Published online Jan 28, 2010. doi: 10.3748/wjg.v16.i4.462
Revised: October 7, 2009
Accepted: October 15, 2009
Published online: January 28, 2010
AIM: To compare defecographic abnormalities in symptomatic men and women and to analyze differences between men and age- and symptom-matched women.
METHODS: Sixty-six men (mean age: 55.4 years, range: 20-81 years) who complained of constipation and/or fecal incontinence and/or pelvic pain underwent defecography after intake of a barium meal. Radiographs were analyzed for the diagnosis of rectocele, enterocele, intussusception and perineal descent. They were compared with age- and symptom-matched women (n = 198) who underwent defecography during the same period.
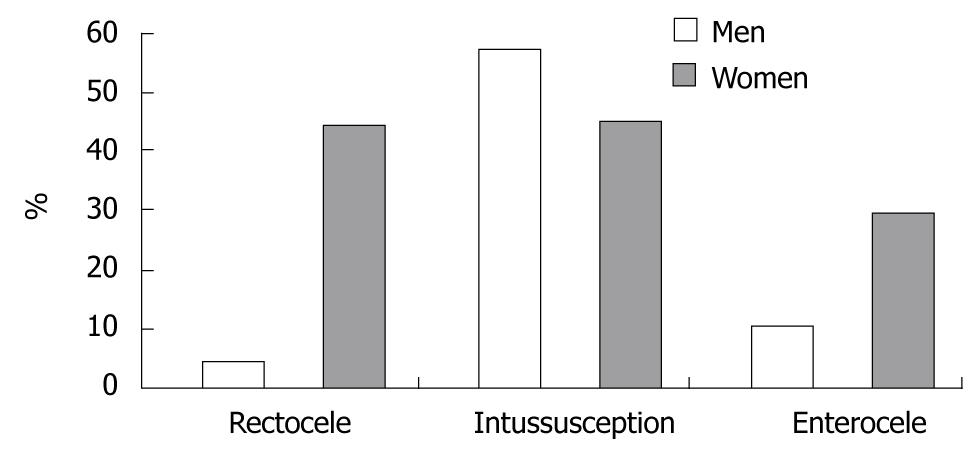
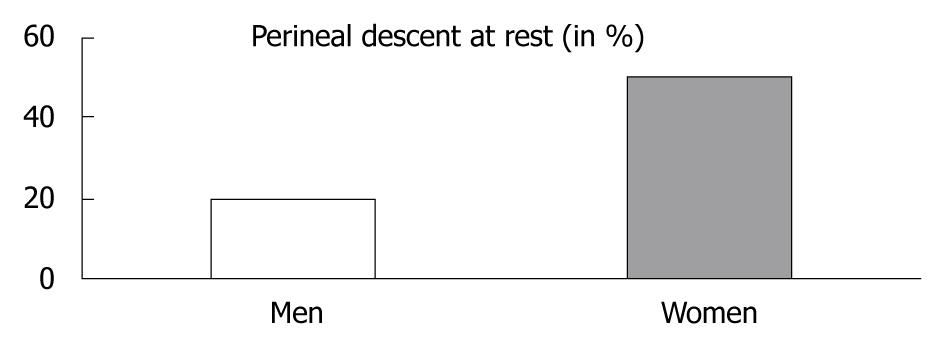
RESULTS: Normal defecography was observed in 22.7% of men vs 5.5% of women (P < 0.001). Defecography in men compared with women showed 4.5% vs 44.4% (P < 0.001) rectocele, and 10.6% vs 29.8% (P < 0.001) enterocele, respectively. No difference was observed for the diagnosis of intussusception (57.6% vs 44.9%). Perineal descent at rest was more frequent in women (P < 0.005).
CONCLUSION: For the same complaint, diagnosis of defecographic abnormalities was different in men than in women: rectocele, enterocele and perineal descent at rest were observed less frequently in men than in women.
- Citation: Savoye-Collet C, Savoye G, Koning E, Leroi AM, Dacher JN. Gender influence on defecographic abnormalities in patients with posterior pelvic floor disorders. World J Gastroenterol 2010; 16(4): 462-466
- URL: https://www.wjgnet.com/1007-9327/full/v16/i4/462.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i4.462
Constipation, fecal incontinence and pelvic pain require meticulous evaluation because therapy can be effective and help patients to lead a fuller life. Radiographic dynamic rectal examination (defecography) is a valuable method to assess evacuation disorders[1-5]. This method provides precise information on anorectal and pelvic floor functions[6-8]. It can be used to evaluate efficiently defecation disorders after clinical examination for the exploration of constipation, pelvic pain and anal incontinence[9-13].
Posterior pelvic floor disorders are common and well known in women, and some are related to obstetrical consequences. Little is known about gender influence in symptomatic patients investigated by defecography[14,15]. Men can also complain of constipation, fecal incontinence and pelvic pain, and these symptoms need the same careful evaluation because they may need specific therapy[16].
The purpose of our study was to compare prevalence of defecographic abnormalities in men and age- and symptom-matched women.
Over a 6-year period, 66 symptomatic aged 20-81 years (mean ± SD: 55.4 ± 14.9 years) addressed for defecography were evaluated consecutively in our institution. All patients were referred by a gastroenterologist or a digestive tract surgeon for the exploration of constipation, pelvic pain or fecal incontinence. Constipation was defined as less than two bowel movements per week. Fecal incontinence was defined by an uncontrolled loss of liquid or solid stools that corresponded to grade C and D of Park’s classification[17].
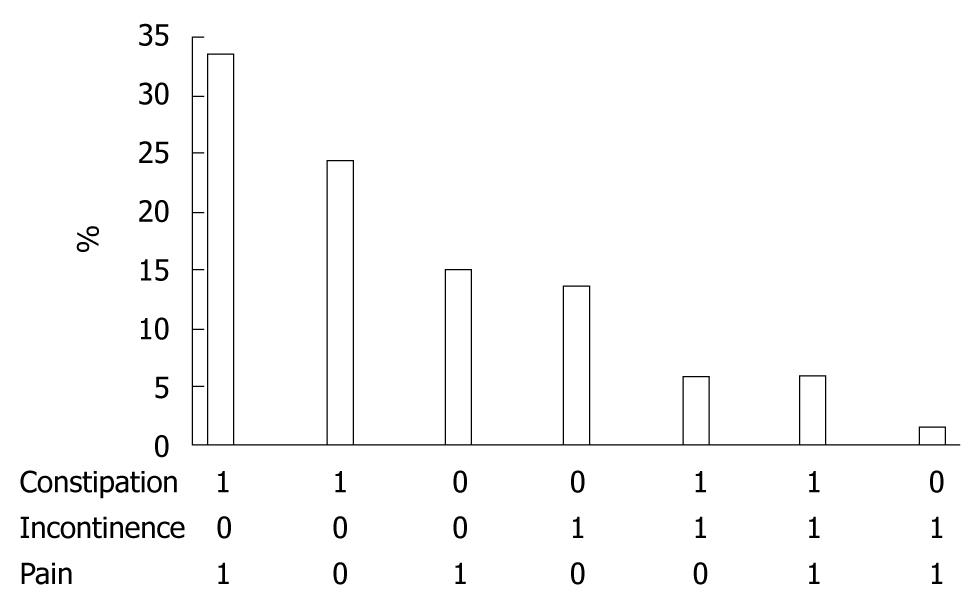
To compare defecographic abnormalities in men with women, a case-matched series was isolated from a prospective database of women (n = 700) investigated by defecography in the same period with the same techniques. Three women for one man were isolated. A series of 198 age- and symptom-matched women was studied. A value of 0 (absence) or 1 (presence) was attributed to each of the three types of symptoms (constipation, anal incontinence or pelvic pain) for all the patients in the database. Several age groups (5-years periods) were isolated for both genders. In these groups of similar age, three women with the same combination of symptoms were associated with one man. The choice of the symptom-matched women was done blindly of the results of the defecography from a global database that contained all the symptomatic patients who underwent defecography during this period in our unit. For example, for a 63-year-old man with constipation and pelvic plain (values = 1/0/1), three women (aged 60-65 years) with the same combination (1/0/1) were isolated. The women were aged 20-81 years (mean: 55.1 ± 14 years).
We applied a standardized protocol to perform and evaluate all defecography examinations. All patients received a barium meal 1.5 h before the examination to opacify the pelvic small bowel for the detection of enterocele. A lateral X-ray was first performed for bone and pelvic loop visualization. In women, a thick barium paste was injected into the vagina, to mark out the posterior vaginal wall. Then, 150 mL of thickened and viscous high-density barium contrast medium was injected in the rectum with the patient in the left lateral position.
Films were taken in a standing lateral position during the following maneuvers: at rest, at voluntary and maximal contraction of the sphincter and pelvic floor (“squeeze”), and at straining without defecation (“strain”). The pubococcygeal line was defined and the distance between this line and the anorectal junction was determined for the three positions. Finally, patients sat on an upright commode attached to the footboard of the fluoroscopy table (a modified toilet), and one frame per second films were taken during expulsion and after completion of defecation at maximum straining.
Precise explanations of the entire procedure were given by the radiologist prior to defecography. In young women, defecography was always performed during the first part of the cycle. Image analysis was done by one of the senior radiologists involved in this study (CSC or EK).
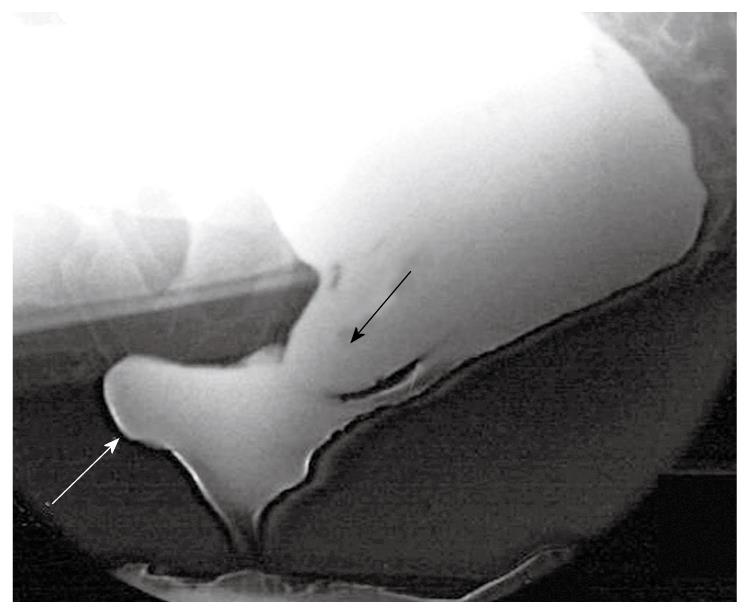
Pathological patterns were defined as follows. Pelvic floor descent was assessed from standing lateral views during maneuvers. For the diagnosis of perineal descent at rest, the distance in millimeters between the anorectal junction and the pubococcygeal line was noted. Perineal descent at rest was defined as a distance of > 30 mm. For perineal descent at straining, the difference in millimeters between the anorectal junction position at straining and at rest was noted. Perineal decent at straining was defined as a difference of > 20 mm between the two positions. The number of male and female patients with perineal descent at rest was compared. Anterior rectocele was defined as > 30 mm outpouching of the anterior rectal wall. This outpouching should persist on incomplete evacuation. Intussusception was defined as an invagination of the rectal wall, either intrarectal, intra-anal, or an external prolapse of the whole circumference. Enterocele was defined as herniation of the small bowel between the vaginal posterior wall and the anterior rectal wall.
χ2 tests were used for the comparison of rectocele, enterocele, perineal descent and intussusception. P < 0.05 was regarded as significant.
Constipation, fecal incontinence and pelvic pain were present in 69%, 27% and 56% of our male patients, respectively. These symptoms could be isolated (53%) or associated (Figure 1). The more frequent association was constipation and pelvic pain (33%).
Defecography could be satisfactorily performed in all patients and all examinations could be analyzed fully with the above-described criteria. In men, 22.7% of the defecography procedures were normal versus 5.5% in women (P < 0.001).
Defecography in men showed intussusception in 38 patients (57.6%), enterocele in seven (10.6%), and rectocele in three (4.5%). Defecography in women showed intussusception in 89 patients (44.9%), enterocele in 59 (29.8%), and rectocele in 88 (44.4%). There was a significantly higher proportion of rectocele and enterocele in matched women (Figures 2 and 3). There was no statistically significant difference for the diagnosis of intussusception.
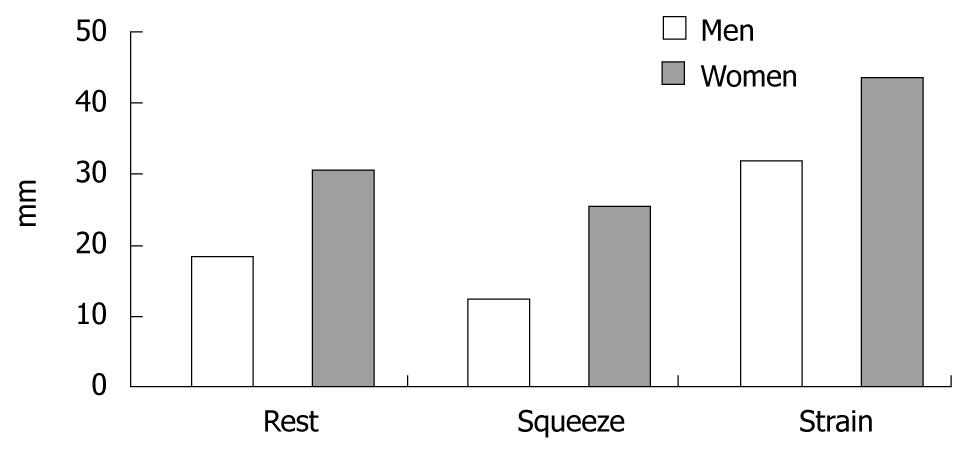
Distance between the pubococcygeal line and the anorectal junction at the three positions (rest, squeeze and strain) was significantly different between men and women, with a lower position of the perineum in women regardless of position (P < 0.001) (Figure 4). There was a greater incidence of perineal descent at rest in women compared with men (P < 0.005) (Figure 5). There was no difference between men and women for the diagnosis of perineal descent at straining.
Defecography is used commonly in women, but only a few procedures are carried out in men. In our department, men represented < 10% of all defecography procedures. To the best of our knowledge, no specific study of defecography has been carried out to explore the gender difference in the diagnosis of defecographic abnormalities. The pairing of our case-matched study was done for age and symptoms, with one man for three matched women, as is usual in this type of study. It allowed us to establish any sex difference in the prevalence of defecographic abnormalities.
Intussusception is very common in both sexes (approximately half of patients undergoing defecography)[7,8]. We did not observe any sex difference in prevalence. Enterocele and rectocele were more common in matched women. This could be explained by obstetrical anteriority (vaginal delivery or hysterectomy). The consequences of obstetric damage on the perineum are well known[18,19]. Enterocele is also more frequent after hysterectomy[20]. Rectocele is diagnosed 10 times more frequently in women, and appears to be characteristic of the female population. Rectocele has been reported previously as being uncommon in men[15]. Chen et al[15] have reported a prevalence higher than ours (17% vs 4.4%), and a frequent association between rectocele and prostatectomy (40%). We did not assess the history of all patients, but this difference could be explained by the higher mean age of the patients in the study of Chen et al[15] (72.4 years) than in our study (55.4 years), because prostatectomy is more likely in older patients.
The distance between the pubococcygeal line and the anorectal junction, which determines the position of the perineum, was greater in women for the three positions (rest, squeeze and strain). As a consequence, there was a gender difference for the diagnosis of perineal descent at rest. There was no such difference for perineal descent at straining. This raises the question that the normal level of the perineum could be different in both sexes. However, our study concerned only symptomatic patients and this needs to be investigated in control subjects. No sex-related definition of pelvic floor disorders was established, therefore, our diagnostic criteria were those commonly used, which means those used in women. However, new criteria for the diagnosis of perineal descent at rest in men could probably be defined. The same question can also be raised in elderly patients, for whom diagnostic criteria could also be adapted[21].
Determination of the clinical value of defecographic abnormalities is also difficult and remains a subject of debate[22-26]. Defecographic abnormalities have been shown not to be symptom-related[12]. This study confirmed this finding, because there were gender differences among symptom-matched patients. Interpretation should be cautious because radiographic changes can be demonstrated in healthy subjects of various ages[27,28]. Interobserver agreement is good for rectocele and enterocele[29] but appears insufficient for perineal descent[25]. Different methods for measuring parameters, especially perineal descent, have been described, with controversy as to which is the most accurate, and with little agreement[26,30,31]. New examinations are also possible, such as magnetic resonance defecography, to assess pelvic floor disorders[32,33].
In conclusion, defecography is a potential adjunct to clinical evaluation of men with constipation, fecal incontinence or pelvic pain. With symptoms equal, some defecographic abnormalities are sex-related: rectocele, enterocele and perineal descent at rest were observed less frequently in men.
Posterior pelvic floor disorders are caused by changes in the musculo-aponeurotic support of the pelvic floor. Defecography (radiographic dynamic rectal examination) provides precise information on anorectal and pelvic floor functions for patients with constipation, fecal incontinence and pelvic pain. These symptoms are more frequent in women, and some are related to obstetrical consequences. Little is known about the influence of gender in patients with pelvic floor disorders.
Radiological exploration of pelvic floor disorders is important to elucidate the pathophysiology and assist in deciding the therapeutic strategy. It is difficult to attribute a radiological abnormality as the direct cause of the symptoms. A better knowledge of gender difference in the prevalence of defecographic abnormalities appears to be useful.
To the best of the authors' knowledge, no specific study of defecography has been carried out to explore the gender difference in the diagnosis of defecographic abnormalities. The strength of this study was that it assessed gender in the diagnosis of defecographic abnormalities.
For the same complaint, defecographic abnormalities are different in men than in women: rectocele, enterocele and perineal descent at rest were less frequent in men than in women. Discussion of sex differences in pelvic floor disorders could probably help to assess more precisely these nosological entities. New examinations are also possible, such as magnetic resonance defecography.
There are several defecographic abnormalities. Rectocele is an outpouching of the anterior rectal wall. Enterocele is an herniation of the small bowel between the vagina and rectum. Perineal descent is an abnormal position of the perineum under the pubococcygeal line.
The results of this study are interesting, although the method of this study (defecography) is relatively old and slightly controversial. The results of this study raise issue concerning gender differences in pelvic floor disorders, and may bring a new dimension.
Peer reviewer: Reiji Sugita, MD, Department of Radiology,Sendai City Medical Center, 5-22-1, Tsurugaya, Miyagino-ku, Sendai 983-0824, Japan
S- Editor Tian L L- Editor Kerr C E- Editor Ma WH
| 1. | Burhenne HJ. Intestinal evacuation study: a new roentgenologic technique. Radiol Clin. 1964;33:79-84. [Cited in This Article: ] |
| 2. | Mahieu P, Pringot J, Bodart P. Defecography: II. Contribution to the diagnosis of defecation disorders. Gastrointest Radiol. 1984;9:253-261. [Cited in This Article: ] |
| 3. | Karasick S, Karasick D, Karasick SR. Functional disorders of the anus and rectum: findings on defecography. AJR Am J Roentgenol. 1993;160:777-782. [Cited in This Article: ] |
| 4. | Liu BH, Fang SW, Tong WD, Gong SG, Zhang SB. Role of pelvicography and colpocystodefecography in diagnosis of outlet obstructive constipation. Int J Colorectal Dis. 2005;20:317-320. [Cited in This Article: ] |
| 5. | Touchais JY, Koning E, Savoye-Collet C, Leroi AM, Denis P. [Role of defecography in female posterior pelvic floor abnormalities]. Gynecol Obstet Fertil. 2007;35:1257-1263. [Cited in This Article: ] |
| 6. | Kelvin FM, Maglinte DD, Hornback JA, Benson JT. Pelvic prolapse: assessment with evacuation proctography (defecography). Radiology. 1992;184:547-551. [Cited in This Article: ] |
| 7. | Agachan F, Pfeifer J, Wexner SD. Defecography and proctography. Results of 744 patients. Dis Colon Rectum. 1996;39:899-905. [Cited in This Article: ] |
| 8. | Mellgren A, Bremmer S, Johansson C, Dolk A, Udén R, Ahlbäck SO, Holmström B. Defecography. Results of investigations in 2,816 patients. Dis Colon Rectum. 1994;37:1133-1141. [Cited in This Article: ] |
| 9. | Rex DK, Lappas JC. Combined anorectal manometry and defecography in 50 consecutive adults with fecal incontinence. Dis Colon Rectum. 1992;35:1040-1045. [Cited in This Article: ] |
| 10. | Jorge JMN, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993;36:77-97. [Cited in This Article: ] |
| 11. | Jean F, Tanneau Y, Le Blanc-Louvry I, Leroi AM, Denis P, Michot F. Treatment of enterocele by abdominal colporectosacropexy - efficacy on pelvic pressure. Colorectal Dis. 2002;4:321-325. [Cited in This Article: ] |
| 12. | Savoye-Collet C, Savoye G, Koning E, Dacher JN. Defecographic disorders in anal incontinent women: relation to symptoms and anal endosonographic patterns. Scand J Gastroenterol. 2005;40:141-146. [Cited in This Article: ] |
| 13. | Savoye-Collet C, Koning E, Dacher JN. Radiologic evaluation of pelvic floor disorders. Gastroenterol Clin North Am. 2008;37:553-567, viii. [Cited in This Article: ] |
| 14. | Cavallo G, Salzano A, Grassi R, Zanatta P, Tuccillo M. Rectocele in males: clinical, defecographic, and CT study of singular cases. Dis Colon Rectum. 1991;34:964-966. [Cited in This Article: ] |
| 15. | Chen HH, Iroatulam A, Alabaz O, Weiss EG, Nogueras JJ, Wexner SD. Associations of defecography and physiologic findings in male patients with rectocele. Tech Coloproctol. 2001;5:157-161. [Cited in This Article: ] |
| 16. | Wang J, Luo MH, Qi QH, Dong ZL. Prospective study of biofeedback retraining in patients with chronic idiopathic functional constipation. World J Gastroenterol. 2003;9:2109-2113. [Cited in This Article: ] |
| 17. | Parks AJ. Anorectal incontinence. J R Soc Med. 1975;68:21-30. [Cited in This Article: ] |
| 18. | Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI. Anal-sphincter disruption during vaginal delivery. N Engl J Med. 1993;329:1905-1911. [Cited in This Article: ] |
| 19. | Kamm MA. Obstetric damage and faecal incontinence. Lancet. 1994;344:730-733. [Cited in This Article: ] |
| 20. | Lapalus MG, Henry L, Barth X, Mellier G, Gautier G, Mion F, Damon H. [Enterocele: clinical risk factors and association with others pelvic floor disorders (about 544 defecographies)]. Gynecol Obstet Fertil. 2004;32:595-600. [Cited in This Article: ] |
| 21. | Savoye-Collet C, Savoye G, Koning E, Leroi AM, Dacher JN. Defecography in symptomatic older women living at home. Age Ageing. 2003;32:347-350. [Cited in This Article: ] |
| 22. | Felt-Bersma RJ, Luth WJ, Janssen JJ, Meuwissen SG. Defecography in patients with anorectal disorders. Which findings are clinically relevant? Dis Colon Rectum. 1990;33:277-284. [Cited in This Article: ] |
| 23. | Ott DJ, Donati DL, Kerr RM, Chen MY. Defecography: results in 55 patients and impact on clinical management. Abdom Imaging. 1994;19:349-354. [Cited in This Article: ] |
| 24. | Hiltunen KM, Kolehmainen H, Matikainen M. Does defecography help in diagnosis and clinical decision-making in defecation disorders? Abdom Imaging. 1994;19:355-358. [Cited in This Article: ] |
| 25. | Wiermsa TG, Mulder CJ, Rieders JW. Dynamic rectal examination : its significant clinical value. Endoscopy. 1997;29:462-471. [Cited in This Article: ] |
| 26. | Harvey JC, Halligan S, Bartram CI, Hollings N, Sahdev A, Kingston K. Evacuation proctography: a prospective study of diagnostic and therapeutic effects. Radiology. 1999;211:223-227. [Cited in This Article: ] |
| 27. | Mahieu P, Pringot J, Bodart P. Defecography: I. Description of a new procedure and results in normal patients. Gastrointest Radiol. 1984;9:247-251. [Cited in This Article: ] |
| 28. | Shorvon PJ, McHugh S, Diamant NE, Somers S, Stevenson GW. Defecography in normal volunteers: results and implications. Gut. 1989;30:1737-1749. [Cited in This Article: ] |
| 29. | Müller-Lissner SA, Bartolo DC, Christiansen J, Ekberg O, Goei R, Höpfner W, Infantino A, Kuijpers HC, Selvaggi F, Wald A. Interobserver agreement in defecography--an international study. Z Gastroenterol. 1998;36:273-279. [Cited in This Article: ] |
| 30. | Choi JS, Wexner SD, Nam YS, Mavrantonis C, Salum MR, Yamaguchi T, Weiss EG, Nogueras JJ, Yu CF. Intraobserver and interobserver measurements of the anorectal angle and perineal descent in defecography. Dis Colon Rectum. 2000;43:1121-1126. [Cited in This Article: ] |
| 31. | Dvorkin LS, Gladman MA, Epstein J, Scott SM, Williams NS, Lunniss PJ. Rectal intussusception in symptomatic patients is different from that in asymptomatic volunteers. Br J Surg. 2005;92:866-872. [Cited in This Article: ] |
| 32. | Pannu HK, Kaufman HS, Cundiff GW, Genadry R, Bluemke DA, Fishman EK. Dynamic MR imaging of pelvic organ prolapse: spectrum of abnormalities. Radiographics. 2000;20:1567-1582. [Cited in This Article: ] |
| 33. | Stoker J, Bartram CI, Halligan S. Imaging of the posterior pelvic floor. Eur Radiol. 2002;12:779-788. [Cited in This Article: ] |