Published online Jan 28, 2010. doi: 10.3748/wjg.v16.i4.431
Revised: October 17, 2009
Accepted: October 24, 2009
Published online: January 28, 2010
AIM: To establish the hospitalized prevalence of severe Crohn’s disease (CD) and ulcerative colitis (UC) in Wales from 1999 to 2007; and to investigate long-term mortality after hospitalization and associations with social deprivation and other socio-demographic factors.
METHODS: Record linkage of administrative inpatient and mortality data for 1467 and 1482 people hospitalised as emergencies for ≥ 3 d for CD and UC, respectively. The main outcome measures were hospitalized prevalence, mortality rates and standardized mortality ratios for up to 5 years follow-up after hospitalization.
RESULTS: Hospitalized prevalence was 50.1 per 100 000 population for CD and 50.6 for UC. The hospitalized prevalence of CD was significantly higher (P < 0.05) in females (57.4) than in males (42.2), and was highest in people aged 16-29 years, but the prevalence of UC was similar in males (51.0) and females (50.1), and increased continuously with age. The hospitalized prevalence of CD was slightly higher in the most deprived areas, but there was no association between social deprivation and hospitalized prevalence of UC. Mortality was 6.8% and 14.6% after 1 and 5 years follow-up for CD, and 9.2% and 20.8% after 1 and 5 years for UC. For both CD and UC, there was little discernible association between mortality and social deprivation, distance from hospital, urban/rural residence and geography.
CONCLUSION: CD and UC have distinct demographic profiles. The higher prevalence of hospitalized CD in more deprived areas may reflect higher prevalence and higher hospital dependency.
- Citation: Button LA, Roberts SE, Goldacre MJ, Akbari A, Rodgers SE, Williams JG. Hospitalized prevalence and 5-year mortality for IBD: Record linkage study. World J Gastroenterol 2010; 16(4): 431-438
- URL: https://www.wjgnet.com/1007-9327/full/v16/i4/431.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i4.431
Inflammatory bowel disease (IBD), comprising mainly Crohn’s disease (CD) and ulcerative colitis (UC), can be one of the most severe gastrointestinal disorders with a significant health and economic burden[1]. Presenting commonly in adolescence, IBD often results in debilitating morbidity and frequent relapses that impact heavily on educational, social, professional and family life[1-3].
CD has increased in many countries in the past few decades, with highest prevalence often reported in western regions such as Northern and Western Europe and North America[3-7]. In the United Kingdom, the incidence of UC has shown greater stability over time[6,8], while CD has continued to rise in many but not in all regions[7,9-13]. Most studies have reported that CD is more common in females than in males[8,10,11,13-16], whereas for UC, higher risks have been reported in females[3,17,18] or in males[2,19], as well as similar risks for females and males[20,21].
In the United Kingdom, the prevalence of IBD is not known accurately, although based on regional studies, it is thought to affect approximately 150 000 people[1]. Of these, the majority have active IBD, with many having severe IBD that may lead to substantial inpatient stays. Our study focused on severe IBD, which we define as an emergency admission to hospital with a length of stay of ≥ 3 d, because we wanted to study people who were acutely ill with severe IBD. Inclusion of all patients admitted to hospital, regardless of length of stay, would have covered a wide spectrum of disease severity, from elective day case investigation of IBD and admissions for elective surgery, to emergency care of patients who were severely ill with IBD.
Little is known about the prevalence of severe IBD in the United Kingdom, how it varies geographically, and its relationship with social deprivation. Mortality following hospitalization for IBD is significant[22], but few studies have been based on long-term follow-up. Additionally, little is known about the effect on mortality of social deprivation and other socio-demographic factors such as area of residence and distance from hospital. These are important aspects of the epidemiology of IBD in the United Kingdom, which are important to understand in planning service provision and treatment.
The main objective of this study was to establish the prevalence of UC and CD that was severe enough to require admission to hospital for ≥ 3 d, and to report on subsequent mortality after up to 5 years follow-up. Wales has a population of 3 million, and a mixed urban and rural geography, with areas of significant social deprivation. Further objectives were to assess geographical variation in the hospitalized prevalence and mortality for CD and UC, and to investigate associations with social deprivation and other socio-demographic characteristics, including any association between mortality and distance of patients’ residence from hospital and urban or rural residence.
For this study, we used hospital inpatient data from the Patient Episode Database for Wales (PEDW), which incorporates medical record linkage to mortality data from the National Health Service Administrative Register[23]. PEDW is a comprehensive administrative database that covers all inpatient and day-case admissions to every National Health Service (NHS) hospital in Wales, and has been used as the basis for previously published studies[24-27]. It covers 17 district general or teaching hospitals in eight NHS hospital trusts across 22 health boards, and serves the Welsh population of 3 million. We used record linkage of inpatient and mortality data because this enabled all repeat hospital admissions to be identified for the same patients, and enabled deaths following discharge from hospital to be identified, as well as in-hospital deaths.
The International Classification of Diseases, 10th Edition (ICD-10) codes used were: K50 for CDand K51 for UC. Patients with an emergency hospital admission of three or more consecutive days were classified as severe cases and included in the study. We selected only those admissions for which CD or UC was recorded as the principal diagnosis on the discharge record, and selected only the first admissions for each patient that met the study inclusion criteria during the 8-year study period from 1999 to 2007. We excluded all elective admissions, all day cases and inpatient admissions lasting < 3 d, all admissions subsequent to the first admission, and all admissions for which CD and UC were recorded on the discharge record as secondary diagnoses to other diseases such as colorectal malignancy.
Hospitalized prevalence rates for CD and UC were calculated per 100 000 resident population, using the numbers of severe hospitalized cases as the numerators and the Welsh residential population as the denominators. The direct method and the standard European population were used to standardize the prevalence rates. Mortality rates following hospital admission were calculated using the numbers of deaths (from all causes) as the numerators, and the total number of hospitalized cases, in the same time periods, as the denominators. Mortality rates were expressed as percentages and calculated at 1 and 5 years follow-up from the date of hospital admission.
To establish how mortality among the CD and UC patients compared with that in the general population, we used standardized mortality ratios (SMRs). These were calculated by applying the age- and sex-specific mortality rates in the general Welsh population to the numbers of study patients in the corresponding age- and sex-specific strata, to calculate the expected number of deaths in the study patients, and by comparing the observed deaths with the expected deaths.
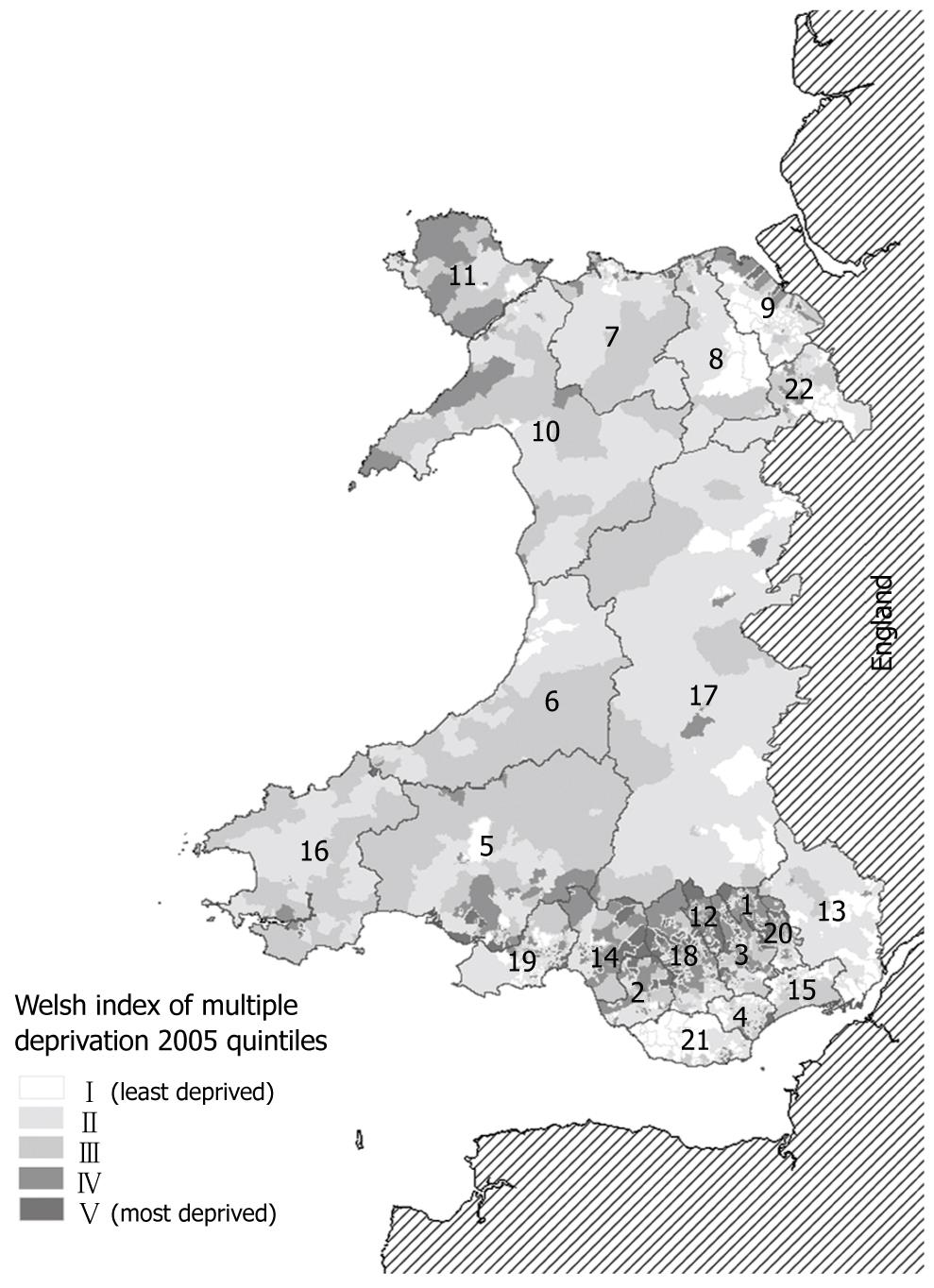
Social deprivation scores were assigned to the patients’ place of residence on each hospital record by using residential postcodes at the Lower Super Output Area (LSOA) and the Welsh Index of Multiple Deprivation (WIMD) 2005[28]. The average population size of the 1896 LSOAs in Wales in 2005 was 1560. The WIMD 2005 was based on seven domains of social deprivation: income, housing, employment, environment, health, access to services, and education. The LSOAs were ranked according to their WIMD 2005 score and grouped into quintiles, with quintile I representing the 20% of least deprived LSOAs and quintile V the 20% of most deprived LSOAs in Wales.
Urban/rural residences were measured using five categories, based on settlement sizes that ranged from < 2500 to > 100 000 people. Distances from patients’ residential LSOAs (geographical center points) to their hospital of admission were calculated using ArcGIS Geographical Information System (GIS) software and were measured in five categories that ranged from < 3 to > 20 km. Other methods used included logistic regression analysis, χ2 tests, and Pearson’s correlations.
From 1999 to 2007, there were 1467 patients hospitalized for ≥ 3 d following emergency admission for CD (mean ± SD, age: 45.8 ± 20.4 years) and 1482 for UC (mean ± SD, age: 52.0 ± 21.0 years). All the results that follow refer to these patients who meet the definition of severe IBD, although, for brevity, we omitted the repeated use of the term severe.
The overall hospitalized prevalence rate per 100 000 population was 50.1 for CD and 50.6 for UC (Table 1). Geographically, across the 22 health boards in Wales (Table 1), the prevalence of Crohn’s varied from 31.5 per 100 000 (95% CI: 22.6-42.7) to 71.3 (59.3-84.9), whereas for UC, it varied from 38.2 per 100 000 (29.6-48.5) to 89.7 (66.6-118.3).
| Health board | Map1 | No. of LSOAs | Deprivation score (mean ± SD) | CD | UC | ||||
| Cases | Prevalence (per 100 000) | 95% CI | Cases | Prevalence (per 100 000) | 95% CI | ||||
| Blaenau Gwent | 1 | 47 | 33.8 ± 12.7 | 31 | 44.7 | (30.4-63.5) | 27 | 39.0 | (25.7-56.7) |
| Bridgend | 2 | 85 | 23.2 ± 13.0 | 41 | 31.5 | (22.6-42.7) | 62 | 47.6 | (36.5-61.0) |
| Caerphilly | 3 | 110 | 27.0 ± 14.1 | 97 | 57.0 | (46.2-69.5) | 91 | 53.5 | (43.0-65.6) |
| Cardiff | 4 | 203 | 21.3 ± 18.0 | 158 | 50.9 | (43.3-59.5) | 137 | 44.1 | (37.1-52.2) |
| Carmarthenshire | 5 | 112 | 22.0 ± 10.3 | 125 | 71.3 | (59.3-84.9) | 67 | 38.2 | (29.6-48.5) |
| Ceredigion | 6 | 47 | 15.0 ± 6.2 | 35 | 46.0 | (32.0-63.9) | 30 | 39.4 | (26.6-56.2) |
| Conwy | 7 | 71 | 18.0 ± 11.0 | 64 | 57.8 | (44.5-73.8) | 84 | 75.9 | (60.6-94.0) |
| Denbighshire | 8 | 58 | 20.4 ± 15.6 | 56 | 59.0 | (44.6-76.7) | 56 | 59.0 | (44.6-76.7) |
| Flintshire | 9 | 92 | 15.0 ± 10.2 | 74 | 49.6 | (38.9-62.2) | 77 | 51.6 | (40.7-64.5) |
| Gwynedd | 10 | 75 | 17.3 ± 7.4 | 63 | 53.7 | (41.2-68.7) | 70 | 59.6 | (46.5-75.4) |
| Isle of Anglesey | 11 | 44 | 20.7 ± 8.8 | 43 | 63.0 | (45.6-84.9) | 43 | 63.0 | (45.6-84.9) |
| Merthyr Tydfil | 12 | 36 | 37.2 ± 17.0 | 26 | 46.7 | (30.5-68.4) | 50 | 89.7 | (66.6-118.3) |
| Monmouthshire | 13 | 58 | 12.2 ± 6.0 | 37 | 42.9 | (30.2-59.1) | 44 | 51.0 | (37.1-68.5) |
| Neath Port Talbot | 14 | 91 | 28.2 ± 14.4 | 76 | 56.0 | (44.1-70.0) | 53 | 39.0 | (29.2-51.0) |
| Newport | 15 | 94 | 22.0 ± 15.6 | 73 | 52.4 | (41.1-65.9) | 71 | 51.0 | (39.8-64.3) |
| Pembrokeshire | 16 | 71 | 19.4 ± 8.9 | 44 | 38.0 | (27.6-51.0) | 47 | 40.6 | (29.8-54.0) |
| Powys | 17 | 80 | 14.3 ± 6.1 | 44 | 34.2 | (24.9-46.0) | 62 | 48.2 | (37.0-61.8) |
| Rhondda Cynon Taff | 18 | 152 | 29.2 ± 15.4 | 116 | 50.0 | (41.3-60.0) | 125 | 53.9 | (44.9-64.2) |
| Swansea | 19 | 147 | 22.6 ± 17.8 | 101 | 44.9 | (36.6-54.6) | 109 | 48.5 | (39.8-58.5) |
| Torfaen | 20 | 60 | 21.3 ± 10.8 | 46 | 50.6 | (37.1-67.5) | 51 | 56.1 | (41.8-73.8) |
| Vale of Glamorgan | 21 | 78 | 15.0 ± 10.5 | 49 | 40.7 | (30.1-53.7) | 74 | 61.4 | (48.2-77.1) |
| Wrexham | 22 | 85 | 19.9 ± 13.5 | 68 | 52.5 | (40.8-66.5) | 52 | 40.2 | (30.0-52.6) |
| All Wales | 1896 | 21.7 ± 14.3 | 1467 | 50.1 | (47.5-52.7) | 1482 | 50.6 | (48.0-53.2) | |
For UC, there was a significant association between hospitalized prevalence and age (P < 0.05, Table 2). The hospitalized prevalence of UC increased with age, and was highest for males and females aged > 65 years (103 and 93.4 per 100 000, respectively). There was no significant association between the hospitalized prevalence of CD and age. The highest age-specific prevalence of CD was in the 16-29 years age group, for both males (61.4) and females (76.0). Overall, the hospitalized prevalence of CD was significantly higher (P < 0.05) in females (57.4) than in males (42.2), whereas the hospitalized prevalence of UC was very similar in females (50.1) and males (51.0, Table 2).
| CD | UC | ||||||
| Cases | Prevalence (per 100 000) | 95% CI | Cases | Prevalence (per 100 000) | 95% CI | ||
| Males | All | 601 | 42.2 | (38.9-45.8) | 726 | 51.0 | (47.4-54.9) |
| 0-15 | 25 | 8.4 | (5.5-12.5) | 20 | 6.7 | (4.1-10.4) | |
| 16-29 | 151 | 61.4 | (52.0-72.0) | 115 | 46.7 | (38.6-56.1) | |
| 30-44 | 141 | 47.6 | (40.1-56.1) | 168 | 56.7 | (48.5-66.0) | |
| 45-64 | 163 | 44.5 | (38.0-51.9) | 199 | 54.4 | (47.1-62.5) | |
| 65+ | 119 | 54.5 | (45.2-65.3) | 224 | 103 | (89.7-117) | |
| Females | All | 866 | 57.4 | (53.7-61.4) | 756 | 50.1 | (46.6-53.8) |
| 0-15 | 21 | 7.5 | (4.6-11.4) | 11 | 3.9 | (2.0-7.0) | |
| 16-29 | 185 | 76.0 | (65.5-87.8) | 114 | 46.9 | (38.6-56.3) | |
| 30-44 | 232 | 74.3 | (65.1-84.5) | 166 | 53.2 | (45.4-61.9) | |
| 45-64 | 222 | 58.9 | (51.4-67.2) | 189 | 50.1 | (43.3-57.8) | |
| 65+ | 205 | 69.4 | (60.2-79.6) | 276 | 93.4 | (82.7-105) | |
| All Wales | 1467 | 50.1 | (47.5-52.7) | 1482 | 50.6 | (48.0-53.2) | |
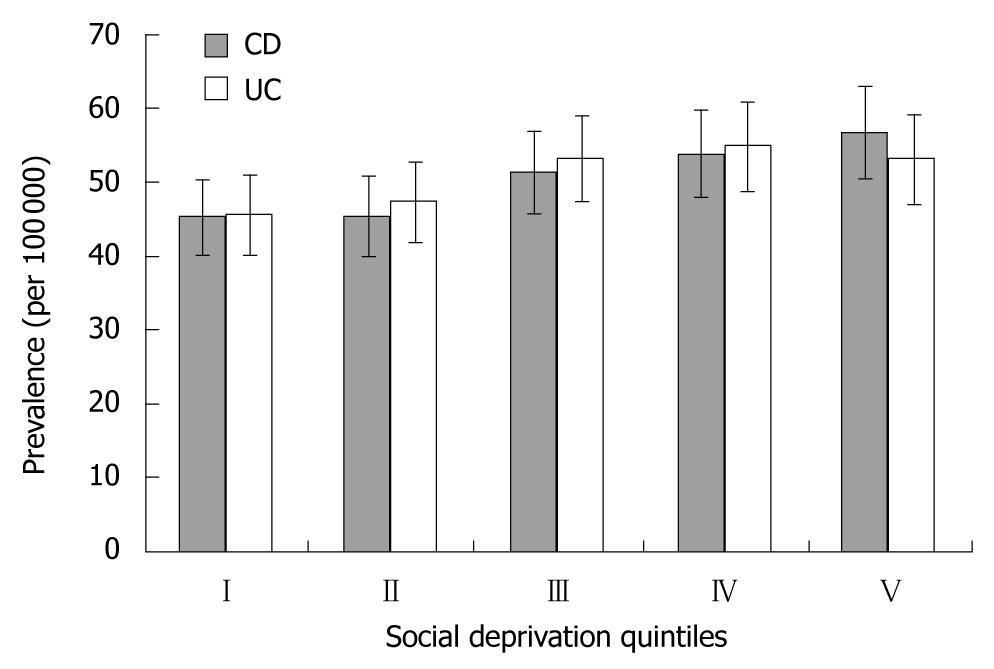
Figure 1 shows the geographical distribution of the social deprivation quintiles to the 1896 LSOAs across Wales. The hospitalized prevalence of CD was associated significantly with social deprivation at the LSOA level (Pearson’s correlation = 0.07, P = 0.004), although the association was not strong. The prevalence of CD tended to be higher in more deprived areas, although there were not quite significant differences between the most and least affluent quintiles (Figure 2). For UC, there was no significant association between prevalence and social deprivation at the LSOA level, or across any of the five social deprivation quintiles (Figure 2).
After 1 year follow-up, mortality was 6.8% for CD and 9.2% for UC (Table 3). Corresponding SMRs at 1 year were 5.1 (95% CI: 4.1-6.27; compared with mortality of 1.0 in the general population) for CD and 4.3 (95% CI: 3.6-5.1) for UC.
| CD | UC | ||||||||
| Cases | No. of deaths | Mortality rate (%) | Adjusted OR1 (95% CI) | Cases | No. of deaths | Mortality rate (%) | Adjusted OR1(95% CI) | ||
| All | 1261 | 86 | 6.8 | 1300 | 119 | 9.2 | |||
| Age groups by gender | |||||||||
| Male | All | 506 | 30 | 5.9 | 633 | 50 | 7.9 | ||
| 0-15 | 22 | 0 | 0.0 | 16 | 0 | 0.0 | |||
| 16-29 | 128 | 0 | 0.0 | 101 | 0 | 0.0 | |||
| 30-44 | 119 | 1 | 0.8 | 145 | 0 | 0.0 | |||
| 45-64 | 136 | 5 | 3.7 | 172 | 7 | 4.1 | |||
| 65+ | 99 | 24 | 24.2 | 199 | 43 | 21.6 | |||
| Female | All | 755 | 56 | 7.4 | 667 | 69 | 10.3 | ||
| 0-15 | 19 | 0 | 0.0 | 8 | 0 | 0.0 | |||
| 16-29 | 165 | 2 | 1.2 | 96 | 0 | 0.0 | |||
| 30-44 | 202 | 5 | 2.5 | 151 | 3 | 2.0 | |||
| 45-64 | 189 | 7 | 3.7 | 169 | 8 | 4.7 | |||
| 65+ | 179 | 42 | 23.5 | 243 | 58 | 23.9 | |||
| Sex | |||||||||
| Male | 504 | 30 | 6.0 | Ref. | 633 | 50 | 7.9 | Ref. | |
| Female | 754 | 56 | 7.4 | 1.05 (0.63-1.74) | 667 | 69 | 10.3 | 1.03 (0.67-1.57) | |
| Colectomy performed | |||||||||
| Yes | 193 | 9 | 4.7 | Ref. | 162 | 17 | 10.5 | Ref. | |
| No | 1068 | 77 | 7.2 | 1.59 (0.74-3.41) | 1138 | 102 | 9.0 | 0.57 (0.31-1.05) | |
| Social deprivation | |||||||||
| I (least deprived) | 229 | 16 | 7.0 | 0.99 (0.45-2.17) | 234 | 20 | 8.5 | 0.83 (0.42-1.65) | |
| II | 236 | 10 | 4.2 | 0.49 (0.21-1.18) | 245 | 21 | 8.6 | 0.89 (0.45-1.76) | |
| III | 257 | 23 | 8.9 | 1.23 (0.60-2.55) | 282 | 27 | 9.6 | 0.86 (0.46-1.61) | |
| IV | 277 | 20 | 7.2 | 0.85 (0.41-1.77) | 280 | 27 | 9.6 | 0.99 (0.52-1.86) | |
| V (most deprived) | 262 | 17 | 6.5 | Ref. | 259 | 24 | 9.3 | Ref. | |
| Urban/rural residence | |||||||||
| Under 2500 people | 256 | 17 | 6.6 | Ref. | 277 | 22 | 7.9 | Ref. | |
| 2500-9999 | 205 | 13 | 6.3 | 0.76 (0.33-1.76) | 222 | 21 | 9.5 | 1.29 (0.64-2.59) | |
| 10 000-24 999 | 278 | 26 | 9.4 | 1.48 (0.72-3.06) | 280 | 24 | 8.6 | 1.17 (0.60-2.30) | |
| 25 000-99 999 | 260 | 15 | 5.8 | 0.71 (0.32-1.60) | 274 | 28 | 10.2 | 1.48 (0.77-2.85) | |
| At least 100 000 | 262 | 15 | 5.7 | 0.67 (0.29-1.54) | 247 | 24 | 9.7 | 1.58 (0.80-3.14) | |
| Distance from hospital | |||||||||
| < 3 km | 187 | 14 | 7.5 | Ref. | 211 | 21 | 10.0 | Ref. | |
| 3-4.99 km | 145 | 6 | 4.1 | 0.55 (0.19-1.59) | 159 | 14 | 8.8 | 0.97 (0.44-2.10) | |
| 5-9.99 km | 269 | 18 | 6.7 | 1.03 (0.46-2.31) | 285 | 25 | 8.8 | 0.91 (0.47-1.76) | |
| 10-19.99 km | 318 | 22 | 6.9 | 1.14 (0.52-2.49) | 303 | 30 | 9.9 | 0.94 (0.49-1.80) | |
| ≥ 20 km | 207 | 16 | 7.7 | 1.14 (0.49-2.65) | 206 | 19 | 9.2 | 1.03 (0.50-2.13) | |
For CD and UC, mortality at 1 year increased sharply with age, and age-adjusted mortality was similar among males and females (Table 3). Very few deaths occurred among people aged < 45 years. For CD and UC, there was no significant variation in mortality according to social deprivation, urban/rural residence, distance from hospital, and whether or not an emergency colectomy was performed (Table 3). Although there was some variation in mortality across the 22 Welsh health boards, there were no significant differences between individual health boards.
Mortality at 5 years was 14.6% for CD and 20.8% for UC (Table 4). SMRs at 5 years were 2.4 (95% CI: 1.9-2.9; compared with mortality of 1.0 in the general population) for CD and 1.9 (95% CI: 1.5-2.2) for UC.
| CD | UC | ||||||||
| Cases2 | No. of deaths | Mortality rate (%) | Adjusted OR1 (95% CI) | Cases2 | No. of deaths | Mortality rate (%) | Adjusted OR1(95% CI) | ||
| All | 535 | 78 | 14.6 | 567 | 118 | 20.8 | |||
| Age groups by sex | |||||||||
| Male | All | 209 | 28 | 13.4 | 275 | 55 | 20.0 | ||
| 0-15 | 10 | 0 | 0.0 | 5 | 0 | 0.0 | |||
| 16-29 | 50 | 0 | 0.0 | 43 | 1 | 2.3 | |||
| 30-44 | 52 | 2 | 3.8 | 73 | 0 | 0.0 | |||
| 45-64 | 58 | 8 | 13.8 | 63 | 4 | 6.3 | |||
| 65+ | 39 | 18 | 46.2 | 91 | 50 | 54.9 | |||
| Female | All | 326 | 50 | 15.3 | 292 | 63 | 21.6 | ||
| 0-15 | 9 | 0 | 0.0 | 4 | 0 | 0.0 | |||
| 16-29 | 72 | 1 | 1.4 | 40 | 1 | 2.5 | |||
| 30-44 | 91 | 3 | 3.3 | 59 | 2 | 3.4 | |||
| 45-64 | 84 | 10 | 11.9 | 86 | 6 | 7.0 | |||
| 65+ | 70 | 36 | 51.4 | 103 | 54 | 52.4 | |||
| Sex | |||||||||
| Male | 209 | 28 | 13.4 | Ref. | 275 | 55 | 20.0 | Ref. | |
| Female | 326 | 50 | 15.3 | 0.96 (0.52-1.76) | 292 | 63 | 21.6 | 0.76 (0.44-1.31) | |
| Colectomy performed | |||||||||
| Yes | 89 | 10 | 11.2 | Ref. | 72 | 15 | 20.8 | Ref. | |
| No | 446 | 68 | 15.2 | 1.48 (0.63-3.52) | 495 | 103 | 20.8 | 0.59 (0.26-1.33) | |
| Social deprivation | |||||||||
| I (least deprived) | 110 | 14 | 12.7 | 0.53 (0.20-1.39) | 110 | 24 | 21.8 | 1.39 (0.61-3.19) | |
| II | 102 | 9 | 8.8 | a0.23 (0.08-0.68) | 110 | 19 | 17.3 | 0.85 (0.35-2.05) | |
| III | 112 | 16 | 14.3 | 0.56 (0.21-1.46) | 114 | 31 | 27.2 | 1.62 (0.73-3.58) | |
| IV | 106 | 21 | 19.8 | 1.09 (0.45-2.68) | 112 | 23 | 20.5 | 1.29 (0.55-3.02) | |
| V (most deprived) | 105 | 18 | 17.1 | Ref. | 121 | 21 | 17.4 | Ref. | |
| Urban/rural residence | |||||||||
| Under 2500 people | 103 | 11 | 10.7 | Ref. | 124 | 28 | 22.6 | Ref. | |
| 2500-9999 | 89 | 16 | 18.0 | 1.42 (0.49-4.12) | 105 | 22 | 21.0 | 0.64 (0.26-1.53) | |
| 10 000-24 999 | 124 | 21 | 16.9 | 1.32 (0.49-3.56) | 109 | 18 | 16.5 | 0.47 (0.19-1.17) | |
| 25 000-99 999 | 99 | 15 | 15.2 | 0.75 (0.26-2.14) | 121 | 26 | 21.5 | 0.86 (0.37-1.97) | |
| ≥ 100 000 | 120 | 15 | 12.5 | 0.89 (0.31-2.54) | 108 | 24 | 22.2 | 0.84 (0.35-1.98) | |
| Distance from hospital | |||||||||
| < 3 km | 87 | 14 | 16.1 | Ref. | 101 | 24 | 23.8 | Ref. | |
| 3-4.99 km | 73 | 9 | 12.3 | 0.52 (0.16-1.63) | 67 | 14 | 20.9 | 0.80 (0.31-2.09) | |
| 5-9.99 km | 111 | 12 | 10.8 | 0.71 (0.25-2.01) | 123 | 22 | 17.9 | 0.80 (0.35-1.85) | |
| 10-19.99 km | 135 | 17 | 12.6 | 0.81 (0.30-2.19) | 112 | 27 | 24.1 | 0.97 (0.41-2.29) | |
| ≥ 20 km | 70 | 15 | 21.4 | 1.26 (0.42-3.78) | 87 | 16 | 18.4 | 0.78 (0.31-2.00) | |
For CD and UC, mortality at 5 years was comparable among females and males, and it increased sharply among older age groups: among men aged > 65 years and women aged > 60 years, mortality was 34% for CD and 49% for UC (Table 4). There were no significant differences in mortality at 5 years according to urban/rural residence, distance travelled to hospital, or whether an emergency colectomy was performed (Table 4). For CD, mortality was significantly higher in the most deprived quintile compared with the second most affluent quintile, although there were no other significant differences in mortality according to social deprivation.
The main aims of this record linkage study were to establish the extent and prognosis of severe CD and UC in Wales, and how they are associated with social deprivation, geography and other socio-demographic aspects. It is thought that IBD affects approximately 150 000 people in the United Kingdom, with corresponding prevalence rates of 55-140 per 100 000 for CD, 160-240 per 100 000 for UC, and approximately 13 300 combined new cases diagnosed each year[1]. We found a hospitalized prevalence rate of 50.1 per 100 000 population for severe CD and 50.6 for severe UC. If these prevalence rates for Wales were applied to the whole of the United Kingdom, this would suggest a total of approximately 62 000 people hospitalized with severe IBD over the 9-year study period (30 000 for CD and 32 000 for UC).
The main strength of this study was its size, which covered almost 3000 patients who were hospitalized for IBD in a geographically defined population of nearly 3 million over a 8-year period. Further strengths are that it was based on systematic record linkage, which enabled long-term mortality follow-up of 5 years, by monitoring deaths that occurred in and following discharge from hospital. The study also used geographical measures of social deprivation to measure social inequality comprehensively on a national scale, as well as other novel prognostic/demographic risk factors, such as distance from home to hospital and urban or rural residences.
We defined severe IBD as emergency hospitalization for IBD, as the principal reason for admission, which lasted ≥ 3 d. This was to distinguish severe illness from relatively minor illness and from day-case investigations. We accept that the definition may also have included some patients who were admitted with long stays for other serious illnesses, for example, myocardial infarction or pneumonia, who also had IBD. However, we sought to minimize this by restricting case selection to people in whom IBD itself was coded as the principal reason for admission.
The main limitation of record linkage studies such as this is the lack of detailed information about the history, severity and management of the illness. It was not possible to ascertain the extent of disease from endoscopic evidence or detailed pathology information from our data sources. Our hospitalized prevalence rates referred specifically to CD and UC patients with an inpatient stay of ≥ 3 d following emergency admission. Although length of stay is often affected by factors such as age, comorbidity, and effectiveness of self care and social support, we believe that a length of stay of ≥ 3 d after emergency admission usually indicates severe disease that requires intensive medical or surgical treatment rather than admission for diagnosis or assessment.
For both males and females, we found a continuous rise in the hospitalized prevalence of UC as age increased. For CD, we found highest prevalence among patients aged 16-29 years, with a second peak in prevalence in males aged > 65 years and females aged ≥ 60 years. We also found a higher prevalence of CD in females than in males, but a similar prevalence of UC among males and females, which is consistent with other studies[8,10,11,13,14,16,19,29].
IBD has been linked with higher socioeconomic groups in some studies, particularly for CD[30,31], but also for UC[31], although other studies have reported no association[32-34]. Instead, we found slightly higher hospitalized prevalence of CD in more socially deprived locations, although there were not quite significant differences across the social deprivation quintiles. As our study focused on more severe cases, possible reasons for this include higher levels of health-care dependency as well as higher levels of smoking and more comorbidity among patients from more deprived social backgrounds. For UC, we found no significant association between hospitalized prevalence and social deprivation. The differing demographic profiles between CD and UC, and the stronger evidence of an association between CD and social deprivation suggests that environmental factors play a stronger part in the etiology of CD, but attempts to establish environmental factors have proved inconclusive and sometimes controversial in the past[31,33-37].
Overall mortality was 6.8% at 1 year and 14.6% at 5 years for CD, compared with 9.2% at 1 year and 20.8% at 5 years for UC. At 5 years, mortality was high among older patients (49% and 54% for CD and UC, respectively, among patients aged ≥ 65 years). The higher mortality for UC is consistent with other studies[16,22,38], although there is a lack of large studies with long-term follow-up for people hospitalized with IBD. Mortality at 1 year follow-up was five times higher than in the general population for CD and four times higher for UC. At 5 years, mortality was increased two fold for CD and UC. An earlier study has reported SMRs of 3.2 and 2.4 after 3 years follow-up for people hospitalized with severe CD and UC, respectively, in England[22], and further demonstrates that people hospitalized with severe IBD are often at increased risk of mortality, which continues in the long term. Elective colectomy may well be the most effective means of reducing these excess risks of mortality[22].
Although there was some variation in prognosis geographically across health boards, it was not significant for either CD or UC. We also found little discernible association between social deprivation quintiles, distance travelled to hospital and rural versus urban residence, and subsequent mortality at either 1 or 5 years. As IBD often relapses and requires regular monitoring and surveillance, it is possible that patients who live remotely from outpatient clinics and hospital care may have poorer outcomes. Our findings for mortality outcomes do not support such concerns, although recent health service developments in the United Kingdom that encourage greater management and treatment of IBD in primary care may partially offset the distances travelled by patients.
We found that severe CD and UC had quite distinct demographic profiles in Wales. CD and UC also showed slightly differing patterns of association with social deprivation. The higher prevalence of hospitalized CD in more deprived areas may reflect higher smoking rates, more comorbidity and higher levels of hospital dependency, as well as higher prevalence.
The prevalence of Crohn’s disease (CD) has increased in many countries in recent decades. Although inflammatory bowel disease (IBD) is thought to affect about 150 000 people in the United Kingdom, the prevalence of severe IBD is not known. Mortality following hospitalization for IBD is significant but little has been reported on long-term follow-up.
This study determined the hospitalized prevalence of severe IBD and subsequent 5-year mortality in Wales, and investigates associations between severe IBD and social deprivation, distance travelled to hospital, and other socio-demographic characteristics.
This study showed that the hospitalized prevalence of severe CD was slightly higher among the most deprived groups but there was no association between social deprivation and severe ulcerative colitis (UC). Five-year mortality was high for severe CD (14.6%) and UC (20.8%), but there was little association between mortality and social deprivation, distance from hospital, urban/rural residences or geography.
The higher hospitalized prevalence of severe CD among the most deprived groups, and differing demographic profiles between CD and UC, suggest that environmental factors play a more significant role in the etiology of CD. The findings of this large population-based study on the prevalence and mortality of IBD are also important for service planning and provision.
Hospitalized prevalence of severe IBD in this study referred to the number of people (per 100 000 population) who were hospitalized as an emergency for ≥ 3 d for IBD, as the principal reason for admission, on at least one occasion during the 8-year study period. One and five-year mortality referred to the percentage of these people who died during the subsequent one and five-year follow-up period.
This was a well-conducted, large epidemiological study that provided interesting and novel findings. For example, the findings that distance travelled by patients to hospital did not affect long-term mortality for CD or UC has not been reported previously.
Peer reviewer: Tauseef Ali, Assistant Professor, Department of Gastroenterology, University of Oklahoma, WP 1360 Digestive Disease, 920 SL Young Blvd, Oklahoma City, OK 73104, United States
S- Editor Tian L L- Editor Kerr C E- Editor Ma WH
| 1. | Williams JG, Roberts SE, Ali MF, Cheung WY, Cohen DR, Demery G, Edwards A, Greer M, Hellier MD, Hutchings HA. Gastroenterology services in the UK. The burden of disease, and the organisation and delivery of services for gastrointestinal and liver disorders: a review of the evidence. Gut. 2007;56 Suppl 1:1-113. [Cited in This Article: ] |
| 2. | Karlinger K, Györke T, Makö E, Mester A, Tarján Z. The epidemiology and the pathogenesis of inflammatory bowel disease. Eur J Radiol. 2000;35:154-167. [Cited in This Article: ] |
| 3. | de Dombal FT. Ulcerative colitis. Epidemiology and aetiology, course and prognosis. Br Med J. 1971;1:649-650. [Cited in This Article: ] |
| 4. | Baumgart DC, Carding SR. Inflammatory bowel disease: cause and immunobiology. Lancet. 2007;369:1627-1640. [Cited in This Article: ] |
| 5. | Danese S, Sans M, Fiocchi C. Inflammatory bowel disease: the role of environmental factors. Autoimmun Rev. 2004;3:394-400. [Cited in This Article: ] |
| 6. | Srivastava ED, Mayberry JF, Morris TJ, Smith PM, Williams GT, Roberts GM, Newcombe RG, Rhodes J. Incidence of ulcerative colitis in Cardiff over 20 years: 1968-87. Gut. 1992;33:256-258. [Cited in This Article: ] |
| 7. | Lee FI, Costello FT. Crohn’s disease in Blackpool--incidence and prevalence 1968-80. Gut. 1985;26:274-278. [Cited in This Article: ] |
| 8. | Primatesta P, Goldacre MJ. Crohn’s disease and ulcerative colitis in England and the Oxford record linkage study area: a profile of hospitalized morbidity. Int J Epidemiol. 1995;24:922-928. [Cited in This Article: ] |
| 9. | Mayberry J, Rhodes J, Hughes LE. Incidence of Crohn’s disease in Cardiff between 1934-1977. Gut. 1979;20:602-608. [Cited in This Article: ] |
| 10. | Humphreys WG, Brown JS, Parks TG. Crohn’s disease in Northern Ireland--a retrospective study of 440 cases. Ulster Med J. 1990;59:30-35. [Cited in This Article: ] |
| 11. | Kyle J. Crohn’s disease in the northeastern and northern Isles of Scotland: an epidemiological review. Gastroenterology. 1992;103:392-399. [Cited in This Article: ] |
| 12. | Fellows IW, Freeman JG, Holmes GK. Crohn’s disease in the city of Derby, 1951-85. Gut. 1990;31:1262-1265. [Cited in This Article: ] |
| 13. | Gunesh S, Thomas GA, Williams GT, Roberts A, Hawthorne AB. The incidence of Crohn’s disease in Cardiff over the last 75 years: an update for 1996-2005. Aliment Pharmacol Ther. 2008;27:211-219. [Cited in This Article: ] |
| 14. | Brown JS, Humphreys WG, Parks TG. Changing pattern of Crohn’s disease in Northern Ireland. Br Med J (Clin Res Ed). 1988;296:1444-1445. [Cited in This Article: ] |
| 15. | Smith IS, Young S, Gillespie G, O’Connor J, Bell JR. Epidemiological aspects of Crohn’s disease in Clydesdale 1961-1970. Gut. 1975;16:62-67. [Cited in This Article: ] |
| 16. | Sonnenberg A. Mortality from Crohn’s disease and ulcerative colitis in England-Wales and the U.S. from 1950 to 1983. Dis Colon Rectum. 1986;29:624-629. [Cited in This Article: ] |
| 17. | Evans JG, Acheson ED. An epidemiological study of ulcerative colitis and regional enteritis in the Oxford area. Gut. 1965;6:311-324. [Cited in This Article: ] |
| 18. | Edwards FC, Truelove SC. The course and prognosis of ulcerative colitis. Gut. 1963;4:299-315. [Cited in This Article: ] |
| 19. | Montgomery SM, Morris DL, Thompson NP, Subhani J, Pounder RE, Wakefield AJ. Prevalence of inflammatory bowel disease in British 26 year olds: national longitudinal birth cohort. BMJ. 1998;316:1058-1059. [Cited in This Article: ] |
| 20. | Ehlin AG, Montgomery SM, Ekbom A, Pounder RE, Wakefield AJ. Prevalence of gastrointestinal diseases in two British national birth cohorts. Gut. 2003;52:1117-1121. [Cited in This Article: ] |
| 21. | Jess T, Riis L, Vind I, Winther KV, Borg S, Binder V, Langholz E, Thomsen OØ, Munkholm P. Changes in clinical characteristics, course, and prognosis of inflammatory bowel disease during the last 5 decades: a population-based study from Copenhagen, Denmark. Inflamm Bowel Dis. 2007;13:481-489. [Cited in This Article: ] |
| 22. | Roberts SE, Williams JG, Yeates D, Goldacre MJ. Mortality in patients with and without colectomy admitted to hospital for ulcerative colitis and Crohn’s disease: record linkage studies. BMJ. 2007;335:1033. [Cited in This Article: ] |
| 23. | Welsh Assembly Government. NHS Administrative Register. Cardiff: Welsh Assembly Government 2006; . [Cited in This Article: ] |
| 24. | Lyons RA, Jones SJ, Deacon T, Heaven M. Socioeconomic variation in injury in children and older people: a population based study. Inj Prev. 2003;9:33-37. [Cited in This Article: ] |
| 25. | Brophy S, John G, Evans E, Lyons RA. Methodological issues in the identification of hip fractures using routine hospital data: a database study. Osteoporos Int. 2006;17:405-409. [Cited in This Article: ] |
| 26. | Polinder S, Meerding WJ, Lyons RA, Haagsma JA, Toet H, Petridou ET, Mulder S, van Beeck EF. International variation in clinical injury incidence: exploring the performance of indicators based on health care, anatomical and outcome criteria. Accid Anal Prev. 2008;40:182-191. [Cited in This Article: ] |
| 27. | Lyons RA, Ward H, Brunt H, Macey S, Thoreau R, Bodger OG, Woodford M. Using multiple datasets to understand trends in serious road traffic casualties. Accid Anal Prev. 2008;40:1406-1410. [Cited in This Article: ] |
| 28. | Lyons RA; WAG. Welsh Index of Multiple Deprivation 2005. Cardiff: Welsh Assembly Government (WAG) 2005; . [Cited in This Article: ] |
| 29. | Armitage E, Drummond H, Ghosh S, Ferguson A. Incidence of juvenile-onset Crohn’s disease in Scotland. Lancet. 1999;353:1496-1497. [Cited in This Article: ] |
| 30. | Blanchard JF, Bernstein CN, Wajda A, Rawsthorne P. Small-area variations and sociodemographic correlates for the incidence of Crohn‘s disease and ulcerative colitis. Am J Epidemiol. 2001;154:328-335. [Cited in This Article: ] |
| 31. | Green C, Elliott L, Beaudoin C, Bernstein CN. A population-based ecologic study of inflammatory bowel disease: searching for etiologic clues. Am J Epidemiol. 2006;164:615-623; discussion 624-628. [Cited in This Article: ] |
| 32. | Logan RF, Kay CR. Oral contraception, smoking and inflammatory bowel disease--findings in the Royal College of General Practitioners Oral Contraception Study. Int J Epidemiol. 1989;18:105-107. [Cited in This Article: ] |
| 33. | Duggan AE, Usmani I, Neal KR, Logan RF. Appendicectomy, childhood hygiene, Helicobacter pylori status, and risk of inflammatory bowel disease: a case control study. Gut. 1998;43:494-498. [Cited in This Article: ] |
| 34. | Gent AE, Hellier MD, Grace RH, Swarbrick ET, Coggon D. Inflammatory bowel disease and domestic hygiene in infancy. Lancet. 1994;343:766-767. [Cited in This Article: ] |
| 35. | el-Omar E, Penman I, Cruikshank G, Dover S, Banerjee S, Williams C, McColl KE. Low prevalence of Helicobacter pylori in inflammatory bowel disease: association with sulphasalazine. Gut. 1994;35:1385-1388. [Cited in This Article: ] |
| 36. | Pearce CB, Duncan HD, Timmis L, Green JR. Assessment of the prevalence of infection with Helicobacter pylori in patients with inflammatory bowel disease. Eur J Gastroenterol Hepatol. 2000;12:439-443. [Cited in This Article: ] |
| 37. | Korzenik JR. Is Crohn’s disease due to defective immunity? Gut. 2007;56:2-5. [Cited in This Article: ] |
| 38. | Delcò F, Sonnenberg A. Commonalities in the time trends of Crohn’s disease and ulcerative colitis. Am J Gastroenterol. 1999;94:2171-2176. [Cited in This Article: ] |