Published online Apr 28, 2015. doi: 10.3748/wjg.v21.i16.5110
Peer-review started: September 30, 2014
First decision: October 29, 2014
Revised: November 13, 2014
Accepted: February 5, 2015
Article in press: February 5, 2015
Published online: April 28, 2015
Post-gastrectomy anastomosis site obstruction is a relatively rare complication after a subtotal gastrectomy. We present a case of a 75-year-old man who underwent a truncal vagotomy, omental patch, gastrojejunostomy, and Braun anastomosis for duodenal ulcer perforation and a gastric outlet obstruction. Following the 10th postoperative day, the patient complained of abdominal discomfort and vomiting. We diagnosed post-gastrectomy anastomosis site obstruction by an upper gastrointestinal series and an upper endoscopic examination. We inserted a self-expandable metallic stent (SEMS) at the anastomosis site. The stent was fully expanded after deployment. On the day following the stent insertion, the patient began to eat, and his abdominal discomfort was resolved. This paper describes the successful management of post-gastrectomy anastomosis site obstruction with temporary placement of a SEMS.
Core tip: Post-gastrectomy anastomosis site obstruction is a relatively rare complication in patients following gastric surgery; however, it could cause serious discomfort and carries a risk of deterioration of the condition of the patient if a re-operation is required. We report successful management for post-gastrectomy anastomosis site obstruction with temporary placement of a self-expandable metallic stent.
- Citation: Cha RR, Lee SS, Kim H, Kim HJ, Kim TH, Jung WT, Lee OJ, Bae KS, Jeong SH, Ha CY. Management of post-gastrectomy anastomosis site obstruction with a self-expandable metallic stent. World J Gastroenterol 2015; 21(16): 5110-5114
- URL: https://www.wjgnet.com/1007-9327/full/v21/i16/5110.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i16.5110
Post-gastrectomy anastomosis site obstruction is a relatively rare complication following gastric surgery; it can cause serious discomfort and carries a risk of deterioration of the condition of the patient resulting from a re-operation. We present a case of post-gastrectomy anastomosis site obstruction after a truncal vagotomy, omental patch, gastrojejunostomy, and Braun anastomosis, and successful management with temporary placement of a self-expandable metallic stent (SEMS).
A 75-year-old man was referred to our hospital with hematemesis with epigastric pain the previous day. He had been admitted to our hospital several times for a gastric ulcer, duodenal ulcer, and gastric outlet obstruction. He had a history of smoking and daily alcohol use. On this admission, the physical examination revealed whole abdominal tenderness and rebound tenderness with rigidity. The patient presented with a fever (38.3 °C), tachycardia (100 beats/min), and an elevated white blood cell count (12100/μL). The serum glucose was 222 mg/dL (normal range: 70-110 mg/dL), and the levels of total protein, albumin, and C-reactive protein were 5.5 g/dL (normal range: 6.4-8.3 g/dL), 3.0 g/dL (normal range: 3.4-4.8 g/dL), and 242 mg/L (normal range: 0-5 mg/L), respectively; there were no remarkable abnormalities in the other biochemical tests including the renal and hepatic function tests. The abdominal CT scans demonstrated fluid collection and pneumoperitoneum around the pylorus.
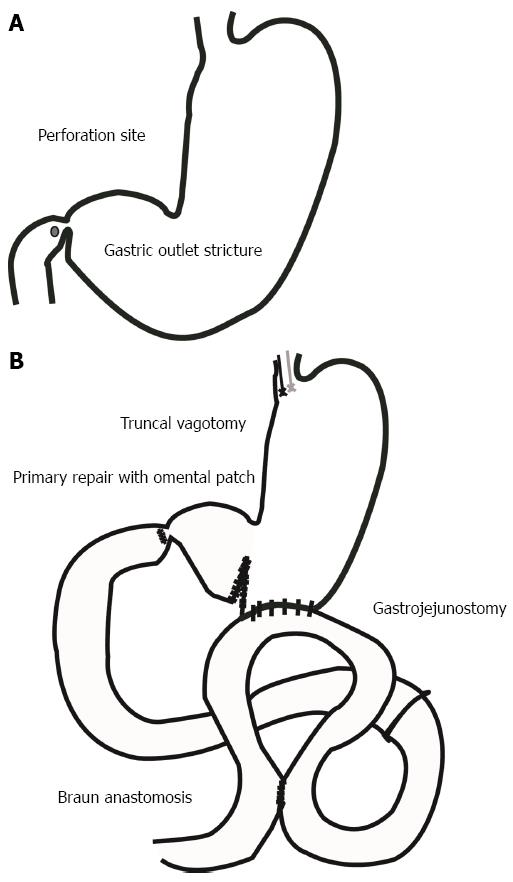
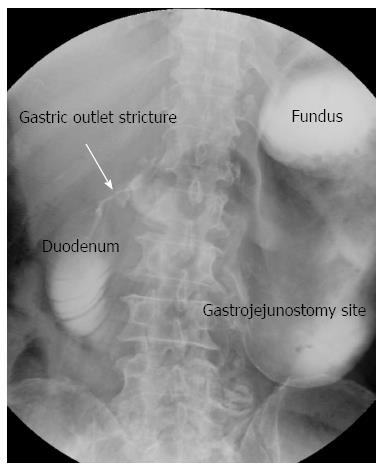
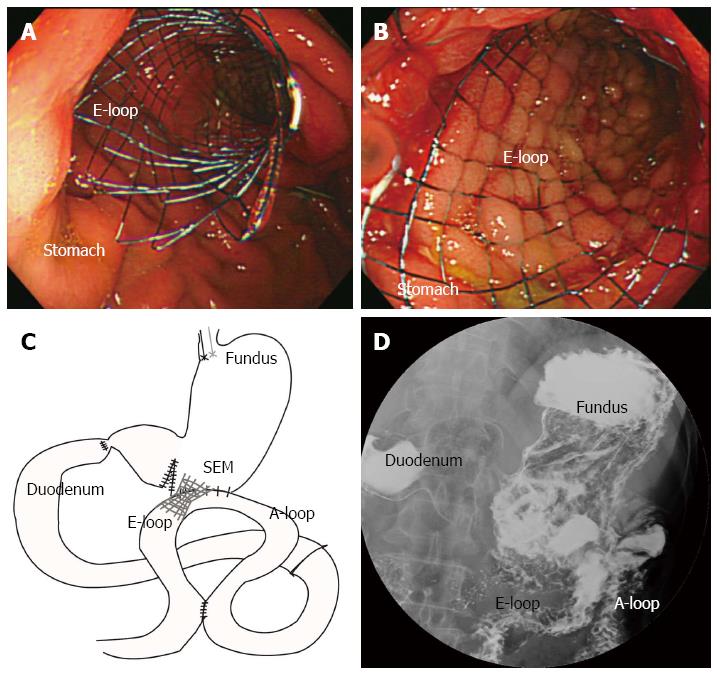
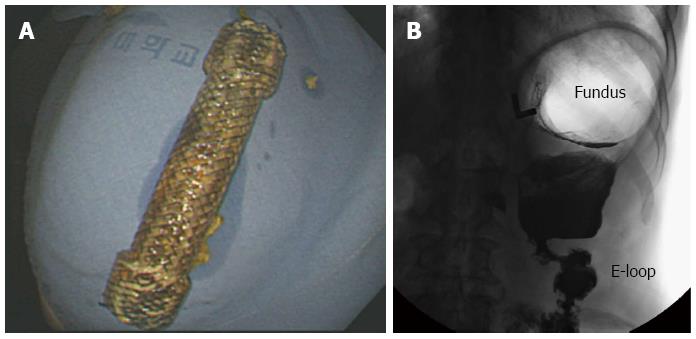
The patient underwent an emergency operation (truncal vagotomy, omental patch, gastrojejunostomy, and small-size Braun anastomosis) for the duodenal ulcer perforation and gastric outlet obstruction (Figure 1). After the 5th postoperative day, he began to eat. However, after the 10th postoperative day, he complained of abdominal discomfort and vomiting without bilious. An upper gastrointestinal series (UGIS) showed decreased peristalsis and severe distension of the stomach with no visible contrast passage to the gastrojejunostomy, and an endoscopy was performed (Figure 2). The endoscopy revealed extensive food material and anastomosis site obstruction. We diagnosed anastomosis site stricture of the gastrojejunostomy from postoperative stricture or torsion of the efferent loop of the gastrojejunostomy. We inserted a SEMS (a duodenal/pyloric non-covered stent; Sewoon Medical Co., Ltd., Chungcheongnam-Do, South Korea) at the anastomosis site (Figure 3A and B). Because the patient was older and did not have good general health, a reoperation was not advisable. The stent was introduced and inserted over a guide wire. The length of the stent body was 60 mm, with a diameter of 20 mm. The stent was fully expanded after deployment (Figure 3C). The UGIS showed good passage of the contrast material from the esophagus to the jejunum and no evidence of leakage at the anastomosis site (Figure 3D). On the day following the stent insertion, the patient began to eat, and his abdominal discomfort was resolved. The patient subsequently recovered, and there were no abdominal pain episodes. At the one-year follow-up, the stent had migrated into the stomach and was removed using alligator forceps with endoscopy. The UGIS revealed that the contrast dye passed the anastomosis site well. The patient survived, without other complications (Figure 4).
Post-gastrectomy anastomosis site obstruction is a rare complication (approximately 0.3%-1.0%)[1], and a re-operation is typically performed to resolve a gastric outlet obstruction; however, re-operations cause deterioration of the patient’s condition, and can be limited in elderly patients.
Two mechanical problems in post-gastric surgery complications are leakage and obstruction. First, anastomotic leakage is a life-threatening complication that requires prompt recognition and treatment[2]. Recent reports of successful endoscopic closure of anastomotic leakage suggest that endoscopic techniques might be a feasible alternative to surgical approaches[3]. Second, two loop syndromes of obstruction might occur after certain types of gastrectomies. Afferent or efferent loop syndrome is a purely mechanical problem caused by the obstruction of gastric emptying at or near the site of a gastrectomy[4]. Less invasive non-surgical procedures, such as insertion of gastrointestinal stents under endoscopy, percutaneous transhepatic biliary drainage, and percutaneous enterostomies have been used as a palliative option for post-gastrectomy obstruction[5,6].
Efferent loop syndrome is a rare post-gastrectomy complication. The major cause of the syndrome is an intestinal hernia, and minor causes include an adhesive band and kinking[7,8]. The clinical symptoms of efferent loop syndrome are characterized by abdominal cramps and bilious vomiting[7]. The treatment of efferent loop syndrome varies depending on the cause of the syndrome. Complete loop obstruction with a mechanical cause requires surgical intervention. Because of recent advances in endoscopic intervention, various treatment methods have been attempted. However, treatment has predominantly been reported in afferent loop syndrome, and very little documentation of the treatment of efferent loop syndrome exists. In several cases, endoscopic stent insertion was reported for the treatment of an obstruction caused by tumor recurrence or peritoneal seeding[8]. In this case, we used SEMS insertion to treat a patient with anastomosis site stricture in efferent loop syndrome caused by a benign stricture.
Recently, SEMS insertion has been used for palliative treatment of malignant gastric and duodenal obstructions because it requires a shorter procedure time and provides more prompt restoration of oral intake than surgical treatment. Some cases of SEMS insertion have been reported for the treatment of postoperative gastric outlet obstruction[9]. Most of these cases were for recurrent malignant gastric outlet obstruction; however, there are a few cases for benign gastric outlet obstruction. In our case, the patient underwent surgery for benign diseases including a gastric ulcer, duodenal ulcer, and gastric outlet obstruction. Temporary placement of a SEMS might be effective for symptomatic improvement in benign pyloric stenosis as well as for malignant stricture, although an inserted stent could migrate. A successful insertion of a SEMS in patients with post-gastrectomy anastomosis site obstruction is reported herein for the first time. For patients with post-gastrectomy anastomosis site obstruction who are poor candidates for surgery, the placement of SEMS might be an effective treatment method. The risk of anastomosis leakage could increase at the anastomosis site as a result of SEMS insertion. This procedure should be performed in selected cases in which the obstruction results from torsion instead of in cases of pure anastomosis site stricture.
In conclusion, placement of SEMS in selected patients with post-gastrectomy anastomosis site obstruction is a technically feasible and clinically effective procedure.
A 75-year-old man who underwent a truncal vagotomy, omental patch, gastrojejunostomy, and Braun anastomosis for duodenal ulcer perforation and a gastric outlet obstruction.
Anastomosis site torsion of the efferent loop of the gastrojejunostomy.
Anastomosis site stricture of the gastrojejunostomy from postoperative stricture.
An upper gastrointestinal series showed decreased peristalsis and severe distension of the stomach, with no visible contrast passage to the gastrojejunostomy, and an endoscopy revealed extensive food material and anastomosis site obstruction.
The authors inserted a self-expandable metallic stent (SEMS) at the anastomosis site.
Insertion of SEMSs has been used for palliative treatment of malignant gastric and duodenal obstructions.
Placement of SEMSs in selected patients with post-gastrectomy anastomosis site obstruction is a technically feasible and clinically effective procedure.
The authors report a rare case of a successful management for post-gastrectomy anastomosis site obstruction with temporary placement of a SEMS. The topic is interesting and this procedure could be an effective treatment for older patients who suffer anastomosis site obstruction after gastrointestinal anastomosis who are not suitable for reoperation.
P- Reviewer: Yu Z S- Editor: Ma YJ L- Editor: AmEditor E- Editor: Ma S
| 1. | Aoki M, Saka M, Morita S, Fukagawa T, Katai H. Afferent loop obstruction after distal gastrectomy with Roux-en-Y reconstruction. World J Surg. 2010;34:2389-2392. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Pedrazzani C, Marrelli D, Rampone B, De Stefano A, Corso G, Fotia G, Pinto E, Roviello F. Postoperative complications and functional results after subtotal gastrectomy with Billroth II reconstruction for primary gastric cancer. Dig Dis Sci. 2007;52:1757-1763. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 45] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Raju GS. Endoscopic closure of gastrointestinal leaks. Am J Gastroenterol. 2009;104:1315-1320. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Shchepotin IB, Evans SR, Chorny VA, Shabahang M, Buras RR, Nauta RJ. Postoperative complications requiring relaparotomies after 700 gastretomies performed for gastric cancer. Am J Surg. 1996;171:270-273. [PubMed] [Cited in This Article: ] |
| 5. | Han K, Song HY, Kim JH, Park JH, Nam DH, Ryu MH, Yook JH. Afferent loop syndrome: treatment by means of the placement of dual stents. AJR Am J Roentgenol. 2012;199:W761-W766. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Jung GS, Song HY, Kang SG, Huh JD, Park SJ, Koo JY, Cho YD. Malignant gastroduodenal obstructions: treatment by means of a covered expandable metallic stent-initial experience. Radiology. 2000;216:758-763. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 134] [Cited by in F6Publishing: 132] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 7. | Lee WY, Moon JS. Endoscopic treatment of efferent loop syndrome with insertion of double pigtail stent. World J Gastroenterol. 2013;19:7209-7212. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 10] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Baron TH, Harewood GC, Morgan DE, Yates MR. Outcome differences after endoscopic drainage of pancreatic necrosis, acute pancreatic pseudocysts, and chronic pancreatic pseudocysts. Gastrointest Endosc. 2002;56:7-17. [PubMed] [Cited in This Article: ] |
| 9. | Seth R, Rajasekaran K, Lee WT, Lorenz RR, Wood BG, Kominsky A, Scharpf J. Patient reported outcomes in endoscopic and open transcervical treatment for Zenker’s diverticulum. Laryngoscope. 2014;124:119-125. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |