Published online Mar 21, 2010. doi: 10.3748/wjg.v16.i11.1418
Revised: January 10, 2010
Accepted: January 17, 2010
Published online: March 21, 2010
Insulinomas are the most common category of pancreatic endocrine tumors, with an annual incidence of 1-4 cases per million people. Most are intrapancreatic, benign and solitary. Therefore, they have an excellent prognosis after surgical resection. However, the localization diagnosis of insulinomas still poses a challenge to surgeons and radiologists. In this case, the tumor was occult and could not be found by either abdominal enhanced spiral computed tomography (CT) or ultrasonography. Therefore, we tried a new method of CT scanning and localized the tumor.
- Citation: Bao ZK, Huang XY, Zhao JG, Zheng Q, Wang XF, Wang HC. A case of occult insulinoma localized by pancreatic dynamic enhanced spiral CT. World J Gastroenterol 2010; 16(11): 1418-1421
- URL: https://www.wjgnet.com/1007-9327/full/v16/i11/1418.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i11.1418
Insulinomas are the most common category of pancreatic endocrine tumors, with an annual incidence of 1-4 cases per million people. Most are intrapancreatic, benign and solitary. Therefore, they have an excellent prognosis after surgical resection. However, the localization diagnosis of insulinomas still poses a challenge to surgeons and radiologists. Eighty to ninety percent of insulinomas are < 2 cm in size and the lesions are distributed equally throughout the head, body and tail of the pancreas[1]. Thus, localization diagnosis before operation is important.
In the present case, the tumor was occult and could not be found by either abdominal enhanced spiral computed tomography (CT) or ultrasonography. Therefore, we tried a new method of CT scanning and localized the tumor. This paper introduces the method.
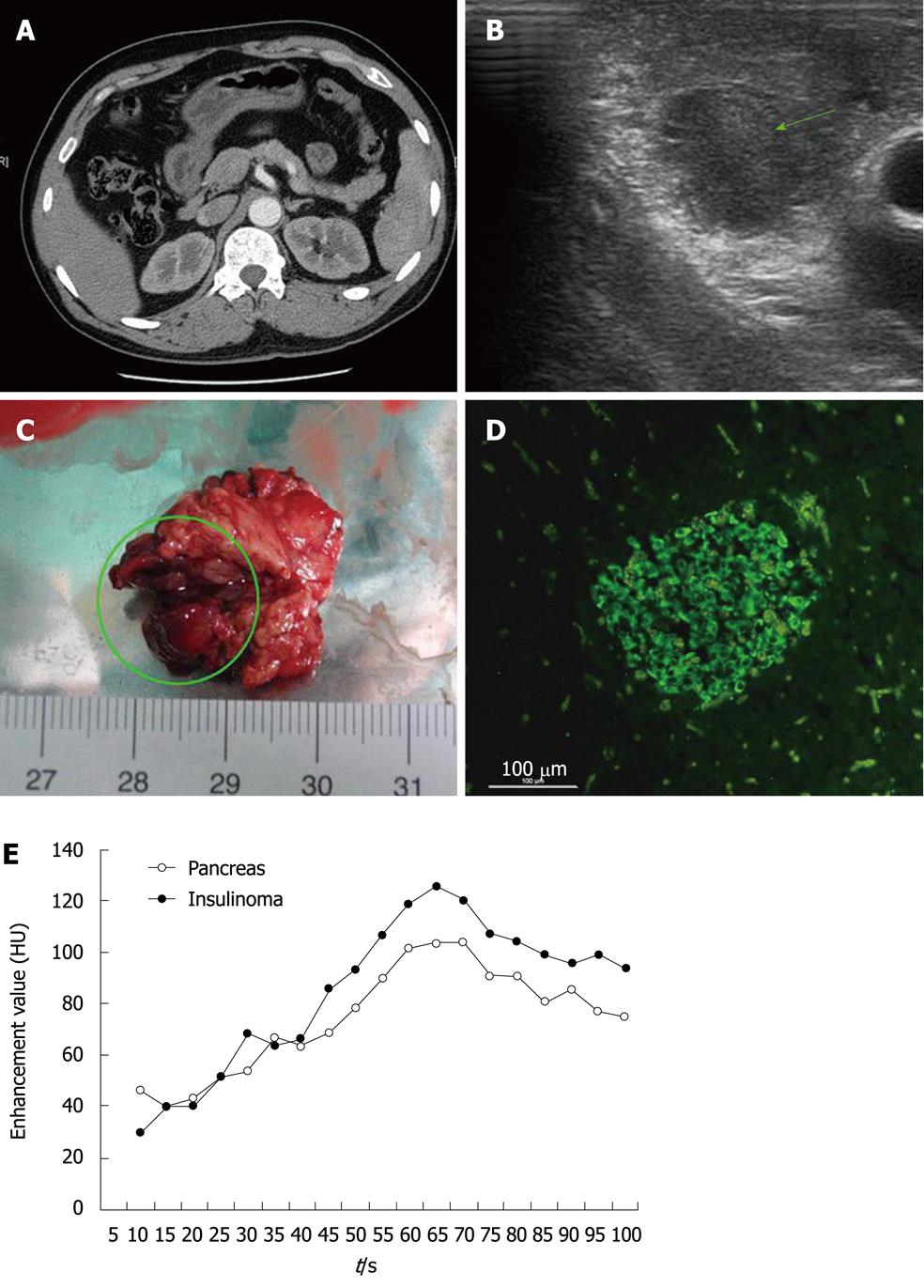
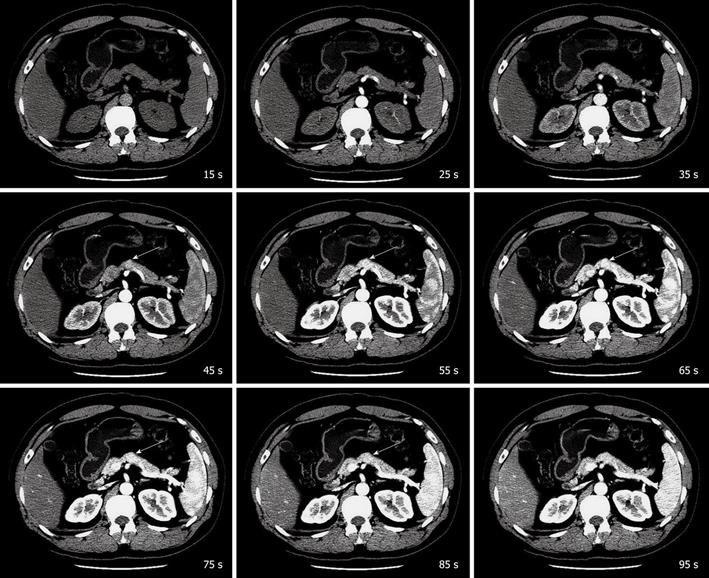
A 38-year-old man presented with a typical Whipple’s triad. He often suffered from symptoms of hypoglycemia such as hunger, sweating, palpitations, loss of consciousness and syncope. When these symptoms occurred, the blood glucose level was always below 2.48 mmol/L, and the symptoms could be relieved after being given glucose. These symptoms had lasted 14 years. During that time, he had been to many hospitals for treatment, but none of them could localize the tumor, and no one was willing to perform an exploratory operation. This time in our hospital, we tried abdominal enhanced spiral CT (Figure 1A) and ultrasonography to localize the tumor, but neither was successful. Then, the patient underwent selective arterial calcium stimulation with hepatic venous sampling. The data from the test suggested that the tumor was in the head or neck of the pancreas. Therefore, we designed a new method of CT scanning. The CT machine we used was Lightspeed VCT 64-row detector (GE Healthcare, Milwaukee, WI, USA). We chose the pancreas as the object of scanning. We use non-enhanced CT to define the range of the pancreas. After that, we started to inject contrast material (50 mL in total) by using a technology called intra-arterial infusion[2]. The injection rate was 4 mL/s. Ten seconds after the onset of injection, the dynamic enhanced CT scanning started. It was designed to scan the whole pancreas from top to bottom in 1 s. This was repeated for 90 s. The slice thickness was 5 mm. The insulinoma was finally localized in the body of the pancreas (adjoining the neck) (Figure 2). Then, with the help of intraoperative ultrasonography (Figure 1B), we performed the operation successfully. The tumor was about 1.4 cm × 1.4 cm × 1.2 cm in size (Figure 1C) and was proven to be an insulinoma by immunopathology (Figure 1D). After resection of the insulinoma, the patient was followed up for 6 mo. His blood glucose level was in the normal range, and no symptoms of hypoglycemia recurred.
Some researchers have advocated that preoperative localization diagnosis is not necessary because most insulinomas can be localized by operative exploration. Others insist that preoperative localization diagnosis is necessary and valuable for surgery[1,3]. Preoperative localization is very helpful in planning the operation: it allows the surgeon to determine whether simple tumor resection or partial pancreatectomy is likely to be required. Furthermore, it avoids prolonging the duration of surgery and potential intraoperative damage to major structures.
The advent of spiral CT has improved the detection of insulinomas compared with conventional CT. The sensitivity of CT scanning is significantly higher than it was 15 years ago[4]. A retrospective study showed that 63% of insulinomas could be detected by multiphasic spiral CT prospectively, and 83% of the lesions could be seen in retrospect[5]. However, occult insulinomas are not rare. There is still argument about which phase is more sensitive in detecting insulinoma. Some subscribe to the arterial phase, whereas others espouse that the pancreatic phase may be more useful[5]. Furthermore, different injection rates of contrast material may have great effects on enhancement of tumor and pancreas contrast. Also, the time point of the peak may be different[6,7].
Therefore, when we are confronted with an occult insulinoma, how should we localize the tumor by CT scanning? And why is abdominal dual-phase spiral CT not able to find the tumor in these patients? First of all, the interval of occult insulinoma-to-pancreas contrast is not obvious. We know that tumor delineation is based mainly on the interval of tumor-to-pancreas contrast during contrast-enhanced CT. Generally speaking, when the interval of tumor-to-pancreas contrast exceeds 30 HU, it is relatively easier to distinguish the tumor from the surrounding pancreas[6]. However, in this case, the interval of tumor-to-pancreas contrast was less than 20 HU most of the time. The largest interval was only 21.9 HU, and appeared at 65 s (Figure 1E). Secondly, as with the individual differences, the time point of the enhancement value peak of the tumor is uncertain. Thus, it is possible that abdominal dual-phase spiral CT cannot catch the time point of the peak. For these reasons, we designed the pancreatic dynamic consecutive enhanced CT scanning. It is able to display images of each time point (containing the arterial, pancreatic and portal venous phases). Also, it supplies a large number of images for radiologists to search the tumor. Therefore, when we are confronted with an occult insulinoma, pancreatic dynamic consecutive enhanced CT scanning may help us to localize the tumor.
Peer reviewer: Reiji Sugita, MD, Department of Radiology, Sendai City Medical Center, 5-22-1, Tsurugaya, Miyagino-ku, Sendai 983-0824, Japan
S- Editor Wang YR L- Editor Kerr C E- Editor Ma WH
| 1. | Abboud B, Boujaoude J. Occult sporadic insulinoma: localization and surgical strategy. World J Gastroenterol. 2008;14:657-665. [Cited in This Article: ] |
| 2. | Takeshita K, Kutomi K, Takada K, Kohtake H, Furui S. 3D pancreatic arteriography with MDCT during intraarterial infusion of contrast material in the detection and localization of insulinomas. AJR Am J Roentgenol. 2005;184:852-854. [Cited in This Article: ] |
| 3. | Ravi K, Britton BJ. Surgical approach to insulinomas: are pre-operative localisation tests necessary? Ann R Coll Surg Engl. 2007;89:212-217. [Cited in This Article: ] |
| 4. | Nikfarjam M, Warshaw AL, Axelrod L, Deshpande V, Thayer SP, Ferrone CR, Fernández-del Castillo C. Improved contemporary surgical management of insulinomas: a 25-year experience at the Massachusetts General Hospital. Ann Surg. 2008;247:165-172. [Cited in This Article: ] |
| 5. | Fidler JL, Fletcher JG, Reading CC, Andrews JC, Thompson GB, Grant CS, Service FJ. Preoperative detection of pancreatic insulinomas on multiphasic helical CT. AJR Am J Roentgenol. 2003;181:775-780. [Cited in This Article: ] |