Published online May 7, 2015. doi: 10.3748/wjg.v21.i17.5231
Peer-review started: December 19, 2014
First decision: February 10, 2015
Revised: February 26, 2015
Accepted: March 31, 2015
Article in press: March 31, 2015
Published online: May 7, 2015
Inflammatory bowel disease (IBD) is one of the most common chronic gastrointestinal diseases in pediatric patients. Choosing the optimal imaging modality for the assessment of gastrointestinal disease in pediatric patients can be challenging. The invasiveness and patient acceptance, the radiation exposure and the quality performance of the diagnostic test need to be considered. By reviewing the literature regarding imaging in inflammatory bowel disease the value of ultrasound in the clinical management of pediatric patients is highlighted. Transabdominal ultrasound is a useful, noninvasive method for the initial diagnosis of IBD in children; it also provides guidance for therapeutic decisions and helps to characterize and predict the course of the disease in individual patients. Ultrasound techniques including color Doppler imaging and contrast-enhanced ultrasound are promising imaging tools to determine disease activity and complications. Comparative studies between different imaging methods are needed.
Core tip: Inflammatory bowel disease is one of the most common chronic gastrointestinal diseases in pediatric patients. Choosing the optimal imaging modality for the assessment of gastrointestinal disease in pediatric patients can be challenging. The presented paper is intended to discuss the value of ultrasound, including conventional ultrasound, color Doppler imaging and contrast enhanced ultrasound, in the clinical management of pediatric patients with inflammatory bowel disease.
- Citation: Chiorean L, Schreiber-Dietrich D, Braden B, Cui XW, Buchhorn R, Chang JM, Dietrich CF. Ultrasonographic imaging of inflammatory bowel disease in pediatric patients. World J Gastroenterol 2015; 21(17): 5231-5241
- URL: https://www.wjgnet.com/1007-9327/full/v21/i17/5231.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i17.5231
Inflammatory bowel disease (IBD) is one of the most common gastrointestinal diseases affecting pediatric patients in the developed world[1]. Although true incidence rates are uncertain, Crohn’s disease (CD) is diagnosed annually in children at a rate of 0.2-8.5 per 100000 whereas ulcerative colitis (UC) is diagnosed at a rate of 0.5-4.3 per 100000[2,3]. Colonic involvement is frequently found in CD pediatric patients (84%), particularly the left-sided colon where maximal disease activity is usually found[4]. Isolated colonic disease is more frequent in early-onset CD (0-5 years of age) as compared to an older age group (6-17 years of age)[5]. Adolescents with UC tend to have severe and extensive disease at presentation, about 90% of adolescents presenting with pancolitis [6].
Diagnosis of IBD in pediatric patients can be challenging due to presentation with atypical symptoms and/or extraintestinal manifestations (e.g., short stature, chronic anemia, unexplained fever, arthritis, mouth ulcers)[7]. There is currently no single diagnostic test for CD, and the diagnosis is based on a combination of history, physical examination, endoscopic appearance, histologic findings in gastrointestinal biopsies, presence of serum inflammatory markers, and typical imaging results[8]. The course of the disease is unpredictable, exacerbations and phases of remissions can alternate, and no single parameter alone can at present reliably define the disease activity or prognosis[9,10].
In the last two decades, tremendous technological advances in IBD imaging resulted in significant effects on the diagnostic and therapeutic work-up of patients[11,12]. These new imaging modalities can reveal mucosal alterations as well as transmural and periintestinal inflammation and enable a more detailed disease staging; they also can be helpful in detecting asymptomatic disease and assessing response to therapy[13]. Due to the noninvasive nature of some of the new techniques, there has been a remarkably increased imaging demand for pediatric IBD patients, mainly when repeated investigations are required for follow-up[14].
Imaging of pediatric patients with IBD must balance diagnostic accuracy of the test against concerns about patient exposure to ionizing radiation. Patient acceptance and non-invasiveness of the imaging technique need also be accounted for. Because of their small body size and higher rate of cellular proliferation, pediatric patients have a higher cancer risk per unit radiation dose than adults[15]. The cumulative radiation dose should also be considered because pediatric patients may undergo numerous imaging tests over a lifetime due to the relapsing nature of the disease[16-19]. Current risk estimates indicate that the radiation exposure from these imaging studies may be sufficient to increase the lifetime risk of cancer[20].
In the ESPGHAN Revised Porto Criteria for the Diagnosis of Inflammatory Bowel Disease in Children and Adolescents[21], ultrasound has been described as a noninvasive, and widespread available method, valuable as a screening tool in the preliminary diagnostic work-up of pediatric patients with suspected IBD due to its major advantages of low costs and lack of radiation exposure[22-24].
According to the European Crohn’s and Colitis Organisation (ECCO) guidelines[25], computed-tomography and magnetic resonance imaging are considered the current standard for assessing the small intestine providing similar diagnostic accuracy for the detection of small intestine inflammatory lesions[26,27]. Considering radiation exposure resulting from computed tomography examinations, magnetic resonance should be preferred when possible[25,28]. Transabdominal ultrasound is described as a useful additional technique for assessing bowel inflammation, representing another non-ionizing imaging technique which may provide information about disease activity, in particular for CD limited to the ileum[29]. The use of contrast-enhanced abdominal ultrasound and color Doppler imaging increases its sensitivity and specificity in the detection of disease activity[30-32]. Significant drawbacks of the sonographic technique are the difficult visualisation of deep bowel segments and the high interobserver variability[25].
Transabdominal ultrasound is presently accepted as a clinically important first line tool in assessing patients with CD irrespective of their clinical symptoms and/or disease activity and it provides guidance for therapeutic decisions[33-35]. Due to its high negative predictive value, abdominal ultrasound is useful in the preliminary diagnostic work-up of patients with suspected small bowel inflammation before more invasive tests are performed[25]. However, its most important application is the follow-up of patients with a previous diagnosis of CD to assess the extent of disease involvement and identify early intra-abdominal complications[36].
Duigenan et al[17] published in 2012 a review on the current imaging literature and developed basic imaging guidelines for the diagnostic evaluation of children with IBD. They outlined the role of ultrasound as a noninvasive test that avoids ionizing radiation, is ideally suited for pediatric IBD assessment, with the need of prospective evaluation of high-frequency bowel ultrasound as a potentially helpful tool in routine surveillance.
Oral contrast (“small intestinal contrast ultrasonography”) has been tested in pediatric patients. The use of oral anechoic contrast solution (iso-osmolar polyethylene glycol) enhances the sensitivity and decreases the inter-observer variability[21,37,38].
Pallotta et al[38] published in 2013 a study in 51 consecutive pediatric patients, 21 with suspected and 30 with proven CD. Transabdominal ultrasound and small intestine contrast ultrasonography were compared with small bowel follow-through and endoscopy for the detection of small bowel lesions using the final diagnosis as reference standard. They reported a sensitivity and specificity of 75% and 100% respectively for Transabdominal ultrasound, and of 100% and 100% respectively for small intestine contrast ultrasonography in undiagnosed patients, and of 76% and 100% respectively for transabdominal ultrasound, and of 96% and 100% respectively for small intestine contrast ultrasonography in patients with proved CD. The agreement (k) with radiology for the site of the lesions was almost perfect for small intestine contrast ultrasonography (0.93), both for jejunal and ileal lesions, and it was fair (0.40) for jejunal and substantial (0.68) for ileal lesions for transabdominal ultrasound. They concluded that small intestine contrast ultrasonography, as a noninvasive, radiation free, and well-tolerated tool should be used as a first line investigation in the management of children with suspected or already-diagnosed CD[39]. Previously, in a study published in 2005, Pallotta et al[38] studied 148 adolescents and adults, 57 of them with previously diagnosed CD, and showed that small intestine contrast ultrasonography had a higher sensitivity and specificity (100% and 98%, respectively) than conventional ultrasound (57% and 94.3%, respectively), in detecting the number and sites of small bowel lesions.
Recently, technological advances[40-45] have improved the performance of ultrasound with regard to different disease aspects and potential therapeutic decisions and produced enthusiasm for its use in IBD children[37,38]. Intravenous contrast agents have not yet been authorized for pediatric ages but off label use is mandatory if no other equivalent and approved method is available[46,47]. Elastography is also an additional and promising tool[48,49].
A review published in 2012 by Di Nardo et al[50] describes the most recent advances, the application of novel imaging and endoscopic methodologies for investigation of the small bowel in children with suspected or established CD. They described ultrasound as a very useful modality for IBD imaging in children due to its non-invasiveness, low cost, lack of radiation and widespread availability[22,51].
On the other hand, important limitations are that the alimentary tract cannot be visualized over its entire length, many of the findings are nonspecific and obtaining and interpreting the images is operator dependent[52].
According to the ESPGHAN Revised Porto Criteria for the Diagnosis of Inflammatory Bowel Disease in Children and Adolescents, small bowel imaging is recommended in all suspected cases of IBD at diagnosis (except for the cases of typical UC, where the diagnosis can be based on endoscopy and histology). Imaging is particularly important in suspected CD, in patients whose ileum could not be intubated, in patients with apparent UC with atypical presentations, and in patients with unclassified IBD[21].
Based on the ECCO consensus on the diagnosis and management of CD in special situations[53], initial investigation in children and adolescents with suspected IBD should consist of ileocolonoscopy with multiple biopsies and small bowel imaging, irrespective of the findings at ileocolonoscopy, in order to guide therapeutic management and detect strictures that may need surgical resection even though the terminal ileum may appear normal at colonoscopy[25,53-55].
The sonographic sensitivity and specificity for the diagnosis of CD range from 75% to 94% and 67% to 100%, respectively[29]. In a prospective study by Borthne et al[56], the sensitivity and diagnostic accuracy of 15 ultrasound examinations tested against endoscopy as the gold standard was 93.3%. All the ultrasound examinations were concordant with the endoscopy findings except in one patient with CD but negative ultrasound result. Comparative studies between ultrasound and ileocolonoscopy with histology in detecting CD lesions at the terminal ileum have shown an overall sensitivity and specificity of 74%-88% and 78%-93%, respectively[57,58]. Ultrasound is more sensitive in detecting terminal ileum lesions (about 90%-95%), while its sensitivity is decreased for proximal small bowel lesions (75%) and colonic lesions (82%)[59]. In a prospective study on 43 pediatric patients with clinical suspicion of IBD, the sensitivity of ultrasound compared to endoscopy was 93.3% and the diagnostic accuracy 93.3%[56]. Overall result of the meta-analysis by Horsthuis et al[27], regarding the accuracies of ultrasound, magnetic resonance imaging, scintigraphy, and computed tomography in the diagnosis of IBD was that no significant differences in diagnostic accuracy among the imaging techniques were observed (mean sensitivity estimates on a per-patient basis were 89.7%, 93.0%, 87.8%, and 84.3% for ultrasound, magnetic resonance imaging, scintigraphy, and computed tomography, respectively; mean per-patient specificity estimates were 95.6%, 92.8%, 84.5%, and 95.1% for ultrasound, magnetic resonance imaging, scintigraphy, and computed tomography, respectively).
Mesenteric lymphadenopathy might be a very early finding of CD which can be found even before mural changes are visible. This might reflect the autoimmune nature of the disease but published data are lacking.
According to the ESPGHAN Revised Porto Criteria for the Diagnosis of Inflammatory Bowel Disease in Children and Adolescents, ultrasound is recommended as a valuable screening tool in the preliminary diagnostic work-up of pediatric patients with suspected IBD, but should be complemented by more sensitive imaging of the small bowel[21].
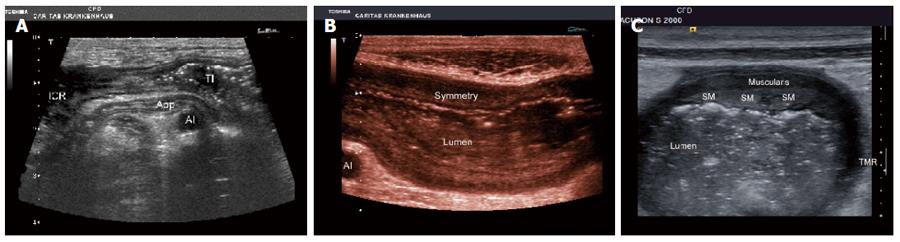
Transabdominal ultrasound is clinically useful in CD by evaluating the extent and localization of involved bowel segments (Figure 1A). The early signs are segmental bowel wall thickening (Figure 1B) and asymmetric thickening (Figure 1C), assumed to correspond to endoscopic signs of focal ulcerations and/or polypoid mucosal changes. The asymmetric segmental bowel wall thickening, areas of normal appearing mucosa alternating with inflamed mucosa, is creating the so called “cobblestone appearance” in CD, different from the continuous involvement in UC[33,60]. In early CD the wall stratification is usually preserved, and the submucosa is thickened and appears as a hyperechoic band. In severe disease the stratification may disappear, due to deep mural ulcers with substantial inflammation and neovascularization[22,50].
Dinkel and colleagues evaluated 32 children diagnosed with CD by real-time sonography and described typical ultrasound patterns which might help to establish the correct diagnosis in patients presenting with unspecific abdominal complaints. However, the differential diagnosis of similar sonographic features and the limitations of ultrasound in evaluating gastrointestinal disease must still be considered[61].
Different values for the wall thickness have been suggested as threshold for a positive diagnosis in various reports (from 1.5 mm to 3 mm for the terminal ileum and < 2 mm for the colon)[62].
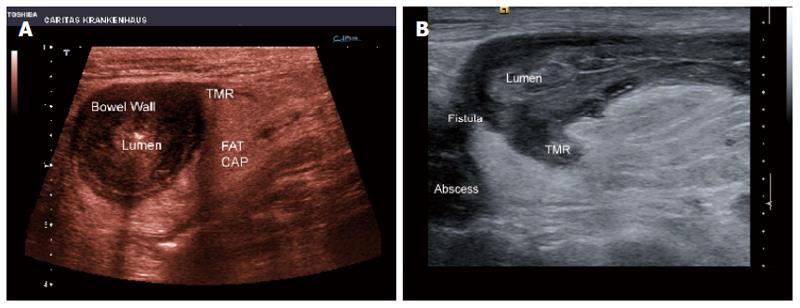
In proven CD the sonographic findings during follow-up reflect the clinical course and may delineate complications[61]. Transmural inflammation (Figure 2A) and transmural inflammation with fistula formation (Figure 2B) are observed in more advanced and complicated stages. In long-standing disease the bowel wall is thickened due to fibrosis and it sonographically appears hypoechoic, with loss of normal stratification. Due to the fibrofatty proliferation of the mesentery, the affected segment tends to be isolated, fixed, without peristalsis, and shows abnormal angulation[22].
Pediatric patients with IBD as well as adults with childhood-onset IBD are at increased risk to develop other comorbidities and complications[63]. Therefore, the presence of periintestinal inflammatory reaction and the surrounding structures should also be assessed to detect luminal (ileus) and extraluminal complications such as ileus, carcinoma, fistula, perforation and abscesses[33,64]. Strictures are typically visualised as marked thickening with a fixed hyperechoic narrowed lumen associated with dilatation and hyperperistalsis of the prestenotic gut[65]. In UC, the so called lead pipe appearance is due to mucosal ulcerations and consecutive fibrosis[66].
According to joint ECCO and ESGAR evidence-based consensus guidelines published by Panes et al[67] in 2013, ultrasound, computed tomography, and magnetic resonance imaging have a high accuracy for the assessment of penetrating complications (i.e., fistula, abscess) and for monitoring disease progression. Ultrasound allows the detection of complications such as fistulas (and the early stage of fistula, transmural inflammation), abscesses and ileus/subileus with high sensitivity and specificity[68-73]. Power Doppler ultrasound has been suggested to improve the diagnostic accuracy of transabdominal ultrasound in discriminating inflammatory from fibrotic strictures[27,29,58,74,75]. Maconi et al[70] have been able to detect internal fistulae in CD, by detecting an increased vascularity within the wall of these lesions and associated abscesses by detecting the absence of signals within the centre of these lesions (Figure 3).
As a cross-sectional imaging method, computed tomography may be particularily helpful in the acute situation, for planing surgery, or in the evaluation of strictures or obstruction[76,77]. Ultrasound and computed tomography are widely available and facilitate early abscess drainage[67]. However, the major disadvantage of computed tomography scans is the large amount of radiation exposure[78]. Furthermore, computed tomography enteroclysis is poorly tolerated in children[79].
Transabdominal ultrasound examination of extraluminal phenomena such as free fluid collection and/or mesenteric lymph nodes may reflect disease activity, but clinical data corroborating such a view are scanty. Although lymph node enlargement is a common sonographic finding in CD[34,35,80-82], it appears that ultrasound assessment of lymph nodes with regard to clinical parameters, particularly disease activity, is only of limited value and the clinical implications remain to be further clarified. Very early manifestation of CD in children might be mesenterial lymphadenopathy with or without bowel wall thickening[33].
In addition, several extraintestinal manifestations, particularly perihepatic lymphadenopathy can be reliably diagnosed by transabdominal ultrasound, along with pericholangitis, steatosis, chronic hepatitis, cirrhosis, and gallstone formation which are also overrepresented[34,53,80].
Ileostomy, small bowel resection or longstanding extensive small bowel activity are risk factors in CD to develop urolithiasis which can be detected using ultrasound[83].
Assessment of disease activity is important for treatment decisions[32,35,68,84-90]. The first parameter in imaging modalities supposed to reflect disease activity is bowel wall thickening, although detailed data are disappointing[33,84,85,88-98]. The length and extent of the involved bowel segments is also related to disease activity[33,99]. Other parameters of disease activity with an overlap to complications include extraluminal phenomena such as free fluid collection (ascites)[100].
The role of ultrasound in assessing disease activity has been extensively investigated. Haber et al[62] have shown in 23 CD children that the maximal bowel wall thickness is correlated with the disease activity index, erythrocyte sedimentation rate, and C-reactive protein (CRP) levels.
In their study on pediatric patients with UC, Civitelli et al[101] showed that ultrasound can accurately detect the anatomic location of the disease, with a high level of agreement with endoscopy (k = 0.094). Also, their constructed ultrasound score to quantify disease severity strongly correlated with both endoscopic (r = 0.94) and clinical (r = 0.90) activity of disease. They concluded that colonic ultrasound may therefore be preferred in clinical pediatric practice for monitoring disease course and for assessing short-term treatment response, moreover since colonic ultrasound does not require a specific bowel preparation such as magnetic resonance enteroclysis does.
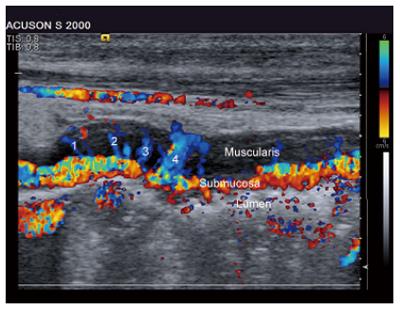
As stated in current guidelines, color Doppler imaging increases the sensitivity and specificity of transabdominal ultrasound, in particular for CD limited to the ileum[25]. It has been used to determine the disease activity by demonstrating hyperemia both of the bowel wall and adjacent mesentery. This turned out to be a notable marker of disease activity in IBD[29,31,32,98,102-113]. Combination of B-mode and power Doppler sonography has a high accuracy in the determination of disease activity in CD when compared to ileocolonoscopy[114]. A significantly higher bowel wall perfusion has been demonstrated in bowel segments of CD patients compared with healthy pediatric patients. The vessel density in affected bowel loops, as estimated with Doppler ultrasound, along with bowel wall thickening (> 5 mm) has been proved to reflect disease activity in patients with CD[98,111]. The hypervascularity in the gastrointestinal wall of patients with CD may be indicative of subclinical disease and this should be followed in prospective studies[115].
Ruess et al[116] found in 17 children and adolescents with IBD that bowel wall thickening (> 3 mm) and Doppler ultrasound grading of the bowel wall vascular pattern correlated with laboratory and clinical parameters of disease activity. Reduction or resolution of hypervascularity (as assessed by color Doppler ultrasound) can suggest efficacy of treatment.
In a study by Spalinger et al[98], ninety-two pediatric patients underwent 119 ultrasound examinations, from which 85 were performed in patients with active disease. Thicker affected bowel loops with higher vessel density were observed in disease state than during remission. They concluded that with the use of strictly controlled and constant technical factors, color Doppler imaging estimation of vessel density in a bowel loop affected by CD reflects disease activity. This noninvasive test may prove to be useful for monitoring the course of the disease. It has the potential to monitor the response to therapy, e.g., when experimental treatments of the disease, including angiogenesis inhibitors, are being tested in clinical trials.
In a study by Scholbach et al[111] color Doppler imaging videos of bowel wall perfusion from 34 healthy children and from 14 patients with CD were recorded under defined conditions and have been compared using the Pediatric Disease Activity Index. The method of dynamic, automatic noninvasive perfusion quantification has been proved to be useful to describe local inflammatory activity in bowel segments affected by CD and adds new information to activity evaluation by the Pediatric Crohn’s Disease Activity Index. Specific wall perfusion in intestines of CD patients is significantly elevated and reaches up to seven fold intensity compared with healthy subjects.
After the first guidelines on the use of contrast-enhanced ultrasound, introduced by The European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) in 2004, which mainly focused on liver applications[117], the update version published in 2008 described applications on other organs as well[118,119]. The new EFSUMB guidelines and recommendations from 2011[45] have added among others a section on the gastrointestinal tract. Herein, the role of contrast-enhanced ultrasound in the diagnosis of IBD has been described, including considerations on the disease activity, distinguishing between fibrous and inflammatory strictures, abscesses, and fistula. Limitations as well as recommended uses and indications have also been stated. “Comments and Illustrations of the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) Non-Liver Guidelines 2011” which focuses more on established applications are published in the same supplement to Ultraschall in der Medizin (European Journal of Ultrasound)[120].
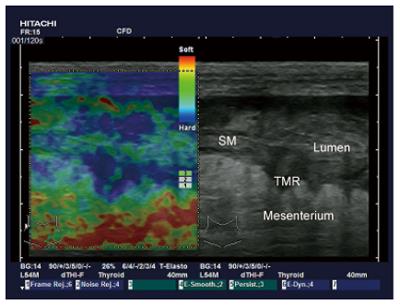
In a study with 104 patients with CD examined by contrast-enhanced ultrasound with respect to the disease activity index, it was found that the pattern of contrast enhancement and the ratio of enhanced to entire wall thickness had a positive predictive value of 63.0% and 58.6%, respectively, in distinguishing active from inactive disease[121] (Figure 4). Peri-intestinal inflammation also can be characterized in more detail[122]. Contrast-enhanced ultrasound has been proven to be helpful in the delineation of abscess[45,120,123-126]. Contrast-enhanced ultrasound can also provide prognostic data concerning relapse and/or response to therapy[127].
Elastography has recently been applied in patients with IBD[128-130]. Strain imaging techniques (“elastography”) allow noninvasive imaging of the mechanical characteristics of tissues. Inflammation and neoplastic infiltration lead to changes in normal tissue structure causing hardening of the tissue and alteration of its elasticity[131] (Figure 5).
The European Federation for Ultrasound in Medicine and Biology (EFSUMB) developed a set of recommendations for the use of elastography including clinical applications on the gastrointestinal tract, regarding the wall pathology as well as the motility[48,49].
Most studies using elastography in the gastrointestinal tract have used the endosonographic approach but the percutaneous access is also promising[132,133].
Transabdominal ultrasound is useful for the detection of IBD in pediatric patients (initial diagnosis) by evaluating the bowel wall thickening and surrounding structures. Periintestinal inflammatory reaction, the extent and localization of involved bowel segments and the presence of extraluminal complications such as fistula, abscesses, carcinoma and ileus can be assessed using transabdominal ultrasound. Ultrasound techniques including color Doppler imaging and contrast-enhanced ultrasound are promising novel tools to determine disease activity. Transabdominal ultrasound also helps to guide therapeutic decisions and allows better characterization of the disease course in individual patients.
P- Reviewer: BaronToaldo M, Farkas K S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
| 1. | Loftus EV. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology. 2004;126:1504-1517. [PubMed] [Cited in This Article: ] |
| 2. | Diefenbach KA, Breuer CK. Pediatric inflammatory bowel disease. World J Gastroenterol. 2006;12:3204-3212. [PubMed] [Cited in This Article: ] |
| 3. | Mamula P, Markowitz JE, Baldassano RN. Inflammatory bowel disease in early childhood and adolescence: special considerations. Gastroenterol Clin North Am. 2003;32:967-995, viii. [PubMed] [Cited in This Article: ] |
| 4. | Maccioni F, Viola F, Carrozzo F, Di Nardo G, Pino AR, Staltari I, Al Ansari N, Vestri A, Signore A, Marini M. Differences in the location and activity of intestinal Crohn’s disease lesions between adult and paediatric patients detected with MRI. Eur Radiol. 2012;22:2465-2477. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Paul T, Birnbaum A, Pal DK, Pittman N, Ceballos C, LeLeiko NS, Benkov K. Distinct phenotype of early childhood inflammatory bowel disease. J Clin Gastroenterol. 2006;40:583-586. [PubMed] [Cited in This Article: ] |
| 6. | Kugathasan S, Judd RH, Hoffmann RG, Heikenen J, Telega G, Khan F, Weisdorf-Schindele S, San Pablo W, Perrault J, Park R. Epidemiologic and clinical characteristics of children with newly diagnosed inflammatory bowel disease in Wisconsin: a statewide population-based study. J Pediatr. 2003;143:525-531. [PubMed] [Cited in This Article: ] |
| 7. | Cuffari C, Darbari A. Inflammatory bowel disease in the pediatric and adolescent patient. Gastroenterol Clin North Am. 2002;31:275-291. [PubMed] [Cited in This Article: ] |
| 8. | Baumgart DC, Sandborn WJ. Inflammatory bowel disease: clinical aspects and established and evolving therapies. Lancet. 2007;369:1641-1657. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1247] [Cited by in F6Publishing: 1242] [Article Influence: 73.1] [Reference Citation Analysis (0)] |
| 9. | Present DH. Serologic tests are not helpful in managing inflammatory bowel disease. Inflamm Bowel Dis. 2002;8:227-229; discussion 223, 227-29;. [PubMed] [Cited in This Article: ] |
| 10. | Maccioni F, Viscido A, Broglia L, Marrollo M, Masciangelo R, Caprilli R, Rossi P. Evaluation of Crohn disease activity with magnetic resonance imaging. Abdom Imaging. 2000;25:219-228. [PubMed] [Cited in This Article: ] |
| 11. | Fletcher JG, Fidler JL, Bruining DH, Huprich JE. New concepts in intestinal imaging for inflammatory bowel diseases. Gastroenterology. 2011;140:1795-1806. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 101] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 12. | Mackalski BA, Bernstein CN. New diagnostic imaging tools for inflammatory bowel disease. Gut. 2006;55:733-741. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 80] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 13. | Pariente B, Cosnes J, Danese S, Sandborn WJ, Lewin M, Fletcher JG, Chowers Y, D’Haens G, Feagan BG, Hibi T. Development of the Crohn’s disease digestive damage score, the Lémann score. Inflamm Bowel Dis. 2011;17:1415-1422. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 412] [Cited by in F6Publishing: 419] [Article Influence: 32.2] [Reference Citation Analysis (1)] |
| 14. | Shikhare G, Kugathasan S. Inflammatory bowel disease in children: current trends. J Gastroenterol. 2010;45:673-682. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Harley NH, Chittaporn P, Heikkinen MS, Meyers OA, Robbins ES. Radon carcinogenesis: risk data and cellular hits. Radiat Prot Dosimetry. 2008;130:107-109. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Brenner DJ, Elliston CD, Hall EJ, Berdon WE. Estimates of the cancer risks from pediatric CT radiation are not merely theoretical: comment on „point/counterpoint: in x-ray computed tomography, technique factors should be selected appropriate to patient size. against the proposition“. Med Phys. 2001;28:2387-2388. [PubMed] [Cited in This Article: ] |
| 17. | Duigenan S, Gee MS. Imaging of pediatric patients with inflammatory bowel disease. AJR Am J Roentgenol. 2012;199:907-915. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 18. | Rice HE, Frush DP, Farmer D, Waldhausen JH. Review of radiation risks from computed tomography: essentials for the pediatric surgeon. J Pediatr Surg. 2007;42:603-607. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 131] [Cited by in F6Publishing: 127] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 19. | Robbins E, Meyers PA. Ionizing radiation: an element of danger in every procedure. Pediatr Blood Cancer. 2010;55:397-398. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Robbins E. Radiation risks from imaging studies in children with cancer. Pediatr Blood Cancer. 2008;51:453-457. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 64] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Levine A, Koletzko S, Turner D, Escher JC, Cucchiara S, de Ridder L, Kolho KL, Veres G, Russell RK, Paerregaard A. ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr. 2014;58:795-806. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 822] [Cited by in F6Publishing: 811] [Article Influence: 81.1] [Reference Citation Analysis (0)] |
| 22. | Alison M, Kheniche A, Azoulay R, Roche S, Sebag G, Belarbi N. Ultrasonography of Crohn disease in children. Pediatr Radiol. 2007;37:1071-1082. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 23. | Dietrich CF. [Editorial on the contribution “Challenges for the German Health Care System”]. Z Gastroenterol. 2012;50:555-556. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Dietrich CF, Riemer-Hommel P. Challenges for the German Health Care System. Z Gastroenterol. 2012;50:557-572. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Van Assche G, Dignass A, Panes J, Beaugerie L, Karagiannis J, Allez M, Ochsenkühn T, Orchard T, Rogler G, Louis E. The second European evidence-based Consensus on the diagnosis and management of Crohn’s disease: Definitions and diagnosis. J Crohns Colitis. 2010;4:7-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 818] [Cited by in F6Publishing: 776] [Article Influence: 55.4] [Reference Citation Analysis (0)] |
| 26. | Schmidt S, Lepori D, Meuwly JY, Duvoisin B, Meuli R, Michetti P, Felley C, Schnyder P, van Melle G, Denys A. Prospective comparison of MR enteroclysis with multidetector spiral-CT enteroclysis: interobserver agreement and sensitivity by means of “sign-by-sign” correlation. Eur Radiol. 2003;13:1303-1311. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 110] [Cited by in F6Publishing: 115] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 27. | Horsthuis K, Bipat S, Bennink RJ, Stoker J. Inflammatory bowel disease diagnosed with US, MR, scintigraphy, and CT: meta-analysis of prospective studies. Radiology. 2008;247:64-79. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 436] [Cited by in F6Publishing: 402] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 28. | Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357:2277-2284. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6212] [Cited by in F6Publishing: 5560] [Article Influence: 327.1] [Reference Citation Analysis (3)] |
| 29. | Fraquelli M, Colli A, Casazza G, Paggi S, Colucci A, Massironi S, Duca P, Conte D. Role of US in detection of Crohn disease: meta-analysis. Radiology. 2005;236:95-101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 225] [Cited by in F6Publishing: 196] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 30. | Biancone L, Calabrese E, Petruzziello C, Onali S, Caruso A, Palmieri G, Sica GS, Pallone F. Wireless capsule endoscopy and small intestine contrast ultrasonography in recurrence of Crohn’s disease. Inflamm Bowel Dis. 2007;13:1256-1265. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 31. | Martínez MJ, Ripollés T, Paredes JM, Blanc E, Martí-Bonmatí L. Assessment of the extension and the inflammatory activity in Crohn’s disease: comparison of ultrasound and MRI. Abdom Imaging. 2009;34:141-148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 108] [Cited by in F6Publishing: 112] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 32. | Rapaccini GL, Pompili M, Orefice R, Covino M, Riccardi L, Cedrone A, Gasbarrini G. Contrast-enhanced power doppler of the intestinal wall in the evaluation of patients with Crohn disease. Scand J Gastroenterol. 2004;39:188-194. [PubMed] [Cited in This Article: ] |
| 33. | Allgayer H, Braden B, Dietrich CF. Transabdominal ultrasound in inflammatory bowel disease. Conventional and recently developed techniques--update. Med Ultrason. 2011;13:302-313. [PubMed] [Cited in This Article: ] |
| 34. | Hirche TO, Russler J, Braden B, Schuessler G, Zeuzem S, Wehrmann T, Seifert H, Dietrich CF. Sonographic detection of perihepatic lymphadenopathy is an indicator for primary sclerosing cholangitis in patients with inflammatory bowel disease. Int J Colorectal Dis. 2004;19:586-594. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 30] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 35. | Hirche TO, Russler J, Schröder O, Schuessler G, Kappeser P, Caspary WF, Dietrich CF. The value of routinely performed ultrasonography in patients with Crohn disease. Scand J Gastroenterol. 2002;37:1178-1183. [PubMed] [Cited in This Article: ] |
| 36. | Nylund K, Hausken T, Gilja OH. Ultrasound and inflammatory bowel disease. Ultrasound Q. 2010;26:3-15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 37. | Migaleddu V, Quaia E, Scanu D, Carla S, Bertolotto M, Campisi G, Sirigu D, Virgilio G. Inflammatory activity in Crohn’s disease: CE-US. Abdom Imaging. 2011;36:142-148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 38. | Pallotta N, Tomei E, Viscido A, Calabrese E, Marcheggiano A, Caprilli R, Corazziari E. Small intestine contrast ultrasonography: an alternative to radiology in the assessment of small bowel disease. Inflamm Bowel Dis. 2005;11:146-153. [PubMed] [Cited in This Article: ] |
| 39. | Pallotta N, Civitelli F, Di Nardo G, Vincoli G, Aloi M, Viola F, Capocaccia P, Corazziari E, Cucchiara S. Small intestine contrast ultrasonography in pediatric Crohn’s disease. J Pediatr. 2013;163:778-784.e1. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 40. | Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsøe CP, Piscaglia F, Wilson SR, Barr RG, Chammas MC. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver--update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultraschall Med. 2013;34:11-29. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 210] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 41. | Dietrich CF. [3D real time contrast enhanced ultrasonography,a new technique]. Rofo. 2002;174:160-163. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 31] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 42. | Dietrich CF, Averkiou MA, Correas JM, Lassau N, Leen E, Piscaglia F. An EFSUMB introduction into Dynamic Contrast-Enhanced Ultrasound (DCE-US) for quantification of tumour perfusion. Ultraschall Med. 2012;33:344-351. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 212] [Cited by in F6Publishing: 228] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 43. | Dietrich CF, Ignee A, Gebel M, Braden B, Schuessler G. [Imaging of the abdomen. Z Gastroenterol. 2002;40:965-970. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 44. | Hocke M, Dietrich CF. New technology--combined use of 3D contrast enhanced endoscopic ultrasound techniques. Ultraschall Med. 2011;32:317-318. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 45. | Piscaglia F, Nolsøe C, Dietrich CF, Cosgrove DO, Gilja OH, Bachmann Nielsen M, Albrecht T, Barozzi L, Bertolotto M, Catalano O. The EFSUMB Guidelines and Recommendations on the Clinical Practice of Contrast Enhanced Ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med. 2012;33:33-59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 663] [Cited by in F6Publishing: 659] [Article Influence: 54.9] [Reference Citation Analysis (0)] |
| 46. | Schreiber-Dietrich D, Dietrich CF. Contrast enhanced ultrasound (CEUS) and off-label use (in children). Ultraschall Med. 2012;33:295-296. [PubMed] [Cited in This Article: ] |
| 47. | Dietrich CF, Mäurer M, Riemer-Hommel P. Challenges for the German Health Care System - Pharmaceuticals. Endo heute. 2014;27:45-53. [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 48. | Bamber J, Cosgrove D, Dietrich CF, Fromageau J, Bojunga J, Calliada F, Cantisani V, Correas JM, D’Onofrio M, Drakonaki EE. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 1: Basic principles and technology. Ultraschall Med. 2013;34:169-184. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 756] [Cited by in F6Publishing: 690] [Article Influence: 62.7] [Reference Citation Analysis (0)] |
| 49. | Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, Klauser AS, Sporea I, Calliada F, Cantisani V. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: Clinical applications. Ultraschall Med. 2013;34:238-253. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 621] [Cited by in F6Publishing: 461] [Article Influence: 41.9] [Reference Citation Analysis (0)] |
| 50. | Di Nardo G, Aloi M, Oliva S, Civitelli F, Casciani E, Cucchiara S. Investigation of small bowel in pediatric Crohn’s disease. Inflamm Bowel Dis. 2012;18:1760-1776. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 51. | Maconi G, Radice E, Greco S, Bianchi Porro G. Bowel ultrasound in Crohn’s disease. Best Pract Res Clin Gastroenterol. 2006;20:93-112. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 88] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 52. | Adamek HE, Dietrich CF. [Imaging of the small intestine: current knowledge]. Internist (Berl). 2010;51:722-729. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 53. | Van Assche G, Dignass A, Reinisch W, van der Woude CJ, Sturm A, De Vos M, Guslandi M, Oldenburg B, Dotan I, Marteau P. The second European evidence-based Consensus on the diagnosis and management of Crohn’s disease: Special situations. J Crohns Colitis. 2010;4:63-101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 569] [Cited by in F6Publishing: 526] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 54. | Lipson A, Bartram CI, Williams CB, Slavin G, Walker-Smith J. Barium studies and ileoscopy compared in children with suspected Crohn’s disease. Clin Radiol. 1990;41:5-8. [PubMed] [Cited in This Article: ] |
| 55. | Halligan S, Nicholls S, Beattie RM, Saunders BP, Williams CB, Walker-Smith JA, Bartram CI. The role of small bowel radiology in the diagnosis and management of Crohn’s disease. Acta Paediatr. 1995;84:1375-1378. [PubMed] [Cited in This Article: ] |
| 56. | Borthne AS, Abdelnoor M, Rugtveit J, Perminow G, Reiseter T, Kløw NE. Bowel magnetic resonance imaging of pediatric patients with oral mannitol MRI compared to endoscopy and intestinal ultrasound. Eur Radiol. 2006;16:207-214. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 47] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 57. | Bremner AR, Griffiths M, Argent JD, Fairhurst JJ, Beattie RM. Sonographic evaluation of inflammatory bowel disease: a prospective, blinded, comparative study. Pediatr Radiol. 2006;36:947-953. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 72] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 58. | Drews BH, Barth TF, Hänle MM, Akinli AS, Mason RA, Muche R, Thiel R, Pauls S, Klaus J, von Boyen G. Comparison of sonographically measured bowel wall vascularity, histology, and disease activity in Crohn’s disease. Eur Radiol. 2009;19:1379-1386. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 59. | Parente F, Maconi G, Bollani S, Anderloni A, Sampietro G, Cristaldi M, Franceschelli N, Bianco R, Taschieri AM, Bianchi Porro G. Bowel ultrasound in assessment of Crohn’s disease and detection of related small bowel strictures: a prospective comparative study versus x ray and intraoperative findings. Gut. 2002;50:490-495. [PubMed] [Cited in This Article: ] |
| 60. | DiCandio G, Mosca F, Campatelli A, Bianchini M, D’Elia F, Dellagiovampaola C. Sonographic detection of postsurgical recurrence of Crohn disease. AJR Am J Roentgenol. 1986;146:523-526. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 51] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 61. | Dinkel E, Dittrich M, Peters H, Baumann W. Real-time ultrasound in Crohn’s disease: characteristic features and clinical implications. Pediatr Radiol. 1986;16:8-12. [PubMed] [Cited in This Article: ] |
| 62. | Haber HP, Busch A, Ziebach R, Stern M. Bowel wall thickness measured by ultrasound as a marker of Crohn’s disease activity in children. Lancet. 2000;355:1239-1240. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 80] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 63. | Cuffari C. Diagnostic Considerations in Pediatric Inflammatory Bowel Disease Management. Gastroenterol Hepatol. 2009;5:775-783. [Cited in This Article: ] |
| 64. | Sarrazin J, Wilson SR. Manifestations of Crohn disease at US. Radiographics. 1996;16:499-520; discussion 520-521. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 96] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 65. | Chaubal N, Dighe M, Shah M, Chaubal J. Sonography of the gastrointestinal tract. J Ultrasound Med. 2006;25:87-97. [PubMed] [Cited in This Article: ] |
| 66. | Valette PJ, Rioux M, Pilleul F, Saurin JC, Fouque P, Henry L. Ultrasonography of chronic inflammatory bowel diseases. Eur Radiol. 2001;11:1859-1866. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 65] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 67. | Panes J, Bouhnik Y, Reinisch W, Stoker J, Taylor SA, Baumgart DC, Danese S, Halligan S, Marincek B, Matos C. Imaging techniques for assessment of inflammatory bowel disease: joint ECCO and ESGAR evidence-based consensus guidelines. J Crohns Colitis. 2013;7:556-585. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 465] [Cited by in F6Publishing: 478] [Article Influence: 43.5] [Reference Citation Analysis (0)] |
| 68. | Hollerweger A, Macheiner P, Dirks K, Dietrich CF. [Differential diagnosis of severe hypoechoic oedema of the small bowel]. Ultraschall Med. 2006;27:234-239. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 69. | Maconi G, Bollani S, Bianchi Porro G. Ultrasonographic detection of intestinal complications in Crohn’s disease. Dig Dis Sci. 1996;41:1643-1648. [PubMed] [Cited in This Article: ] |
| 70. | Maconi G, Sampietro GM, Russo A, Bollani S, Cristaldi M, Parente F, Dottorini F, Bianchi Porro G. The vascularity of internal fistulae in Crohn’s disease: an in vivo power Doppler ultrasonography assessment. Gut. 2002;50:496-500. [PubMed] [Cited in This Article: ] |
| 71. | Orsoni P, Barthet M, Portier F, Panuel M, Desjeux A, Grimaud JC. Prospective comparison of endosonography, magnetic resonance imaging and surgical findings in anorectal fistula and abscess complicating Crohn’s disease. Br J Surg. 1999;86:360-364. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 162] [Cited by in F6Publishing: 165] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 72. | Pera A, Cammarota T, Comino E, Caldera D, Ponti V, Astegiano M, Barletti C, Rocca R, Cosimato M, Bertolusso L. Ultrasonography in the detection of Crohn’s disease and in the differential diagnosis of inflammatory bowel disease. Digestion. 1988;41:180-184. [PubMed] [Cited in This Article: ] |
| 73. | Seitz K, Reuss J. [Sonographic detection of fistulas in Crohn disease]. Ultraschall Med. 1986;7:281-283. [PubMed] [DOI] [Cited in This Article: ] |
| 74. | Di Mizio R, Maconi G, Romano S, D’Amario F, Bianchi Porro G, Grassi R. Small bowel Crohn disease: sonographic features. Abdom Imaging. 2004;29:23-35. [PubMed] [Cited in This Article: ] |
| 75. | Sturm EJ, Cobben LP, Meijssen MA, van der Werf SD, Puylaert JB. Detection of ileocecal Crohn’s disease using ultrasound as the primary imaging modality. Eur Radiol. 2004;14:778-782. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 76. | Furukawa A, Saotome T, Yamasaki M, Maeda K, Nitta N, Takahashi M, Tsujikawa T, Fujiyama Y, Murata K, Sakamoto T. Cross-sectional imaging in Crohn disease. Radiographics. 2004;24:689-702. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 194] [Cited by in F6Publishing: 199] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 77. | Guimarães LS, Fidler JL, Fletcher JG, Bruining DH, Huprich JE, Siddiki H, Sandborn WJ, Loftus EV, Pardi DS, McCollough CH. Assessment of appropriateness of indications for CT enterography in younger patients. Inflamm Bowel Dis. 2010;16:226-232. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 78. | Gaca AM, Jaffe TA, Delaney S, Yoshizumi T, Toncheva G, Nguyen G, Frush DP. Radiation doses from small-bowel follow-through and abdomen/pelvis MDCT in pediatric Crohn disease. Pediatr Radiol. 2008;38:285-291. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 71] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 79. | Bender GN, Timmons JH, Williard WC, Carter J. Computed tomographic enteroclysis: one methodology. Invest Radiol. 1996;31:43-49. [PubMed] [Cited in This Article: ] |
| 80. | Dietrich CF, Zeuzem S, Caspary WF, Wehrmann T. [Ultrasound lymph node imaging in the abdomen and retroperitoneum of healthy probands]. Ultraschall Med. 1998;19:265-269. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 81. | Maconi G, Di Sabatino A, Ardizzone S, Greco S, Colombo E, Russo A, Cassinotti A, Casini V, Corazza GR, Bianchi Porro G. Prevalence and clinical significance of sonographic detection of enlarged regional lymph nodes in Crohn’s disease. Scand J Gastroenterol. 2005;40:1328-1333. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 82. | Puylaert JB, van der Zant FM. Mesenteric lymphadenitis or appendicitis? AJR Am J Roentgenol. 1995;165:490. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 83. | Primas C, Novacek G, Schweiger K, Mayer A, Eser A, Papay P, Gratzer C, Angelberger S, Dejaco C, Reinisch W. Renal insufficiency in IBD--prevalence and possible pathogenetic aspects. J Crohns Colitis. 2013;7:e630-e634. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 84. | Worlicek H, Lutz H, Thoma B. Sonography of chronic inflammatory bowel diseases--a prospective study. Ultraschall Med. 1986;7:275-280. [PubMed] [DOI] [Cited in This Article: ] |
| 85. | Maconi G, Sampietro GM, Parente F, Pompili G, Russo A, Cristaldi M, Arborio G, Ardizzone S, Matacena G, Taschieri AM. Contrast radiology, computed tomography and ultrasonography in detecting internal fistulas and intra-abdominal abscesses in Crohn’s disease: a prospective comparative study. Am J Gastroenterol. 2003;98:1545-1555. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 156] [Cited by in F6Publishing: 140] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 86. | Loonen HJ, Griffiths AM, Merkus MP, Derkx HH. A critical assessment of items on the Pediatric Crohn‘s Disease Activity Index. J Pediatr Gastroenterol Nutr. 2003;36:90-95. [PubMed] [Cited in This Article: ] |
| 87. | Hyams J, Markowitz J, Otley A, Rosh J, Mack D, Bousvaros A, Kugathasan S, Pfefferkorn M, Tolia V, Evans J. Evaluation of the pediatric crohn disease activity index: a prospective multicenter experience. J Pediatr Gastroenterol Nutr. 2005;41:416-421. [PubMed] [Cited in This Article: ] |
| 88. | Hata J, Haruma K, Suenaga K, Yoshihara M, Yamamoto G, Tanaka S, Shimamoto T, Sumii K, Kajiyama G. Ultrasonographic assessment of inflammatory bowel disease. Am J Gastroenterol. 1992;87:443-447. [PubMed] [Cited in This Article: ] |
| 89. | Futagami Y, Haruma K, Hata J, Fujimura J, Tani H, Okamoto E, Kajiyama G. Development and validation of an ultrasonographic activity index of Crohn’s disease. Eur J Gastroenterol Hepatol. 1999;11:1007-1012. [PubMed] [Cited in This Article: ] |
| 90. | Dietrich CF, Brunner V, Lembcke B. [Intestinal ultrasound in rare small and large intestinal diseases]. Z Gastroenterol. 1998;36:955-970. [PubMed] [Cited in This Article: ] |
| 91. | Adler J, Stidham RW, Higgins PDR. Bringing the Inflamed and Fibrotic Bowel into Focus: Imaging in Inflammatory Bowel Disease. Gastroenterol Hepatol. 2009;5:705-715. [Cited in This Article: ] |
| 92. | Bozkurt T, Richter F, Lux G. Ultrasonography as a primary diagnostic tool in patients with inflammatory disease and tumors of the small intestine and large bowel. J Clin Ultrasound. 1994;22:85-91. [PubMed] [Cited in This Article: ] |
| 93. | Erdozain JC, Herrera A, Molina E, Conde P, Moreno A, Olveira A, Martínez A, Segura JM. [Usefulness of abdominal echography in the diagnosis of active Crohn’s disease]. Gastroenterol Hepatol. 1998;21:272-276. [PubMed] [Cited in This Article: ] |
| 94. | Hollerbach S, Geissler A, Schiegl H, Kullmann F, Lock G, Schmidt J, Schlegel J, Schoelmerich J, Andus T. The accuracy of abdominal ultrasound in the assessment of bowel disorders. Scand J Gastroenterol. 1998;33:1201-1208. [PubMed] [Cited in This Article: ] |
| 95. | Khaw KT, Yeoman LJ, Saverymuttu SH, Cook MG, Joseph AE. Ultrasonic patterns in inflammatory bowel disease. Clin Radiol. 1991;43:171-175. [PubMed] [Cited in This Article: ] |
| 96. | Maconi G, Parente F, Bollani S, Cesana B, Bianchi Porro G. Abdominal ultrasound in the assessment of extent and activity of Crohn’s disease: clinical significance and implication of bowel wall thickening. Am J Gastroenterol. 1996;91:1604-1609. [PubMed] [Cited in This Article: ] |
| 97. | Nuernberg D, Ignee A, Dietrich CF. [Current status of ultrasound in gastroenterology--bowel and upper gastrointestinal tract--part 1]. Z Gastroenterol. 2007;45:629-640. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 98. | Spalinger J, Patriquin H, Miron MC, Marx G, Herzog D, Dubois J, Dubinsky M, Seidman EG. Doppler US in patients with crohn disease: vessel density in the diseased bowel reflects disease activity. Radiology. 2000;217:787-791. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 187] [Cited by in F6Publishing: 161] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 99. | Parente F, Greco S, Molteni M, Anderloni A, Maconi G, Bianchi Porro G. Modern imaging of Crohn’s disease using bowel ultrasound. Inflamm Bowel Dis. 2004;10:452-461. [PubMed] [Cited in This Article: ] |
| 100. | Sandhu BK, Fell JM, Beattie RM, Mitton SG, Wilson DC, Jenkins H. Guidelines for the management of inflammatory bowel disease in children in the United Kingdom. J Pediatr Gastroenterol Nutr. 2010;50 Suppl 1:S1-13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 107] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 101. | Civitelli F, Di Nardo G, Oliva S, Nuti F, Ferrari F, Dilillo A, Viola F, Pallotta N, Cucchiara S, Aloi M. Ultrasonography of the colon in pediatric ulcerative colitis: a prospective, blind, comparative study with colonoscopy. J Pediatr. 2014;165:78-84.e2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 102. | Britton I, Maguire C, Adams C, Russell RI, Leen E. Assessment of the role and reliability of sonographic post-prandial flow response in grading Crohn’s disease activity. Clin Radiol. 1998;53:599-603. [PubMed] [Cited in This Article: ] |
| 103. | Dietrich CF, Ignee A, Seitz KH, Caspary WF. [Duplex sonography of visceral arteries]. Ultraschall Med. 2001;22:247-257. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 104. | Esteban JM, Maldonado L, Sanchiz V, Minguez M, Benages A. Activity of Crohn’s disease assessed by colour Doppler ultrasound analysis of the affected loops. Eur Radiol. 2001;11:1423-1428. [PubMed] [Cited in This Article: ] |
| 105. | Ludwig D. Doppler sonography in inflammatory bowel disease. Z Gastroenterol. 2004;42:1059-1065. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 106. | Maconi G, Parente F, Bollani S, Imbesi V, Ardizzone S, Russo A, Bianchi Porro G. Factors affecting splanchnic haemodynamics in Crohn’s disease: a prospective controlled study using Doppler ultrasound. Gut. 1998;43:645-650. [PubMed] [Cited in This Article: ] |
| 107. | Neye H, Voderholzer W, Rickes S, Weber J, Wermke W, Lochs H. Evaluation of criteria for the activity of Crohn’s disease by power Doppler sonography. Dig Dis. 2004;22:67-72. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 65] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 108. | Nuernberg D, Ignee A, Dietrich CF. [Current status of ultrasound in gastroenterology--bowel and upper gastrointestinal tract--part 2]. Z Gastroenterol. 2008;46:355-366. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 109. | Onali S, Calabrese E, Petruzziello C, Zorzi F, Sica GS, Lolli E, Ascolani M, Condino G, Pallone F, Biancone L. Endoscopic vs ultrasonographic findings related to Crohn’s disease recurrence: a prospective longitudinal study at 3 years. J Crohns Colitis. 2010;4:319-328. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 110. | Parente F, Greco S, Molteni M, Anderloni A, Sampietro GM, Danelli PG, Bianco R, Gallus S, Bianchi Porro G. Oral contrast enhanced bowel ultrasonography in the assessment of small intestine Crohn’s disease. A prospective comparison with conventional ultrasound, x ray studies, and ileocolonoscopy. Gut. 2004;53:1652-1657. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 150] [Cited by in F6Publishing: 145] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 111. | Scholbach T, Herrero I, Scholbach J. Dynamic color Doppler sonography of intestinal wall in patients with Crohn disease compared with healthy subjects. J Pediatr Gastroenterol Nutr. 2004;39:524-528. [PubMed] [Cited in This Article: ] |
| 112. | van Oostayen JA, Wasser MN, Griffioen G, van Hogezand RA, Lamers CB, de Roos A. Activity of Crohn’s disease assessed by measurement of superior mesenteric artery flow with Doppler ultrasound. Neth J Med. 1998;53:S3-S8. [PubMed] [Cited in This Article: ] |
| 113. | van Oostayen JA, Wasser MN, van Hogezand RA, Griffioen G, de Roos A. Activity of Crohn disease assessed by measurement of superior mesenteric artery flow with Doppler US. Radiology. 1994;193:551-554. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 73] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 114. | Karoui S, Nouira K, Serghini M, Ben Mustapha N, Boubaker J, Menif E, Filali A. Assessment of activity of Crohn’s disease by Doppler sonography of superior mesenteric artery flow. J Crohns Colitis. 2010;4:334-340. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 115. | Nylund K, Ødegaard S, Hausken T, Folvik G, Lied GA, Viola I, Hauser H, Gilja OH. Sonography of the small intestine. World J Gastroenterol. 2009;15:1319-1330. [PubMed] [Cited in This Article: ] |
| 116. | Ruess L, Blask AR, Bulas DI, Mohan P, Bader A, Latimer JS, Kerzner B. Inflammatory bowel disease in children and young adults: correlation of sonographic and clinical parameters during treatment. AJR Am J Roentgenol. 2000;175:79-84. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 66] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 117. | Albrecht T, Blomley M, Bolondi L, Claudon M, Correas JM, Cosgrove D, Greiner L, Jäger K, Jong ND, Leen E. Guidelines for the use of contrast agents in ultrasound. January 2004. Ultraschall Med. 2004;25:249-256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 297] [Cited by in F6Publishing: 211] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 118. | Claudon M, Cosgrove D, Albrecht T, Bolondi L, Bosio M, Calliada F, Correas JM, Darge K, Dietrich C, D’Onofrio M. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) - update 2008. Ultraschall Med. 2008;29:28-44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 526] [Cited by in F6Publishing: 483] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 119. | Dietrich CF. Comments and illustrations regarding the guidelines and good clinical practice recommendations for contrast-enhanced ultrasound (CEUS)--update 2008. Ultraschall Med. 2008;29 Suppl 4:S188-S202. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 120. | Dietrich CF, Cui XW, Schreiber-Dietrich DG, Ignee A. EFSUMB guidelines 2011: comments and illustrations. Ultraschall Med. 2012;33 Suppl 1:S11-S21. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 121. | Serra C, Menozzi G, Labate AM, Giangregorio F, Gionchetti P, Beltrami M, Robotti D, Fornari F, Cammarota T. Ultrasound assessment of vascularization of the thickened terminal ileum wall in Crohn’s disease patients using a low-mechanical index real-time scanning technique with a second generation ultrasound contrast agent. Eur J Radiol. 2007;62:114-121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 96] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 122. | Dietrich CF, Jedrzejczyk M, Ignee A. Sonographic assessment of splanchnic arteries and the bowel wall. Eur J Radiol. 2007;64:202-212. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 123. | Dietrich CF. Significance of abdominal ultrasound in inflammatory bowel disease. Dig Dis. 2009;27:482-493. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 124. | Dietrich CF, Cui XW, Barreiros AP, Hocke M, Ignee A. EFSUMB guidelines 2011: comment on emergent indications and visions. Ultraschall Med. 2012;33 Suppl 1:S39-S47. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 125. | Dietrich CF, Ignee A, Hocke M, Schreiber-Dietrich D, Greis C. Pitfalls and artefacts using contrast enhanced ultrasound. Z Gastroenterol. 2011;49:350-356. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 126. | Dietrich CF, Schreiber-Dietrich D, Hocke M. [Comments on the EFSUMB non-liver Guidelines 2011]. Praxis (Bern 1994). 2012;101:1175-1181. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 127. | Guidi L, De Franco A, De Vitis I, Armuzzi A, Semeraro S, Roberto I, Papa A, Bock E, Gasbarrini G, Fedeli G. Contrast-enhanced ultrasonography with SonoVue after infliximab therapy in Crohn’s disease. Eur Rev Med Pharmacol Sci. 2006;10:23-26. [PubMed] [Cited in This Article: ] |
| 128. | Allgayer H, Ignee A, Dietrich CF. Endosonographic elastography of the anal sphincter in patients with fecal incontinence. Scand J Gastroenterol. 2010;45:30-38. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 129. | Dietrich CF, Hocke M, Jenssen C. [Interventional endosonography]. Ultraschall Med. 2011;32:8-22, quiz 23-25. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 130. | Dietrich CF, Jenssen C. [Evidence based endoscopic ultrasound]. Z Gastroenterol. 2011;49:599-621. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 131. | Dietrich CF, Săftoiu A, Jenssen C. Real time elastography endoscopic ultrasound (RTE-EUS), a comprehensive review. Eur J Radiol. 2014;83:405-414. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 132. | Dietrich CF, Cantisani V. Current status and perspectives of elastography. Eur J Radiol. 2014;83:403-404. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 133. | Ishikawa D, Ando T, Watanabe O, Ishiguro K, Maeda O, Miyake N, Nakamura M, Miyahara R, Ohmiya N, Hirooka Y. Images of colonic real-time tissue sonoelastography correlate with those of colonoscopy and may predict response to therapy in patients with ulcerative colitis. BMC Gastroenterol. 2011;11:29. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |