Published online May 21, 2014. doi: 10.3748/wjg.v20.i19.5930
Revised: March 4, 2014
Accepted: April 5, 2014
Published online: May 21, 2014
Lung cancer is a common malignancy in the world; however symptomatic colonic metastasis from primary lung cancer is rare. A 64-year-old man was originally found poorly differentiated squamous cell carcinoma of right lung and received right lower lobectomy and lymph node dissection. Three years later, the patient presented to our emergency room with the symptom of upper abdominal pain and weight loss. Abdominal palpation and computed tomography scan of the abdomen revealed a large mass measuring 7.6 cm × 8.5 cm in the ascending colon. Colonoscopy and biopsy revealed poorly differentiated squamous cell carcinoma with similar morphological pattern to that of the previous lung cancer. Chemotherapy was given and the patient died 5 mo later. Lung cancer metastatic to the colon confers a poor prognosis: overall survival ranged from 5 wk to 1 year, with a median survival of 3 mo after the diagnosis of the colonic metastasis.
Core tip: Lung cancer with colonic metastasis is a rare condition, accounting for only 0.5% of lung cancer cases. Symptomatic colonic metastases are often emergent and colonoscopy with biopsy can make further diagnosis. Herein we report a case of patient with upper abdominal pain and weight loss after lung cancer resection. Subsequent colonoscopy and pathology confirmed poorly-differrentiated squamous cell carcinoma due to colonic metastasis of lung cancer. The patient improved after receiving chemotherapy but died from rectal bleeding. We report the case for its rarity and emphasize disease management after prompt clinical and pathological analyses.
- Citation: Lou HZ, Wang CH, Pan HM, Pan Q, Wang J. Colonic metastasis after resection of primary squamous cell carcinoma of the lung: A case report and literature review. World J Gastroenterol 2014; 20(19): 5930-5934
- URL: https://www.wjgnet.com/1007-9327/full/v20/i19/5930.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i19.5930
Lung cancer is a common malignancy in the world; however symptomatic colonic metastasis from primary lung cancer is rare. Clinically, patients may present with symptoms of abdominal pain, obstruction, bowel perforation, and lower gastrointestinal bleeding. In this report, we describe a rare case of symptomatic colonic metastasis from squamous cell carcinoma of the lung and with literature review.
A 64-year-old man originally presented to local hospital for left chest pain in May 2009. At that time, he underwent a contrast-enhanced computed tomography (CT) scan of the chest,which showed a mass in the right lower lobe of lung. Flexible bronchoscopy identified focal areas of thickening in the bronchus of right lower lobe. Histopathologic examination revealed a poorly differentiated squamous cell carcinoma (SCC) of the lung. Then he underwent right lower lobectomy and lymph node dissection.The final pathologic diagnosis of the tumor was stage II poorly differentiated SCC. Margins were negative and no involved lymph nodes. The patient refused any adjuvant chemotherapy or radiation therapy after surgery.
In February 2012, nearly three years after his initial lung cancer diagnosis, the patient presented to our emergency room with the symptom of upper abdominal pain and weight loss. On physical examination at admission, the patient was fully alert and oriented, afebrile. His vital parameters were normal. There was slight pallor, no peripheral lymphadenopathy or pedal edema. Abdominal palpation revealed a large mass in the right upper quadrant. The mass was tender on palpation, but there was no rebound tenderness or guarding. Rest of the systemic examination was unremarkable. On laboratory tests,hemoglobin was 10.6 g/dL, blood count showed slight leukocytosis with neutrophils elevated. Liver and renal functions were normal.Fecal occult blood test was positive.
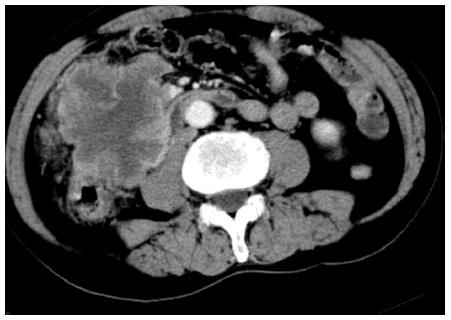
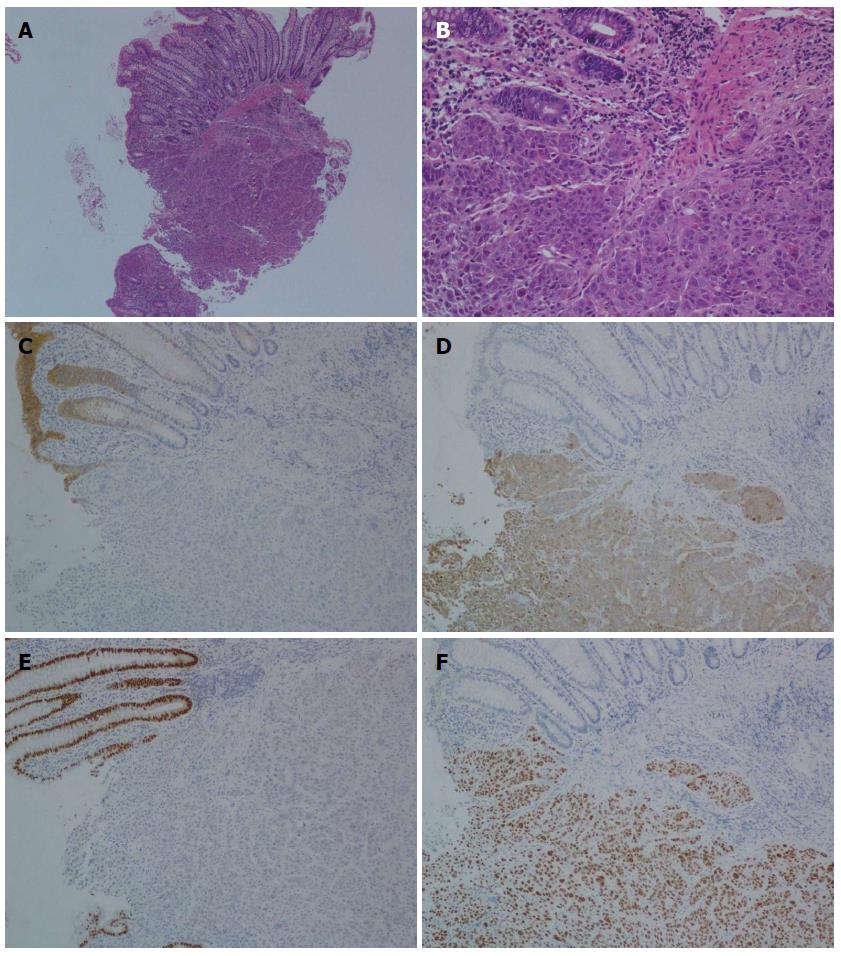
CT scan of the abdomen revealed a large mass measuring 7.6 cm × 8.5 cm in the ascending colon with heterogeneous enhancement (Figure 1). Subsequent colonoscopy disclosed a large ulcerated lesion in the ascending colon, and biopsy revealed poorly differentiated SCC with similar morphological pattern to that of the previous lung cancer. Furthermore, immune histochemical results of the tissue specimen were positive for CK5/6 and p63, but negative for CDX2 and CK20 (Figure 2). Upon review by our hospital’s tumor board, it was concluded that these results were consistent with primary lung cancer. Then chemotherapy with intravenous cisplatin and oral S-1 every 5 wk was initiated and a total of 2 cycles were given. The patient improved remarkably after 2 cycles of chemotherapy. CT scan of the abdomen showed significant reduction in the abdominal mass. Just before the 3rd cycle, the patient developed rectal bleeding with bright red blood in stool. He was treated with somatostatin and hemostatic drugs and symptoms relieved soon. But three weeks later the patient refused further chemotherapy and was discharged from the hospital. The patient died 5 mo after diagnosis.
Lung cancer is one of the most common primary malignancies, and nearly 50% have distal metastasis at the time of diagnosis[1,2]. The preferential sites of distal metastasisare the liver, adrenal gland, bone, and brain[3,4]. Gastrointestinal metastasis of primary lung cancer is considered to be rare. The overall incidence of primary lung cancer metastatic to gastrointestinal tract is about 4.7%-14.0% at autopsy[1,5]. Symptomatic gastrointestinal metastasis of lung cancer is 1.77% (6/339) as reported by Yang et al[6]. Lung cancer metastatic to the colon are very rare, accounting for only 0.5%of lung cancer cases[5].
Gastrointestinal metastases from lung cancer are often asymptomatic. Symptomatic colonic metastasis is very rare and only a few cases were reported in the English literature. After review of the literature, a total of only 12 such cases were identified since 1970 (Table 1)[2-4,6-13]. In these patients, the mean age was 64.4 years and all patients were male. Abdominal pain and anemia are the most common symptoms[1,10]. Other symptoms like intestinal obstruction, lower GI bleeding, bowel perforation, or GI fistula may occur[2,10].These findings can occur synchronously or before the diagnosis of lung cancer, but more frequently after the diagnosis of primary lung cancer[6].
| Case | Year | Age | Sex | Site of metastasis | Pathology type of lung cancer | Location of lung cancer | Interval time to diagnosis | Survival |
| 1 | 1978 | 52 | Male | Sigmoid colon | Poorly differentiated squamous cell carcinoma | Left upper lobe | Same time | > 1yr |
| 2 | 1978 | 57 | Male | Sigmoid colon | Squamous cell carcinoma | Left lower lobe | 2 yr later | 1 yr |
| 3 | 1980 | 63 | Male | Sigmoid colon | Large cell carcinoma | Left upper lobe | 1 mo | NA |
| 4 | 1988 | 69 | Male | Ascending colon | Small cell carcinoma | Right medial lobe | Same time | 2 mo |
| 5 | 1998 | 69 | Male | Sigmoid colon | Squamous cell carcinoma | Right main bronchus | 9 mo | 2 mo |
| 6 | 2001 | 68 | Male | Sigmoid colon | Squamous cell carcinoma | Right lower lobe | 10 wk | 6 mo |
| 7 | 2002 | 73 | Male | Entire colon | Large cell carcinoma | Right lower lobe | Same time | 3 mo |
| 8 | 2006 | 60 | Male | Ascending colon | Squamous cell carcinoma | Left upper lobe | Same time | NA |
| 9 | 2006 | 57 | Male | Caecum | Small cell carcinoma | Left upper lobe | 645 d | 70 d |
| 10 | 2008 | 74 | Male | Descending colon | Squamous cell carcinoma | Right upper lobe | Same time | 23 wk |
| 11 | 2008 | 59 | Male | Caecum | Small cell carcinoma | Left hilar mass | Same time | NA |
| 12 | 2010 | 53 | Male | Descending colon | Adenocarcinoma | Left lower lobe | Same time | 6 mo |
| 32 | 2012 | 67 | Male | Descending colon | Squamous cell carcinoma | Right lower lobe | 32 mo | 5 mo |
Symptomatic colonic metastases are often emergent and intended to undergo emergent computed tomography .Colonoscopy with biopsy can make further diagnosis. PET-FDG has become useful in patients with potentially resectable non-small cell lung cancer[14,15]. In patients with clinical stage III disease, PET scanning willdetect extrathoracic metastases in approximately 25% of patients[16,17]. Recently, case of colonic metastasis from lung cancer has been assessed by PET-CT imaging[11]. PET-CT scanning may reveal a higher incidence of colonic metastases than previously suspected. However, the role of PET-CT in the diagnosis of gastrointestinal metastasis from lung cancer is still unclear because of few clinical data.
The histological type of lung cancer that causes gastrointestinal metastasis varies according to different series[6].The most common type was squamous cell carcinoma which accounting for colonic metastasis in more than 50% of cases in our review. But the study of Stenbygaard et al[18] showed adenocarcinoma was more prominent. The pathologic results of colonic metastasise usually consistent with the primary lung cancer. These findings can be confirmed by immunohistochemistry. Lung carcinomas usually show positive staining forCK5/6 or p63 and negative staining for CK20 and CDX-2, whereas colon adenocarcinoma is typicallyCK5/6 or p63 negative and CDX-2 or CK20 positive[19]. CDX-2 is a highly specific and sensitive marker for gastrointestinal adenocarcinoma andcan be used to differentiate from metastasis of lung cancer[20].
Secondary colonic involvement from lung cancer suggests widespread dissemination and is associated with a poor prognosis. According to our review, after the detection of colonic metastasis secondary to primary lung cancer, survival times ranged from 5 wk to 1 year (Table 1), with most patients dying within 6 mo. Treatment of colonic metastasis depends on the extent of the disease and the nature of the initial presentation. The most important point is which lesion should be treated first-the colonic metastasis or the primary lung cancer? In case of a complicated colonic lesion (obstruction, bleeding or perforation), proper surgery for colonic metastasis provides excellent palliation, increases the quality of life and shortens the time of hospitalization[9,13].Chemotherapy is useful in selected patients. In our case sufficient palliation was achieved with chemotherapy. This patient survived for a further 5 mo after diagnosis.
Although lung cancer metastatic to colon is rare, it should be included in the differential diagnosis for any patient with colonic tumor.Accurate differentiation is necessary because treatment differs significantly for patients with colonic metastasis of lung cancer, as compared with patients with primary colon cancer. Lung cancer metastasis to the colon confers a poor prognosis and early diagnosis can prevent further complications.
The patient presented with the symptom of upper abdominal pain and weight loss.
Clinical diagnosis was colonic metastasis of primary squamous cell carcinoma of lung.
Differential diagnosis of primary colon carcinoma, malignant lymphoma, Crohn disease and diverticulosis should be considered.
On laboratory tests, hemoglobin was 10.6 g/dL, blood count showed slight leukocytosis with neutrophils elevated.
Computed tomography scan revealed a large mass in the ascending colon with heterogeneous enhancement and colonoscopy disclosed a large ulcerated lesion in the ascending colon.
Pathology with Hematoxylin and eosin stain and immunohistochemistry revealed poorly differentiated squamous cell carcinoma.
Chemotherapy with intravenous cisplatin and oral S-1 every 5 wk was initiated and the patient improved remarkably after 2 cycles of chemotherapy.
Most patients presented with symptoms like intestinal obstruction, lower glycemic index or glycaemic index (GI) bleeding, bowel perforation, or GI fistula and pathology with immunohistochemistry can confirm the diagnosis.
Although lung cancer metastatic to colon is rare, it should be included in the differential diagnosis for any patient with colonic tumor. Accurate diagnosis and chemotherapy with cisplatin and S-1 may help to manage the condition but the prognosis is still very poor.
In this manuscript “Colonic metastasis after resection of primary squamous cell carcinoma of the lung: a case report and literature review”, Lou et al reported a case of symptomatic colonic metastasis from squamous cell carcinoma of the lung.
P- Reviewers: Flier SN, Timmons S S- Editor: Qi Y L- Editor: A E- Editor: Liu XM
| 1. | Antler AS, Ough Y, Pitchumoni CS, Davidian M, Thelmo W. Gastrointestinal metastases from malignant tumors of the lung. Cancer. 1982;49:170-172. [PubMed] [Cited in This Article: ] |
| 2. | Hirasaki S, Suzuki S, Umemura S, Kamei H, Okuda M, Kudo K. Asymptomatic colonic metastases from primary squamous cell carcinoma of the lung with a positive fecal occult blood test. World J Gastroenterol. 2008;14:5481-5483. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 19] [Cited by in F6Publishing: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Brown KL, Beg RA, Demany MA, Lacerna MA. Rare metastasis of primary bronchogenic carcinoma to sigmoid colon: report of a case. Dis Colon Rectum. 1980;23:343-345. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 18] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Carroll D, Rajesh PB. Colonic metastases from primary squamous cell carcinoma of the lung. Eur J Cardiothorac Surg. 2001;19:719-720. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 37] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | McNeill PM, Wagman LD, Neifeld JP. Small bowel metastases from primary carcinoma of the lung. Cancer. 1987;59:1486-1489. [PubMed] [Cited in This Article: ] |
| 6. | Yang CJ, Hwang JJ, Kang WY, Chong IW, Wang TH, Sheu CC, Tsai JR, Huang MS. Gastro-intestinal metastasis of primary lung carcinoma: clinical presentations and outcome. Lung Cancer. 2006;54:319-323. [PubMed] [Cited in This Article: ] |
| 7. | Smith HJ, Vlasak MG. Metastasis to the colon from bronchogenic carcinoma. Gastrointest Radiol. 1978;2:393-396. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 21] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Wegener M, Börsch G, Reitemeyer E, Schäfer K. Metastasis to the colon from primary bronchogenic carcinoma presenting as occult gastrointestinal bleeding--report of a case. Z Gastroenterol. 1988;26:358-362. [PubMed] [Cited in This Article: ] |
| 9. | Bastos I, Gomes D, Gouveia H, de Freitas D. Colonic metastasis of a lung carcinoma with ileocolic fistula. J Clin Gastroenterol. 1998;26:348. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | John AK, Kotru A, Pearson HJ. Colonic metastasis from bronchogenic carcinoma presenting as pancolitis. J Postgrad Med. 2002;48:199-200. [PubMed] [Cited in This Article: ] |
| 11. | Stinchcombe TE, Socinski MA, Gangarosa LM, Khandani AH. Lung cancer presenting with a solitary colon metastasis detected on positron emission tomography scan. J Clin Oncol. 2006;24:4939-4940. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 29] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Lau CP, Leung WK. Caecal metastasis from a primary small-cell lung carcinoma. Hong Kong Med J. 2008;14:152-153. [PubMed] [Cited in This Article: ] |
| 13. | Weng MW, Wang HC, Chiou JC, Lin SL, Lai RS. Colonic metastasis from a primary adenocarcinoma of the lung presenting with acute abdominal pain: a case report. Kaohsiung J Med Sci. 2010;26:40-44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Gupta NC, Tamim WJ, Graeber GG, Bishop HA, Hobbs GR. Mediastinal lymph node sampling following positron emission tomography with fluorodeoxyglucose imaging in lung cancer staging. Chest. 2001;120:521-527. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 130] [Cited by in F6Publishing: 134] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 15. | Poncelet AJ, Lonneux M, Coche E, Weynand B, Noirhomme P. PET-FDG scan enhances but does not replace preoperative surgical staging in non-small cell lung carcinoma. Eur J Cardiothorac Surg. 2001;20:468-474; discussion 474-475. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Eschmann SM, Friedel G, Paulsen F, Budach W, Harer-Mouline C, Dohmen BM, Bares R. FDG PET for staging of advanced non-small cell lung cancer prior to neoadjuvant radio-chemotherapy. Eur J Nucl Med Mol Imaging. 2002;29:804-808. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 55] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | Detterbeck FC, Falen S, Rivera MP, Halle JS, Socinski MA. Seeking a home for a PET, part 2: Defining the appropriate place for positron emission tomography imaging in the staging of patients with suspected lung cancer. Chest. 2004;125:2300-2308. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 55] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Stenbygaard LE, Sørensen JB. Small bowel metastases in non-small cell lung cancer. Lung Cancer. 1999;26:95-101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Jagirdar J. Application of immunohistochemistry to the diagnosis of primary and metastatic carcinoma to the lung. Arch Pathol Lab Med. 2008;132:384-396. [PubMed] [Cited in This Article: ] |
| 20. | Levine PH, Joutovsky A, Cangiarella J, Yee H, Simsir A. CDX-2 expression in pulmonary fine-needle aspiration specimens: a useful adjunct for the diagnosis of metastatic colorectal adenocarcinoma. Diagn Cytopathol. 2006;34:191-195. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |