | 29 1271 | 121 942b,d |
| Control | 31 635 | 4 86172 |
No complication was encountered in this study.
The TJ-68 solution caused the relaxation of the spastic colonic region as early as 0.5 min after spraying, and the relaxation was maintained for 3 min, or more. This phenomenon was sought to be as the local effects of the TJ-68 on the colonic wall. While in the control, the spastic area did not increase significantly after spraying of saline. Judging from the increase in the number of pixels in the control, this increase seemed to be simply attributable to a volume load. While the increase in the TJ-68 group was attributable to the active relaxing effect of TJ-68, and relaxation of the spastic area was observed within 0.5 min after spraying. We think there is a close correlation between the intraluminal movement of a spastic region and the intraluminal pressure. Actually, Asao et al. reported that the changes of the endoscopic findings by the intraluminal administration of the peppermint oil solution is correlated well with the intraluminal pressure measured by the Barostat[1]. Based on this phenomenon, we assume that TJ-68 will permeate and be absorbed through the colonic wall, and directly act on the myenteric plexus.
Since TJ-68 solution has a light brown color, blinding of the study is thought to be difficult in the strict sense. But selection of the patients or assignment of the agents to each group was performed in a strictly blind fashion. Furthermore, as relaxation of spasms was evaluated objectively, we believe that discernment of the agent after spraying had only a little influence on the outcome.
TJ-68 is an extract powder composed of Shakuyaku (Paeoniae radix) and Kanzo (Glycyrrhizae radix) combined at a ratio (g) of 1:1. TJ-68 inhibits acetylcholine-induced contraction and the contractile machinery of the smooth muscle by Kanzo and that of neurogenic contraction by Shakuyaku in guinea pig ileum[5,6]. Furthermore, the two components of TJ-68 exert synergistic effects[5].
Peppermint oil and warm water were examined in a way, analogous to our study, for their relaxing effect on the colonic wall after direct spraying[1,2]. Peppermint oil was reported to have a direct relaxing effect on the colonic smooth muscle when used in endoscopy or barium enema examination[1,7,8]. We also studied the antispasmodic effect of peppermint oil on the colonic wall using our method of evaluation and compared it to that of TJ-68. As a result, TJ-68 was found to have an antispasmodic effect similar or stronger than that of peppermint oil (data not shown). Peppermint oil is not sold via a regular medical distribution system. Furthermore, it is sometimes difficult to get and prepare the peppermint oil solution[1]. On the other hand, TJ-68 is available in any medical facility in Japan, because it is a regular medical prescription sold via a regular medical distribution system. In addition, the preparation of TJ-68 solution is easy and simple: only mixing TJ-68 with saline.
Church reported that warm water irrigation significantly reduced discomfort related to colonoscopy, but there was no difference regarding insertion time, total duration of colonoscopy, dose of midazolam administered, or frequency of severe spasm. Decrease of the patient’s discomfort was the parameter of effectiveness of warm water in their study. But their study had some limitations because they used a sedation drug (midazolam) as premedication[2]. Moreover, warm water has basically no direct antispasmodic effect on the colonic wall.
Colonic relaxation by antispasmodic drugs has been evaluated using various parameters: pain score, colonic spasm score, difficulty of the procedure scored by an endoscopist, and dose of drugs used for sedation[1,2,9-14]. However, these parameters were considered to be subjective, moreover, most studies were performed under sedation[2,9-14]. In the present study, we evaluated colonic relaxation quantitatively. In addition, we did not use any drugs to induce sedation. But the clinical relevance of TJ-68 in colonoscopy should be investigated in subsequent studies, although our preliminary study showed significant differences between the TJ-68 group and the control group in total colonoscopy time and patient’s pain score (data not shown).
Contrary to the ordinary use of antispasmodic age-nts, we sprayed TJ-68 directly on the colonic wall. Antispasmodic agents are generally administered intra-muscularly or intravenously, but systemic administration sometimes prevents the insertion of the endoscope because the muscle tone of the colon is excessively reduced[13]. Colonoscopy is difficult to carry out at the spastic region but not every spasm affects the examination. Ideally, the examiner expects to obtain effective relaxation in only some of them. In this respect, direct spraying of the antispasmodic agent TJ-68 is one of the meaningful ways of administration. But administration of this agent by spraying differed from the common oral administration. Since this was the first attempt to spray this agent directly onto the colonic wall, we had essentially no idea about the adverse effects. But the total amount of TJ-68 used in this study was no more than 2.5 g, that is to say one third of the oral dose: 7.5 g. In fact, no complication was experienced in this study.
In this study, we set the concentration of the TJ-68 solution at 10-2 mg/dL. Significant relaxation of the guinea pig distal colon was obtained with this concentration of TJ-68 in our preliminary experimental study; thus this concentration was thought to be effective enough to depress colonic spasm during colonoscopy.
In conclusion, we objectively demonstrated that intraluminal direct spraying of TJ-68 solution on the colonic mucosa could lower the colonic spasm. Additional studies are needed to determine the time required for colonoscopy or to assess patient’s compliance before TJ-68 can be definitively recommended as a useful antispasmodic agent for use in colonoscopy.
S- Editor Guo SY L- Editor Elsevier HK E- Editor Li HY
| 1. | Asao T, Mochiki E, Suzuki H, Nakamura J, Hirayama I, Morinaga N, Shoji H, Shitara Y, Kuwano H. An easy method for the intraluminal administration of peppermint oil before colonoscopy and its effectiveness in reducing colonic spasm. Gastrointest Endosc. 2001;53:172-177. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 60] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Church JM. Warm water irrigation for dealing with spasm during colonoscopy: simple, inexpensive, and effective. Gastrointest Endosc. 2002;56:672-674. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 68] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Arai M, Sato H, Shirota F. An Investigation into the Relief of the Pain Accompanying with Colonoscopy with Shakuyaku-kanzo-to. Kampo Med. 1994;44:123-128. [Cited in This Article: ] |
| 4. | Nishikawa T, Yoshimura H, Imoto I, Sakai H, Akiyama T. A clinical study of efficacy for suppression of peristaltic motion with Shakuyaku-Kanzo-to (Tsumura No.68) and peppermint oil for barium enema. Gastroenterol mass surv. 2003;41:170-176(in Japanese). [Cited in This Article: ] |
| 5. | Maeda T, Shinozuka K, Baba K, Hayashi M, Hayashi E. Effect of shakuyaku-kanzoh-toh, a prescription composed of shakuyaku (Paeoniae Radix) and kanzoh (Glycyrrhizae Radix) on guinea pig ileum. J Pharmacobiodyn. 1983;6:153-160. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 24] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Takeda S, Goto K, Ishige A, Jiann WW, Tsuen IR, Fong CC, et al. General pharmacological properties of Shakuyaku-kanzo-to. Oyo Yakuri/Pharmacometrics. 2003;64:23-31. [Cited in This Article: ] |
| 7. | Hiki N, Kurosaka H, Tatsutomi Y, Shimoyama S, Tsuji E, Kojima J, Shimizu N, Ono H, Hirooka T, Noguchi C. Peppermint oil reduces gastric spasm during upper endoscopy: a randomized, double-blind, double-dummy controlled trial. Gastrointest Endosc. 2003;57:475-482. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 8. | Asao T, Kuwano H, Ide M, Hirayama I, Nakamura JI, Fujita KI, Horiuti R. Spasmolytic effect of peppermint oil in barium during double-contrast barium enema compared with Buscopan. Clin Radiol. 2003;58:301-305. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Cutler CS, Rex DK, Hawes RH, Lehman GA. Does routine intravenous glucagon administration facilitate colonoscopy A randomized trial. Gastrointest Endosc. 1995;42:346-350. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Saunders BP, Elsby B, Boswell AM, Atkin W, Williams CB. Intravenous antispasmodic and patient-controlled analgesia are of benefit for screening flexible sigmoidoscopy. Gastrointest Endosc. 1995;42:123-127. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 31] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Saunders BP, Williams CB. Premedication with intravenous antispasmodic speeds colonoscope insertion. Gastrointest Endosc. 1996;43:209-211. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 52] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Marshall JB, Patel M, Mahajan RJ, Early DS, King PD, Banerjee B. Benefit of intravenous antispasmodic (hyoscyamine sulfate) as premedication for colonoscopy. Gastrointest Endosc. 1999;49:720-726. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Mui LM, Ng EK, Chan KC, Ng CS, Yeung AC, Chan SK, Wong SK, Chung SC. Randomized, double-blinded, placebo-controlled trial of intravenously administered hyoscine N-butyl bromide in patients undergoing colonoscopy with patient-controlled sedation. Gastrointest Endosc. 2004;59:22-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 43] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Yoong KY, Perkin D, Portal J, Strickland I, Heymann T. Intravenous hyoscine as a premedication for colonoscopy: a randomized double-blind controlled trial. Endoscopy. 2004;36:720-722. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |