Published online Apr 14, 2014. doi: 10.3748/wjg.v20.i14.4106
Revised: February 13, 2014
Accepted: March 6, 2014
Published online: April 14, 2014
Primary squamous cell carcinoma of the rectum is a rare malignancy, and the discrete dual lesions of rectum are even rarer. There is currently no effective and satisfactory treatment for this disease. Here we report a case of an elderly female with bi-primary squamous cell carcinoma of the rectum treated with radical resection and radiotherapy. The patient is still alive 43 mo after the initial curative resection of the tumor. We suggest that surgery as the primary treatment followed by concomitant radiotherapy may be an effective protocol for elderly patients with rectal squamous cell carcinoma.
Core tip: Primary squamous cell carcinoma of the rectum is a rare malignancy, and the discrete dual lesions of rectum are even rarer. Our patient is still alive after surgery as the primary treatment followed by concomitant radiotherapy. It was suggested that surgery combined with radiotherapy may be an effective treatment strategy for patients with rectal squamous cell carcinoma, especially for elderly patients who cannot tolerate chemotherapy.
- Citation: Wang JF, Wang ZX, Xu XX, Wang C, Liu JZ. Primary rectal squamous cell carcinoma treated with surgery and radiotherapy. World J Gastroenterol 2014; 20(14): 4106-4109
- URL: https://www.wjgnet.com/1007-9327/full/v20/i14/4106.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i14.4106
Colorectal squamous cell carcinoma (SCC) is an extremely rare malignancy of the gastrointestinal tract. Since more than 90% of colorectal diseases are adenocarcinomas, very little information is available in the literature about the etiology, prognosis and optimal treatment of this malignancy. It was reported that the survival rate of rectal SCC is by far lower than that of adenocarcinoma[1]. A multidisciplinary approach has been recommended, and surgical resection should be performed in patients with localized disease if possible. Neoadjuvant/adjuvant therapy of rectal cancer can reduce the high risk of locoregional recurrence. In the present study, we report a case of a primary SCC involving two parts of the rectum, which was treated surgically followed by adjuvant radiation.
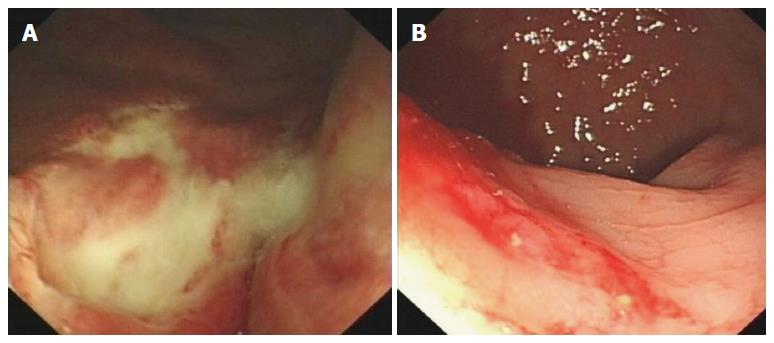
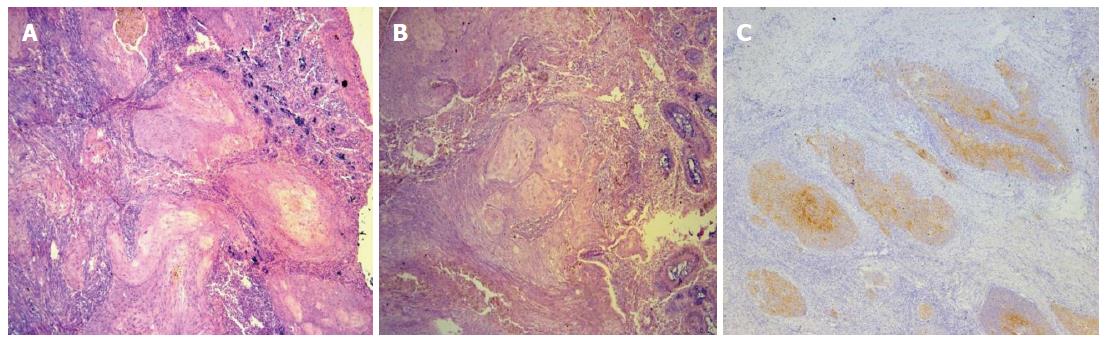
A 75-year-old female patient was admitted to the surgical department of our center in March 2010 because of perianal discomfort and tenesmus for one and half month. She experienced 2.5 kg weight loss during the past three months. She is a nonsmoker and does not drink. Rectal examination revealed a mass of of 1.5 cm arising 3 cm from the anal edge and another 3.5 cm mass arising 7 cm from the anal edge (Figure 1). Computed tomography (CT) scan of the chest, abdomen and pelvis was negative for distal metastases. The rectal examination was performed using colonoscopy, and biopsies revealed squamous cell carcinoma of the rectum. She then underwent combined abdominal perineal resection of the rectum (Miles operation), and pathologic examination found a moderately-poorly differentiated SCC of the rectum (Figure 2) infiltrating the serosa into the soft tissue of the right pelvic cavity. The margins of the excised tissue were tumor free. Multiple regional lymph nodes seen in the full-thickness excision of the lesion revealed no evidence of invasion. The tumor was found to be T4N0M0 in stage. Postoperatively, the patient was treated with a megavoltage linear accelerator (6 MV) in prone position; and a 2-fields technique (AP-PA fields) was used. The upper border of the radiation field was at the L4/L5 junctions; and the inferior border was at the lower edge of ischial tuberosity including the surgical scar. The left border and the right border included a 1.5-cm margin on the pelvic brim. The radiotherapy doses were specified at the intersection of the central axis of the beams in the pelvis. The dose of 45 Gy was delivered to the pelvis in 25 fractions over 5 wk. A daily dose of 1.8 Gy was given through the AP-PA fields. After the treatment, the patient achieved complete remission confirmed by colonoscopy and computed CT scan of the chest, abdomen and pelvis during the follow-up. At the time of writing this report, the patient had survived 43 mo after treatment, with no clinical evidence of recurrence.
Squamous cell carcinoma of the rectum is a relatively rare tumor with a reported incidence of only 0.1%-0.2% of all rectal tumors[2]. This kind of cancer is definitely more common in the anus than in the rectum. The border-line of the two carcinoma types is marked by the 10-12 mm thin transitional layer of the anus, where the cylindrical epithelium changes over to the squamous epithelium[3]. Our case is extremely rare, for the patient presented two lesions in the rectum, both of which were located > 2 cm from the anal edge.
The pathogenesis of these tumors is still unclear. The most possible assumption is that multipotent basal cells proliferate to squamous cells, and the presence of these undifferentiated basal cells at the base of normal mucosal crypts has been previously demonstrated by Lorenzsonn et al[4]. Another possible explanation postulates that ectodermal cells may migrate to the rectum during the embryonic phase and aberrantly proliferate in response to stimuli[5]. Both theories are based on the theory of chronic irritation, e.g., by ulcerative colitis[6], and infection of human papillomavirus (HPV)[7,8], or other viruses such as human immunodeficiency virus[7,9].
The established criteria for a diagnosis of primary SCC of the rectum are as follows[5]: (1) metastases from other sites (e.g., lung SCC) must be ruled out; (2) a squamous cell-lined fistula must not involve the affected bowel; and (3) an SCC of the anus extending to the rectum must be excluded. Immunochemistry is helpful in diagnosing SCC using the markers, including cytokeratins AE1/AE3, 34BE12, CK5 and involucrin in order to differentiate it from other undifferentiated small cell tumors[10].
The optimal treatment for rectal SCC has not been well established due to the rarity of the disease. Traditionally, surgical resection of the affected rectum was considered to be the standard treatment. Local excision is appropriate in selected cases of stage T1 (invasion to the mucosa or submucosa) cancers or possibly stage T2 (invasion to the muscularis propria) lesions. It was reported that T2 lesions particularly require close follow-up, as recurrence after local excision can be as high as 20%[11]. More recently, neoadjuvant radiotherapy (local control of the disease and downstaging) or adjuvant chemo- and/or radio-therapy has been advocated as an alternative primary treatment for SCC with acceptable local control in about 60% of patients[12-16]. Surgery was relegated to the role of salvage therapy for cases that do not respond to radiotherapy[2,3]. However, considering the limited number, the rarity of this condition and the retrospective nature of the series, large randomized prospective trials are needed to identify the role of only chemoradiotherapy. Above all, it is recommended that surgical resection is the treatment of choice, although radiation and chemotherapy can be useful in treating node-positive patients, poorly differentiated cancers and advanced disease. Due to the relatively high risk of locoregional recurrence of rectal cancer of T4N0M0 patients, combined adjuvant therapy after surgery was recommended. However, considering patient’s rejection of chemotherapy and the poor toleration of the old age to chemotherapy, we proposed the individualized treatment of radiotherapy after local excision, which yielded a complete response. The patient remained disease-free for 43 mo after treatment. The therapeutic approach with surgery as the primary treatment followed by combined radiotherapy, may be necessary in order to improve the survival and prognosis of patients with local lesions, especially for those of old age.
The authors gratefully acknowledge the technical staff for their help in the procurement of tumor tissue samples. We also thank the pathologists from the Department of Pathology for the histopathological assessment of the tumor tissues.
A 75-year-old female with one and a half month history of perianal discomfort and tenesmus.
A 2.5 kg weight loss occurred during the past three months and a tumor was found in digital rectal examination.
Colon cancer, rectum adenocarcinoma, colorectal polyps.
Carcinoembryonic antigen 2.67 μg/L; squamous cell carcinoma (SCC) 13.9 μg/L; blood routine, liver and kidney function tests were within normal limits.
Rectal examination revealed a mass of 1.5 cm arising 3 cm from the anal edge and another 3.5 cm mass arising 7 cm from the anal edge.
Pathology of the surgically resected tissues revealed a squamous cell carcinoma.
The patient was treated with combined abdominal-perineal resection of the rectum followed by radiotherapy of totally 4500 cGy in fractions to pelvis.
Colorectal SCC is an extremely rare malignancy of the gastrointestinal tract, and very little information is available in the literature about the etiology, prognosis and optimal treatment of this malignancy.
Colorectal SCC is a very rare disease and selection of proper treatment is a complex process. However, surgical resection and adjuvant radiotherapy can be considered as a better treatment strategy for patients with early colorectal SCC, especially for those of old age who cannot tolerate the side effect of chemotherapy.
In this work, authors reported a case of a 75-year old female patient with bi-primary squamous cell carcinoma. The patient was treated with a curative surgery, followed by radiotherapy with a radiation dose of 45 Gy. The study reported that the patient is no-evidence-disease at the time of writing, 43 months after treatment. Generally, the work presents an interesting case. However, there are several weaknesses to be addressed.
P- Reviewers: Assouline A, Chang Z, Plataniotis G S- Editor: Gou SX L- Editor: A E- Editor: Liu XM
| 1. | Kang H, O’Connell JB, Leonardi MJ, Maggard MA, McGory ML, Ko CY. Rare tumors of the colon and rectum: a national review. Int J Colorectal Dis. 2007;22:183-189. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 95] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 2. | Pikarsky AJ, Belin B, Efron J, Woodhouse S, Weiss EG, Wexner SD, Nogueras JJ. Squamous cell carcinoma of the rectum in ulcerative colitis: case report and review of the literature. Int J Colorectal Dis. 2007;22:445-447. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Smigielski J, Rychter A, Fijuth J, Brocki M. Advanced anal squamous cell carcinoma -- radiotherapy or surgery. Chirurgia (Bucur). 2012;107:626-630. [PubMed] [Cited in This Article: ] |
| 4. | Lorenzsonn V, Trier JS. The fine structure of human rectal mycosa. The epithelial lining of the base of the crypt. Gastroenterology. 1968;55:88-101. [PubMed] [Cited in This Article: ] |
| 5. | Williams GT, Blackshaw AJ, Morson BC. Squamous carcinoma of the colorectum and its genesis. J Pathol. 1979;129:139-147. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 152] [Cited by in F6Publishing: 149] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Michelassi F, Montag AG, Block GE. Adenosquamous-cell carcinoma in ulcerative colitis. Report of a case. Dis Colon Rectum. 1988;31:323-326. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 39] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Matsuda A, Takahashi K, Yamaguchi T, Matsumoto H, Miyamoto H, Kawakami M, Kawachi H, Suzuki H, Furukawa K, Tajiri T. HPV infection in an HIV-positive patient with primary squamous cell carcinoma of rectum. Int J Clin Oncol. 2009;14:551-554. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Audeau A, Han HW, Johnston MJ, Whitehead MW, Frizelle FA. Does human papilloma virus have a role in squamous cell carcinoma of the colon and upper rectum. Eur J Surg Oncol. 2002;28:657-660. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 56] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Salama JK, Mell LK, Schomas DA, Miller RC, Devisetty K, Jani AB, Mundt AJ, Roeske JC, Liauw SL, Chmura SJ. Concurrent chemotherapy and intensity-modulated radiation therapy for anal canal cancer patients: a multicenter experience. J Clin Oncol. 2007;25:4581-4586. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 207] [Cited by in F6Publishing: 220] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 10. | Anagnostopoulos G, Sakorafas GH, Kostopoulos P, Grigoriadis K, Pavlakis G, Margantinis G, Vugiouklakis D, Arvanitidis D. Squamous cell carcinoma of the rectum: a case report and review of the literature. Eur J Cancer Care (Engl). 2005;14:70-74. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Dyson T, Draganov PV. Squamous cell cancer of the rectum. World J Gastroenterol. 2009;15:4380-4386. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 69] [Cited by in F6Publishing: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 12. | Jeong BG, Kim DY, Kim SY. Concurrent chemoradiotherapy for squamous cell carcinoma of the rectum. Hepatogastroenterology. 2013;60:512-516. [PubMed] [Cited in This Article: ] |
| 13. | Wang ML, Heriot A, Leong T, Ngan SY. Chemoradiotherapy in the management of primary squamous-cell carcinoma of the rectum. Colorectal Dis. 2011;13:296-301. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Sanal SM, Sivrikoz ON, Karapolat I, Karademir S. Complete clinical response in squamous cell carcinoma of the rectum with liver metastases. J Clin Oncol. 2011;29:e806-e808. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Rasheed S, Yap T, Zia A, McDonald PJ, Glynne-Jones R. Chemo-radiotherapy: an alternative to surgery for squamous cell carcinoma of the rectum--report of six patients and literature review. Colorectal Dis. 2009;11:191-197. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 16. | Theodosopoulos TK, Marinis AD, Dafnios NA, Vassiliou JG, Samanides LD, Carvounis EE, Smyrniotis VE. Aggressive treatment of metastatic squamous cell carcinoma of the rectum to the liver: a case report and a brief review of the literature. World J Surg Oncol. 2006;4:49. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |