Published online Apr 7, 2015. doi: 10.3748/wjg.v21.i13.3978
Peer-review started: July 22, 2014
First decision: September 27, 2014
Revised: October 10, 2014
Accepted: November 7, 2014
Article in press: November 11, 2014
Published online: April 7, 2015
AIM: To evaluate the technique of transpancreatic septotomy (TS) for cannulating inaccessible common bile ducts in endoscopic retrograde cholangiopancreatography (ERCP).
METHODS: Between May 2012 and April 2013, 1074 patients were referred to our department for ERCP. We excluded 15 patients with previous Billroth II gastrectomy, Roux-en-Y anastomosis, duodenal stenosis, or duodenal papilla tumor. Among 1059 patients who underwent ERCP, there were 163 patients with difficult bile duct cannulation. Pancreatic guidewire or pancreatic duct plastic stent assistance allowed for successful ERCP completion in 94 patients. We retrospectively analyzed clinical data from 69 failed patients (36 transpancreatic septotomies and 33 needle-knife sphincterotomies).
RESULTS: Of the 69 patients who underwent precut papillotomy, common bile duct cannulation was successfully achieved in 67. The success rates in the TS and needle knife sphincterotomy (NKS) groups were 97.2% (35/36) and 96.9% (32/33), respectively, which were not significantly different (P > 0.05). Complications occurred in 11 cases, including acute pancreatitis (n = 6), bleeding (n = 2), and cholangitis (n = 3). The total frequency of complications in the TS group was lower than that in the NKS group (8.3% vs 24.2%, P < 0.05).
CONCLUSION: Pancreatic guidewire or pancreatic duct plastic stent assistance improves the success rate of selective bile duct cannulation in ERCP. TS and NKS markedly improve the success rate of selective bile duct cannulation in ERCP. TS precut is safer as compared with NKS.
Core tip: In this study, we describe that pancreatic guidewire or pancreatic duct plastic stent assistance improves the success rate of selective bile duct cannulation in endoscopic retrograde cholangiopancreatography (ERCP). Transpancreatic septotomy (TS) and needle knife sphincterotomy (NKS) markedly improve the success rate of selective bile duct cannulation in ERCP. TS precut is safer and effective than NKS.
- Citation: Miao L, Li QP, Zhu MH, Ge XX, Yu H, Wang F, Ji GZ. Endoscopic transpancreatic septotomy as a precutting technique for difficult bile duct cannulation. World J Gastroenterol 2015; 21(13): 3978-3982
- URL: https://www.wjgnet.com/1007-9327/full/v21/i13/3978.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i13.3978
Endoscopic retrograde cholangiopancreatography (ERCP) is an important technique in the diagnosis and treatment of biliary and pancreatic diseases. Successful bile duct cannulation in ERCP is key to follow-up treatment. Biliary cannulation rates during ERCP exceed 90% in most large centers worldwide[1,2]. However, selective bile duct cannulation in ERCP is difficult to perform in patients with small duodenal papilla, papilla opening sclerosis, papilla looseness, peripapillary diverticulum or a history of Billroth II gastrectomy. Although a variety of catheters and guidewires are used to guide the knife, the failure rate of bile duct cannulation ranges from 5%-20%[3]. Prolonged or repeated attempts at cannulation in these patients increase the risk of ERCP related complications[2,4].
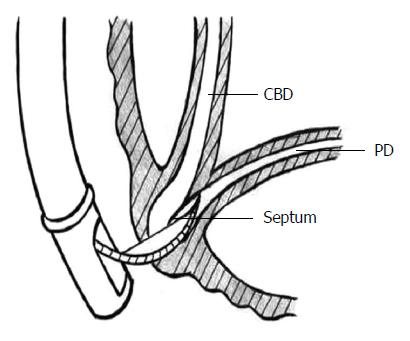
Pancreatic guidewire or stent placement can improve the success rate of bile duct cannulation during ERCP[5,6]. Endoscopic needle-knife precut papillotomy can also significantly increase ERCP cannulation success rate, but the complication rate is 6%-20%[7]. A thin septum between the pancreatic duct and the common bile duct has been reported (Figure 1)[8]; therefore, we hypothesized that difficult bile duct cannulation and repeated insertion into the pancreatic duct may be due to bile duct blockage by the septum in some cases. In the present study, a bow knife was used to cut the septum through the pancreatic duct toward the bile duct. Transpancreatic septotomy (TS) was compared with needle-knife sphincterotomy (NKS) during the same period to explore its clinical value.
From May 2012 to April 2013, 1074 patients were referred to our department for ERCP. Fifteen patients with a history of Billroth II gastrectomy, Roux-en-Y anastomosis, duodenal stenosis, or duodenal papilla tumor were excluded, and ERCP was performed in 1059 patients. Among these, 163 patients experienced difficult bile duct cannulation in ERCP. With the assistance of a pancreatic guidewire or plastic stent, 94 of the 163 patients had successful ERCP procedures. Of the other 69 patients with failed cannulation, 36 underwent TS (referred to as TS group) and 33 had NKS (referred to as NKS group). The TS group included 19 males and 17 females, and they ranged in age from 17 to 89 years, with an average of 59.5 years. The NKS group included 16 males sand 15 females, and they ranged in age from 17 to 85 years, with an average of 57.9 years. There was no significant statistical difference in etiology distribution or duodenal papilla morphology between the two groups (Tables 1 and 2).
| Etiology | TS | NKS | Total |
| Benign | 22 | 21 | 43 |
| Common bile duct stones | 9 | 8 | 17 |
| Cystic dilatation of the common bile duct | 1 | 1 | 2 |
| Cholangitis | 4 | 6 | 10 |
| SOD | 5 | 4 | 9 |
| Others | 3 | 2 | 5 |
| Malignant | 14 | 12 | 26 |
| Cholangiocarcinoma | 4 | 3 | 7 |
| Pancreatic cancer | 4 | 5 | 9 |
| Duodenal papilla tumor | 2 | 1 | 3 |
| Gallbladder carcinoma | 4 | 3 | 7 |
| Papilla morphology | TS | NKS |
| Small papilla | 5 | 6 |
| Sclerosis of papilla opening | 6 | 4 |
| Looseness of papilla | 11 | 9 |
| Peripapillary diverticulum | 7 | 8 |
| Normal papilla | 7 | 6 |
Side-view duodenoscope (Olympus TJF-260), needle knife and bow knife (Boston or COOK), and high-frequency surgical unit (ERBE CC80) were used.
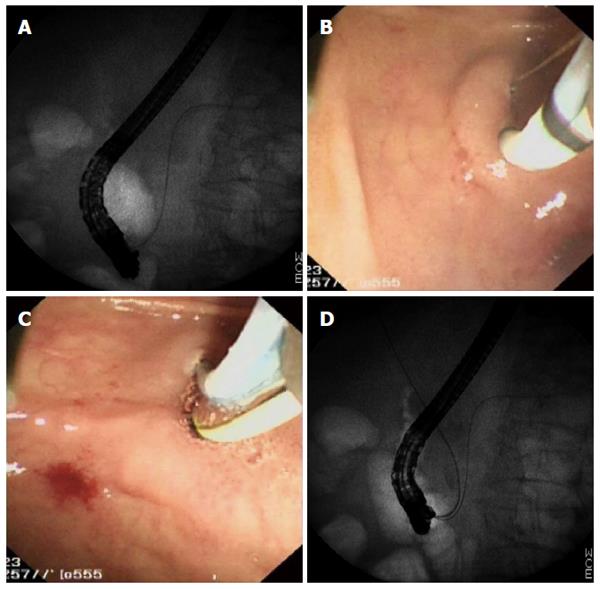
A duodenoscope was inserted into the duodenal papilla. A catheter was then inserted via the papilla. In the case of failing to enter the bile duct but repeated (more three times) insertion of the catheter into the pancreatic duct, a pancreatic guidewire or plastic stent was placed, and bile duct cannulation was attempted again. In cases of failed bile duct cannulation, the following procedures were carried out randomly: (1) TS: If the guidewire repeatedly entered the pancreatic duct but failed to enter the bile duct, the guidewire was left in the pancreatic duct. A bow knife was then inserted into the pancreatic duct to make a small incision (< 5 mm) into the papilla toward the bile duct. The transpancreatic septum was cut, and the bile duct cannulation was then performed again (Figure 2). All patients underwent pancreatic stenting after TS; and (2) conventional NKS: A needle knife was inserted upward into the papilla opening or into the papilla uplift about 5-10 mm above the papilla opening. Electrical excision and electrocoagulation were then applied from the top down to cut the mucous membrane and papilla ampulla sphincter layer by layer in the 11-12 o’clock direction. All patients underwent pancreatic stenting after NKS.
ERCP complications included: (1) acute pancreatitis (AP): at 24 h after ERCP, the serum amylase value exceeded 3 times the upper limit of normal and was accompanied by persistent abdominal pain; (2) infection: The patient had right upper quadrant pain accompanied by fever > 38.5 °C, as well as a white blood cell count > 10 × 109/L without infectious lesions within 24 h after ERCP; (3) gastrointestinal bleeding: The patient had vomiting or black stools after ERCP or hemoglobin < 95% of normal level within 24 h[9]; and (4) perforation: Subcutaneous emphysema, retroperitoneal air, or subphrenic free air was detected after ERCP.
The cannulation success rate and complications were compared by χ2 tests using SPSS 15.0. A P-value < 0.05 was considered statistically significant.
A total of 1059 patients underwent ERCP, and 896 patients achieved successful bile duct cannulation. Of the other 163 patients who experienced difficult bile duct cannulation during ERCP, 94 completed ERCP successfully with the assistance of a pancreatic guidewire or plastic stent. The total success rate was 93.4% (990/1059). Of the remaining 69 patients, 67 underwent successful bile duct cannulation after precut papillotomy, with a success rate of 97.1%. Therefore, the total success rate of bile duct cannulation was 99.8% (1057/1059). The total success rate was 97.2% (35/36) in the TS group, and one unsuccessful case was managed by percutaneous transhepatic cholangial drainage. The total success rate was 96.9% (32/33) in the NKS group, and one unsuccessful case was treated by surgical intervention. The total success rates were not statistically different between the two groups (P > 0.05).
Complications occurred in 11 out of the 69 precut cases, including AP (n = 6), bleeding (n = 2), and cholangitis (n = 3). Two cases of AP and one case of cholangitis occurred in the TS group, and four cases of AP, two cases of bleeding and two cases of cholangitis occurred in the NKS group. The total complication rate was significantly lower in the TS group than in the NKS group (8.3% vs 24.2%, P < 0.05). The patients with AP were fasted and given anti-inflammatory treatment and inhibition of pancreatic secretion, and recovery was achieved one week later. Intravenous hemostatic agents were administrated for patients with bleeding, which was stopped 2 d later. Patients with cholangitis recovered one week after anti-inflammatory treatment.
The 69 patients in the TS and NKS groups were followed for four months. No recurrence of bile duct stones was seen, and SOD was relieved in both groups. One patient with cholangitis in the NKS group relapsed. One patient with cholangiocarcinoma in the TS group died of liver failure by tumor invasion. One patient with pancreatic cancer in the NKS group died of tumor cachexia.
Endoscopy plays an increasingly important role in treating biliary and pancreatic diseases. Successful deep bile duct cannulation in ERCP is key to follow-up treatment of biliary diseases. However, the failure rate of bile duct cannulation is as high as 5%-20%[3]. At present, the most common methods to manage difficult bile duct cannulation include placement of a pancreatic guidewire or plastic stent, NKS, and TS. In this study, the success rate of bile duct cannulation increased to 93.4% by placement of a pancreatic guidewire or plastic stent, which is supposed to relieve the blockage of the pancreatic duct opening and facilitate the insertion of the second guidewire into the bile duct[10]. However, we believe that the guidewire or stent also changes the axis direction of the bile duct and straightens it.
Precut papillotomy is a complementary technique for conventional ERCP and endoscopic sphincterotomy (EST) that improves the success rate of ERCP and increases the success rate of papillotomy to 97%[11]. Needle-knife precut papillotomy is another commonly applied precut technique that has a high success rate of cannulation, as well as a high rate of complications (6%-20%), including perforation, bleeding, pancreatitis, and cholangitis[7]. Endoscopy researchers have been trying other precut techniques and hope to find a technique with a high success rate of cannulation and a low complication rate. Pancreatic duct cannulation has a relatively high success rate in clinical practice, but deep bile duct cannulation is relatively difficult, especially in patients with small papilla, peripapillary diverticulum, malposition of the papilla, or a history of Billroth II gastrectomy. We hypothesized that difficult bile duct cannulation may be related to duct blockage by the ampulla septum in cases where the guidewire repeatedly enters the pancreatic duct. The septum is located between the pancreatic duct and the common bile duct[8]. Therefore, we investigated TS in this study. Both NKS and TS resulted in high success rates, which were 96.9% and 97.2%, respectively, which were not significantly different between the two groups. However, the incidence of complications was significantly lower for TS than for NKS (8.3% vs 24.2%, P < 0.05).
TS was first reported by Goff[12]. In clinical practice, it is easy to insert the guidewire into the pancreatic duct but difficult to insert it into the bile duct. If the guidewire repeatedly enters the pancreatic duct but is unable to access the bile duct, a bow knife is used to make a 5-mm incision along the guidewire from the pancreatic duct at the 11-12 o’clock direction. After removing the bow knife, and the catheter is re-inserted into the bile duct along the upper left of the guidewire. This method has the advantages of a small incision; manageable direction; and a low incidence of bleeding, perforation, and infection. Goff reported an overall success rate up to 97.5% in his long-term study of 51 patients[13]. Weber et al[14] performed transpancreatic precut sphincterotomy for cannulating inaccessible common bile ducts in 108 patients. The success rate of selective bile duct cannulation was 95.4%, and the incidence of complications reached 11.1%. They suggested that the technique could be applied to the unsuccessful cases of conventional EST or needle-knife precutting. Catalano et al[8] compared TS with standard precut papillotomy in a randomized study and found that the former resulted in a higher success rate of bile duct cannulation and a lower incidence of complications; pancreatitis occurred in 3.4% and 11.8% of cases, respectively. Kahaleh et al[15] reported an overall success rate of 85% and a complication rate of 12% for 116 TS cases. In the present study, both TS and NKS had high success rates, which is similar to those reported in the literature. The results indicate that both techniques can improve bile duct surgery success rate, but TS is safer because of its lower complication rate. Of course, both techniques must be performed by skilled ERCP surgeons.
In summary, pancreatic guidewire or plastic stent assistance improves the success rate of selective bile duct cannulation in ERCP. TS and NKS further improve the success rate; however, TS is safer than NKS.
Pre-cut techniques, with the most commonly described being needle knife sphincterotomy (NKS), have been used to facilitate biliary access in failed standard biliary cannulation. Transpancreatic septotomy (TS) is a new pre-cut technique with limited outcome data.
Precut papillotomy is a complementary technique for endoscopic sphincterotomy that improves the success rate of endoscopic retrograde cholangiopancreatography (ERCP) and increases the success rate of papillotomy. Endoscopy researchers have been trying other precut techniques and hope to find a technique with a high success rate of cannulation and a low complication rate.
In the present study, TS has the advantages of a small incision; manageable direction; and a low incidence of bleeding, perforation, and infection.
In clinical practice, it is easy to insert the guidewire into the pancreatic duct but difficult to insert it into the bile duct. If the guidewire repeatedly enters the pancreatic duct but is unable to access the bile duct, TS is a good choice.
Transpancreatic septotomy is defined as a controlled incision into the common bile duct to achieve selective biliary cannulation. During ERCP, TS and NKS further improve the success rate; however, TS is safer than NKS.
In this manuscript the authors report their experience in the treatment of 163 patients with difficult bile duct cannulation who underwent a second attempt by either transpancreatic septotomy or needle knife sphincterotomy. Fortunately, they have two comparable groups of patients subjected to each of both procedures, the results are interesting and conclusions are correctly derived from these results.
P- Reviewer: Gonzalez-Reimers E, Richardson WS S- Editor: Qi Y L- Editor: Wang TQ E- Editor: Liu XM
| 1. | Qayed E, Reid AL, Willingham FF, Keilin S, Cai Q. Advances in endoscopic retrograde cholangiopancreatography cannulation. World J Gastrointest Endosc. 2010;2:130-137. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Cennamo V, Fuccio L, Zagari RM, Eusebi LH, Ceroni L, Laterza L, Fabbri C, Bazzoli F. Can early precut implementation reduce endoscopic retrograde cholangiopancreatography-related complication risk? Meta-analysis of randomized controlled trials. Endoscopy. 2010;42:381-388. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 134] [Cited by in F6Publishing: 142] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 3. | Larkin CJ, Huibregtse K. Precut sphincterotomy: indications, pitfalls, and complications. Curr Gastroenterol Rep. 2001;3:147-153. [PubMed] [Cited in This Article: ] |
| 4. | Chan CH, Brennan FN, Zimmerman MJ, Ormonde DG, Raftopoulos SC, Yusoff IF. Wire assisted transpancreatic septotomy, needle knife precut or both for difficult biliary access. J Gastroenterol Hepatol. 2012;27:1293-1297. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Saritas U, Ustundag Y, Harmandar F. Precut sphincterotomy: a reliable salvage for difficult biliary cannulation. World J Gastroenterol. 2013;19:1-7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 15] [Cited by in F6Publishing: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Freeman ML, Overby C, Qi D. Pancreatic stent insertion: consequences of failure and results of a modified technique to maximize success. Gastrointest Endosc. 2004;59:8-14. [PubMed] [Cited in This Article: ] |
| 7. | Freeman ML, Guda NM. Endoscopic Biliary and Pancreatic Sphincterotomy. Curr Treat Options Gastroenterol. 2005;8:127-134. [PubMed] [Cited in This Article: ] |
| 8. | Catalano MF, Linder JD, Geenen JE. Endoscopic transpancreatic papillary septotomy for inaccessible obstructed bile ducts: Comparison with standard pre-cut papillotomy. Gastrointest Endosc. 2004;60:557-561. [PubMed] [Cited in This Article: ] |
| 9. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. [PubMed] [Cited in This Article: ] |
| 10. | Kramer RE, Azuaje RE, Martinez JM, Dunkin BJ. The double-wire technique as an aid to selective cannulation of the common bile duct during pediatric endoscopic retrograde cholangiopancreatography. J Pediatr Gastroenterol Nutr. 2007;45:438-442. [PubMed] [Cited in This Article: ] |
| 11. | Foutch PG. A prospective assessment of results for needle-knife papillotomy and standard endoscopic sphincterotomy. Gastrointest Endosc. 1995;41:25-32. [PubMed] [Cited in This Article: ] |
| 12. | Goff JS. Common bile duct pre-cut sphincterotomy: transpancreatic sphincter approach. Gastrointest Endosc. 1995;41:502-505. [PubMed] [Cited in This Article: ] |
| 13. | Goff JS. Long-term experience with the transpancreatic sphincter pre-cut approach to biliary sphincterotomy. Gastrointest Endosc. 1999;50:642-645. [PubMed] [Cited in This Article: ] |
| 14. | Weber A, Roesch T, Pointner S, Born P, Neu B, Meining A, Schmid RM, Prinz C. Transpancreatic precut sphincterotomy for cannulation of inaccessible common bile duct: a safe and successful technique. Pancreas. 2008;36:187-191. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Kahaleh M, Tokar J, Mullick T, Bickston SJ, Yeaton P. Prospective evaluation of pancreatic sphincterotomy as a precut technique for biliary cannulation. Clin Gastroenterol Hepatol. 2004;2:971-977. [PubMed] [Cited in This Article: ] |