Published online Oct 14, 2015. doi: 10.3748/wjg.v21.i38.10714
Peer-review started: May 6, 2015
First decision: June 23, 2015
Revised: July 14, 2015
Accepted: September 15, 2015
Article in press: September 15, 2015
Published online: October 14, 2015
Approximately 240 million people are chronically infected with hepatitis B virus (HBV), 75% of whom reside in Asia. Approximately 600000 of infected patients die each year due to HBV-related diseases or hepatocellular carcinoma (HCC). The endemicity of hepatitis surface antigen in Indonesia is intermediate to high with a geographical difference. The risk of HBV infection is high in hemodialysis (HD) patients, men having sex with men, and health care workers. Occult HBV infection has been detected in various groups such as blood donors, HD patients, and HIV-infected individuals and children. The most common HBV subgenotype in Indonesia is B3 followed by C1. Various novel subgenotypes of HBV have been identified throughout Indonesia, with the novel HBV subgenotypes C6-C16 and D6 being successfully isolated. Although a number of HBV subgenotypes have been discovered in Indonesia, genotype-related pathogenicity has not yet been elucidated in detail. Therefore, genotype-related differences in the prognosis of liver disease and their effects on treatments need to be determined. A previous study conducted in Indonesia revealed that hepatic steatosis was associated with disease progression. Pre-S2 mutations and mutations at C1638T and T1753V in HBV/B3 have been associated with advanced liver diseases including HCC. However, drug resistance to lamivudine, which is prominent in Indonesia, remains obscure. Although the number of studies on HBV in Indonesia has been increasing, adequate databases on HBV infection are limited. We herein provided an overview of the epidemiology and clinical characteristics of HBV infection in Indonesia.
Core tip: Hepatitis B virus (HBV) infection is an important public concern and its prevalence varies greatly in different parts of the world. The high prevalence of HBV in Indonesia highlights the need to improve prevention and control measures because few evidence-based prevention strategies are currently available. Although studies on HBV in Indonesia are increasing, it is still not fully understood. We herein reviewed epidemiologically important aspects of HBV infection in Indonesia.
- Citation: Yano Y, Utsumi T, Lusida MI, Hayashi Y. Hepatitis B virus infection in Indonesia. World J Gastroenterol 2015; 21(38): 10714-10720
- URL: https://www.wjgnet.com/1007-9327/full/v21/i38/10714.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i38.10714
Hepatitis B virus (HBV) infection is associated with a diverse range of liver damage including asymptomatic carriers, chronic hepatitis, liver cirrhosis, and hepatocellular carcinoma (HCC). Approximately 240 million people are chronically infected with HBV[1], 75% of whom reside in Asia[2]. Approximately 600000 of infected patients die each year of HBV-related diseases or HCC[3]. The prevalence of HBV infection varies according to the geographic region, and is categorized as high (≥ 8%), intermediate (2%-7%), or low (< 2%) endemicity. The endemicity of HBV in Indonesia is moderate to high[4,5], ranging from 2.5% to 10% for hepatitis B surface antigen (HBsAg)[2,5,6]. HBV has been classified into at least 9 genotypes (A through H and J) and has been shown to have a distinct geographical distribution[7,8]. The most common HBV subgenotype is HBV B3 (HBV/B3), followed by HBV/C1[9]; however, various novel genotypes have been detected in Indonesia.
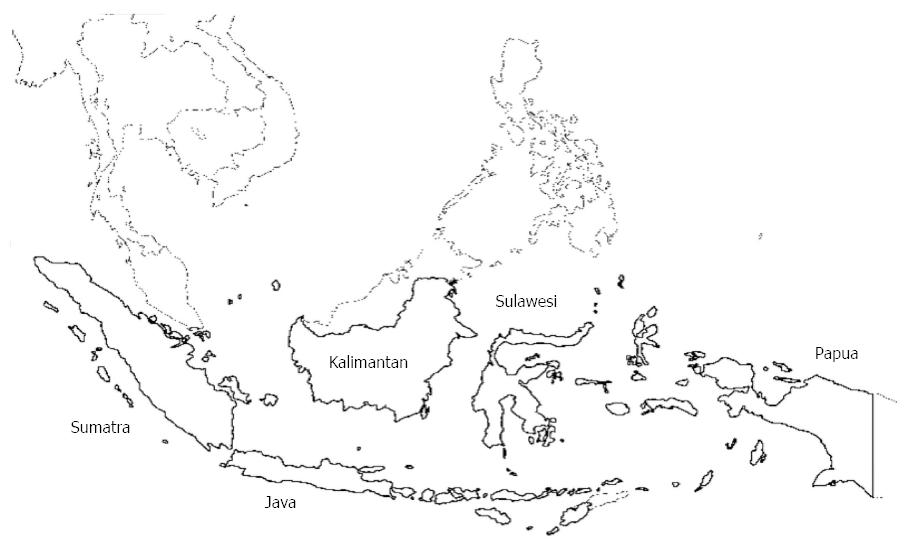
Indonesia is the largest archipelago in the world, consisting of five major islands and approximately 30 smaller groups. The archipelago is located between two oceans, the Pacific and Indian oceans, and bridges two continents, Asia and Australia. This strategic position has influenced the serological and virological aspects of HBV infection (Figure 1). Although the number of studies conducted on HBV in Indonesia has increased, adequate databases on HBV infection are still limited[10]. The epidemiology of HBV remains obscure in Indonesia[11]. Therefore, we herein provided an overview of HBV infection among the Indonesian population.
The prevalence of chronic HBV infection varies greatly in different areas of the world and the prevalence of chronic HBV infection can be categorized as high, intermediate, or low endemicity. Table 1 shows the prevalence of the HBsAg in not only the general population, but also risk groups such as commercial sex workers (CSW) and men having sex with men (MSM). The prevalence of HBV in the general population in Indonesia is higher than that of HCV (2%)[12], with the highest rates being reported in Makassar (7.1%)[13] in Sulawesi Island and the lowest rates being reported in Jakarta (4.0%)[14] in Java Island; however, another study reported that the prevalence of HBV in Jakarta was 5.8% in the general population[15]. Hasan previously reported that the prevalence of HBV infection in the general population was the highest in Pontianak (9.1%) in the Kalimantan Island[5]. Furthermore, the prevalence of HBsAg was markedly higher in habitants in the highland of Papua (12.8%) and North Sulawesi (33.0%)[16]. The prevalence of HBsAg in pregnant women was found to be the same as that in the general population in Indonesia[17,18]. These findings demonstrated that the endemicity of HBsAg among the general population in Indonesia is intermediate to high, as reported previously[2,19].
| Region | Prevalence (%) | Subject | Main genotype | Ref. |
| Java | ||||
| Bandung | 4.7 | Pregnant women | Reniers et al[17], 1987 | |
| Jakarta | 4.0 | General population | Akbar et al[14], 1997 | |
| Jakarta | 5.8 | General population | Budihusodo et al[15], 1991 | |
| Jakarta | 2.2 | Parturient women | Gunardi et al[6], 2014 | |
| Surabaya | 4.0 | CSW | Kotaki et al[26], 2013 | |
| Solo | 9.8 | MSM | Prasetyo et al[21], 2014 | |
| Four prisons in Central Java1 | 3.2 | Drug abuser inmates in prisons | B3, C1 | Prasetyo et al[10], 2013 |
| Yogyakarta | 11.2 | HD patients | B3 | Rinonce et al[12], 2013 |
| 5.7 | Staff in HDU | B3 | ||
| Sumatra | ||||
| Padang | HBV carriers | C1, B3 | Siburian et al[9], 2013 | |
| Kalimantan | ||||
| Banjarmasin | 4.6 | General population | B, C | Darmawan et al[32], 2015 |
| Sulawesi | ||||
| Tahuna | 4.9 | General population | C5 | Achwan et al[11], 2007 |
| Makassar | 7.1 | General population | Amirudin et al[13], 1991 | |
| Bali1 | 1.9 | Pregnant women | Surya et al[18], 2005 | |
| Papua | ||||
| Jayapura | 4.6 | General population | C6, D6, B3 | Lusida et al[36], 2008 |
HBV infection was not detected in children in Tahuna, North Sulawesi, and Surabaya, East Java, suggesting the efficacy of Hepatitis B (HB) vaccinations in pre-school children[11,20].
The highest risk group of HBV infection was previously reported to be hemodialysis (HD) patients (11.2%) in Yogyakarta[12], followed by MSM (9.8%)[21] in Solo in the Java Island (Table 1). The prevalence of HBV/HIV co-infection was found to be higher than that of HBV infection alone in Indonesia[22-24] as well as in neighboring countries such as Vietnam and India. The incidence of HIV and HBV burden are currently increasing in Indonesia[22,23,25]; however, no HBV/HIV co-infection cases have been identified in CSW[26]. The prevalence of HBsAg has been classified as high endemicity (8.8%) in health care workers[27] and intermediate endemicity in staff in HDU (5.7%) throughout Indonesia (Table 1). A previous study also revealed that the prevalence of HBsAg was high among medical employees in Padang (11.2%), Mataram (13.3%), and Irian Jaya (13.3%)[5].
Many unique animals exist in Indonesia because of its specific ecosystem. Gibbons in Kalimantan were previously reported to be infected with HBV having their own genotype[28].
Occult HBV infection (OBI) is defined as the presence of HBV DNA in the serum and/or liver tissue of individuals with HBV core antibodies (anti-HBc) without HBsAg[29]. Several studies have been conducted on OBI in Indonesia. OBI was detected in 8.1% of blood donors with amino acid mutations (T123A, M133L, and T143M) in the a determinant of HBsAg, which resulted in changes in predicted antigenicity[30]. Several OBI cases were detected among school children with the variant T126I, which may be one of the viral mechanisms helping the virus to escape from current HB vaccines in Indonesia[31]. In Banjarmasin, Kalimantan, OBI was identified in healthy young adults with 13 amino acid substitutions[32]. Awareness of the reactivation of OBI has increased in Indonesia, especially in HBV endemic areas[33]. A total of 27.1% and 14.7% of HIV-infected individuals and HD patients, respectively, were considered to have OBI[12,22], suggesting that the prevalence of HBV infection regardless of HBsAg was high in immunosuppressive patients.
HBV is currently grouped into at least 9 genotypes (A through H and J, with I still being controversial)[34]. The HBV sequence is characterized by more than 8% nucleotide (nt) differences for genotypes and 4%-8% for subgenotypes. The most common HBV subgenotype in Indonesia is HBV/B3, followed by HBV/C1[35,36] (Table 1), with various novel subgenotypes of HBV being identified throughout Indonesia. Ten novel HBV subgenotypes (HBV/C7-C16) were isolated in Indonesia between 2008 and 2012[37-41]. HBV/C6, HBV/C11, and HBV/D6 were identified in a Papuan population[36,40,42]. Genotype J (HBV/J) was detected in a Japanese patient with HCC who was thought to have been infected in Kalimantan, Indonesia, during World War II[28,43]. HBV isolates from subjects from Sulawesi clustered within the HBV/C5, together with known isolates from the Philippines and Vietnam[11]. The distribution of genotypes/subgenotypes varies even in different regions of a country, which may partly be related to the ethnic origin of the infected patients.
The most significant achievement in the prevention of HB is the implementation of a universal infant vaccination for HB. The HB universal vaccination was introduced in Indonesia in 1997, with the Indonesian government attempting to ensure that every newborn was vaccinated against HBV infection during the first 7 d of life. The immunization project in Lombok decreased the prevalence of HBsAg from 6.2% to 1.4% among children less than 5 years old[44]. In Surabaya and North Sulawesi, the prevalence of HBsAg in preschool children was reported to be 0%[11,20], a result that was attributed to the universal HB vaccination. Although the prevalence of HBsAg among children varies by region, for example, 3.1% in Lamongan in East Java[31] and 4.2% in Papua, the HB vaccination history is obscure. Since the HB vaccination is one of the Expanded Program on Immunization projects being run by the government, communication with the local government is of great importance for better practices.
Previous studies revealed that the clinical characteristics of chronic HB (CHB) differed among genotypes, and the prognosis of genotype B was better than that of genotype C[45-47]. However, most studies in Asia were conducted in Taiwan, China, Hong Kong, and Japan. The main subgenotype in Indonesia is HBV/B3, which is different from the subgenotypes HBV/B1 and HBV/B2 mainly analyzed in other Asian countries[48]. Furthermore, HBV/C in Indonesia is mainly HBV/C1 in Java and HBV/C6 in Papua, and is different from HBV/C, which is spreading in East Asian countries such as China and Japan[36,42]. Since most clinical studies conducted in Indonesia involved patients with HBV/B, the clinical course of HBV/C in Indonesia currently remains unclear. Although HCC is prevalent in Indonesia, further studies are needed to determine clinical characteristics in relation to the genotypes in Indonesia.
Recent studies revealed that hepatic steatosis was associated with disease progression[49]. Steatosis was identified as an independent risk factor for HCC and the progression of hepatitis was found to be more rapid in HCV patients with steatosis[50,51]. However, a meta-analysis revealed that hepatic steatosis was not related to the clinical course of HBV patients[52]. A previous study reported that hepatic steatosis was more strongly associated with genotype C (37.9%) than with genotype B (24.0%)[53]. Lesmana et al[54] examined 179 CHB patients in Jakarta and found the prevalence of hepatic steatosis to be approximately 30%. Obesity is a serious social issue in Indonesia, as in other countries[55]. However, studies on steatosis in Indonesia are still limited, and, as such, further investigations are warranted.
Although the prevalence of HBV and HCV infections in Southeast Asia including Indonesia is high, clinical studies remain limited. Lamivudine, adefovir, and telbivudine, therapeutic drugs for CHB, are currently covered by health insurance in Indonesia. Although drug resistance to lamivudine has not yet been examined, it is common for the cheapest drug, lamivudine, to be prescribed or antiviral therapy to be discontinued due to economic reasons. Therefore, the prevalence of lamivudine-resistant HBV may increase. Telbivudine, which was recently approved in Indonesia, was found to be effective for Indonesian HBV carriers. Sulaiman et al[56] reported that HBeAg loss and the seroconversion rate for HBeAg-positive patients were 28.8% and 14.1% at week 52 of telbivudine therapy, respectively. Furthermore, undetectable HBV DNA (PCR negativity) was 51.8% at week 24 and 62.7% at week 52 of this therapy. However, a large-scale study has not yet been conducted on interferon therapy for CHB and, thus, its effectiveness currently remains unknown.
Previous studies revealed a hepatitis virus co-infection among HIV patients. Anggorowati et al[23] examined 126 HIV patients in Yogyakarta city and found that 8% had the HBsAg and were considered to be co-infected with HBV. Utsumi et al[22] examined 118 HIV patients in Surabaya City, and reported that 15.3% were HBsAg-positive while 27.1% were positive for HBV-DNA regardless of being HBsAg-negative and were considered to have OBI. These findings suggested that HBV co-infection including OBI was frequent among HIV patients and serological examinations were sometimes insufficient for detecting co-infections because of a compromised immune system. Fibriani et al[24] recently examined 616 HIV patients in Bandung city in West Java, found HBV co-infection in approximately 7% of these patients, and identified the clinical characteristics of co-infection as being male and having a history of injection drug use.
HBV infection was examined in HD patients. Rinonce et al[12] examined 161 HD patients in Yogyakarta, and revealed that the prevalence of HBsAg positivity was 11.8% and also that the viral genomes of several strains were identical, suggesting nosocomial infection.
Cancer-related death is a major public health problem in Indonesia and accounts for the seventh largest cause of death. According to the Jakarta Cancer Registry, the ratio of liver cancer between 2005 and 2007 was 1.4 per 100000 (eleventh place) among women and 4.0 per 100000 (third place) among men[57]. On the other hand, HBV is the most common cause of HCC. Sulaiman[58] and Marwoto et al[59] firstly reported in 1985 that the frequency of HBV among HCC was 67.0%, while Sulaiman showed that it was 47.6%. Wang et al[60] examined the epidemiology of HCC in Japan, India, China, and Indonesia, and found that the positive prevalences of the HBsAg and HCV antibody were 21.0% and 40.0% in Indonesian patients with liver cancer, respectively. HBV is a well-known oncogenic virus, and previous studies revealed that the Pre-S mutation, X mutation, and BCP-PC mutation were associated with hepatocarcinogenesis[61,62]. The Pre-S1 deletion, Pre-S2 deletion, T53C mutation were found to be related to HCC at the S domain. Utama et al[63] examined the prevalence of the Pre-S2 mutation among 268 HBV carriers in Bantan, and showed it was 2.7%, 18.2%, 40.9%, and 28.6% in asymptomatic carriers, chronic hepatitis, liver cirrhosis, and HCC, respectively, indicating that the Pre-S2 mutation was an independent factor of progressive liver disease. A meta-analysis revealed that the X domain including an A1762T/G1764A double mutant, T1753V, C1653T, G1896A, and G1899A were related to HCC[64]. Heriyanto et al[35] compared 40 cirrhosis and liver cancer patients with 109 chronic hepatitis patients in Yogyakarta city, and a multivariate analysis identified being older than 45 years old (OR = 2.61, P = 0.034), having a C1638T variation (OR = 1074.57, P = 0.005), and having a T1753V variation (OR = 6.39, P = 0.047) as independent factors participating in disease progression.
Recent technological advances revealed that various kinds of genetic factors are associated with cancers. The genome-wide association study showed that a large number of single nucleotide polymorphisms (SNPs) were related to various kinds of cancers. In case-control and retrospective studies on liver cancers, numerous candidate genes for SNPs were found to be associated with HCC. In 2009, Kamatani et al[65] examined 188 Japanese CHB patients and 934 controls and was the first to show that SNPs in the human leukocyte antigen (HLA)-DP region were associated with chronic HBV carriers. The HLA gene is located in 6p21.3 and plays an important role in antigen presentation. Polymorphisms in this region were also identified not only in Japanese patients, but also in Chinese patients[66,67]. In Indonesian populations, several SNPs including rs3135363 in HLA-DR, rs9277535 in HLA-DP, and rs9267665 in a gene-rich HLA class III interval were associated with HB vaccine responses[68]. Host factors are also important for HBV infection and disease progression. Further analyses are needed to confirm these findings.
The endemicity of HBsAg in Indonesia is intermediate to high with a geographical difference. HD patients, MSM, and health care workers are at high risk of HBV infection. OBI has also been detected in various groups such as blood donors, HD patients, and HIV-infected individuals and children. Appropriate national immunization programs are required in HBV endemic countries such as Indonesia in order to reduce HBV infection. Although a number of HBV subgenotypes have been discovered in Indonesia, genotype-related pathogenicity has not yet been elucidated in detail. Therefore, genotype-related differences in the prognosis of liver disease and their effects on treatments are eagerly awaited.
P- Reviewer: Blum HE, Chen RF S- Editor: Yu J L- Editor: A E- Editor: Ma S
| 1. | HIV/AIDS Programme. Guidance on prevention of viral hepatitis B and C among people WHO inject drugs. WHO. 2012; Available from: http://apps.who.int/iris/bitstream/10665/75357/1/9789241504041_eng.pdf. [Cited in This Article: ] |
| 2. | Merican I, Guan R, Amarapuka D, Alexander MJ, Chutaputti A, Chien RN, Hasnian SS, Leung N, Lesmana L, Phiet PH. Chronic hepatitis B virus infection in Asian countries. J Gastroenterol Hepatol. 2000;15:1356-1361. [PubMed] [Cited in This Article: ] |
| 3. | Abbas Z, Siddiqui AR. Management of hepatitis B in developing countries. World J Hepatol. 2011;3:292-299. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Fitria L, Gunardi H, Akib AAP. Influence of hepatitis B immunization to prevent vertical transmission of Hep-B virus in infants born from Hep-B positive mother. Paediatr Indones. 2010;50:321-325. [Cited in This Article: ] |
| 5. | Hasan I. Epidemiology of hepatitis B. Acta Med Indones. 2005;37:231-234. [PubMed] [Cited in This Article: ] |
| 6. | Gunardi H, Zaimi LF, Soedjatmiko AR, Muljono DH. Current prevalence of hepatitis B infection among parturient women in Jakarta, Indonesia. Acta Med Indones. 2014;46:3-9. [PubMed] [Cited in This Article: ] |
| 7. | Norder H, Couroucé AM, Coursaget P, Echevarria JM, Lee SD, Mushahwar IK, Robertson BH, Locarnini S, Magnius LO. Genetic diversity of hepatitis B virus strains derived worldwide: genotypes, subgenotypes, and HBsAg subtypes. Intervirology. 2004;47:289-309. [PubMed] [Cited in This Article: ] |
| 8. | Locarnini S, Littlejohn M, Aziz MN, Yuen L. Possible origins and evolution of the hepatitis B virus (HBV). Semin Cancer Biol. 2013;23:561-575. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 67] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 9. | Siburian MD, Utama A, Dhenni R, Arnelis N, Fanany I, Intan MD, Kurniasih TS, Andriani F, Afadlal S, Julianto EB. High prevalence of hepatitis B virus genotype C/C1 in the Minangkabau ethnic group in Indonesia. Virol J. 2013;10:27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Prasetyo AA, Dirgahayu P, Sari Y, Hudiyono H, Kageyama S. Molecular epidemiology of HIV, HBV, HCV, and HTLV-1/2 in drug abuser inmates in central Javan prisons, Indonesia. J Infect Dev Ctries. 2013;7:453-467. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 51] [Article Influence: 4.6] [Reference Citation Analysis (1)] |
| 11. | Achwan WA, Muttaqin Z, Zakaria E, Depamede SA, Mulyanto S, Tsuda F, Takahashi K, Abe N, Mishiro S. Epidemiology of hepatitis B, C, and E viruses and human immunodeficiency virus infections in Tahuna, Sangihe-Talaud Archipelago, Indonesia. Intervirology. 2007;50:408-411. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Rinonce HT, Yano Y, Utsumi T, Heriyanto DS, Anggorowati N, Widasari DI, Lusida MI, Soetjipto H, Hotta H, Hayashi Y. Hepatitis B and C virus infection among hemodialysis patients in Yogyakarta, Indonesia: Prevalence and molecular evidence for nosocomial transmission. J Med Virol. 2013;85:1348-1361. [PubMed] [Cited in This Article: ] |
| 13. | Amirudin R, Akil H, Akahane Y, Suzuki H. Hepatitis B and C virus infection in Ujung Pandang, Indonesia. Gastroenterol Jpn. 1991;26 Suppl 3:184-188. [PubMed] [Cited in This Article: ] |
| 14. | Akbar N, Basuki B, Mulyanto DH, Sulaiman A, Noer HM. Ethnicity, socioeconomic status, transfusions and risk of hepatitis B and hepatitis C infection. J Gastroenterol Hepatol. 1997;12:752-757. [PubMed] [Cited in This Article: ] |
| 15. | Budihusodo U, Sulaiman HA, Akbar HN, Lesmana LA, Waspodo AS, Noer HM, Akahane Y, Suzuki H. Seroepidemiology of HBV and HCV infection in Jakarta, Indonesia. Gastroenterol Jpn. 1991;26:196-201. [PubMed] [Cited in This Article: ] |
| 16. | Wolff AP, Ruys AH, Dolmans WM, Van Loon AM, Pangalila PF. Hepatitis B virus infection in patients with chronic liver disease and healthy controls in north-Sulawesi, Indonesia. Trop Geogr Med. 1990;42:221-225. [PubMed] [Cited in This Article: ] |
| 17. | Reniers J, Vranckx R, Ngantung W, Sugita E, Meheus A. Prevalence and determinants of hepatitis B virus markers in pregnant women in West Java, Indonesia. J Trop Med Hyg. 1987;90:249-253. [PubMed] [Cited in This Article: ] |
| 18. | Surya IG, Kornia K, Suwardewa TG, Mulyanto F, Mishiro S. Serological markers of hepatitis B, C, and E viruses and human immunodeficiency virus type-1 infections in pregnant women in Bali, Indonesia. J Med Virol. 2005;75:499-503. [PubMed] [Cited in This Article: ] |
| 19. | Creati M, Saleh A, Ruff TA, Stewart T, Otto B, Sutanto A, Clements CJ. Implementing the birth dose of hepatitis B vaccine in rural Indonesia. Vaccine. 2007;25:5985-5993. [PubMed] [Cited in This Article: ] |
| 20. | Utsumi T, Lusida MI, Yano Y, Purwono PB, Amin M, Soetjipto , Hotta H, Hayashi Y. Progress in the Control of Hepatitis B Virus Infection among Children in Indonesia. J Vaccines Vaccin. 2014;5:247. [Cited in This Article: ] |
| 21. | Prasetyo AA, Ariapramuda R, Kindi EA, Dirgahayu P, Sari Y, Dharmawan R, Kageyama S. Men having sex with men in Surakarta, Indonesia: demographics, behavioral characteristics and prevalence of blood borne pathogens. Southeast Asian J Trop Med Public Health. 2014;45:1032-1047. [PubMed] [Cited in This Article: ] |
| 22. | Utsumi T, Yano Y, Lusida MI, Nasronudin M, Juniastuti H, Hayashi Y. Detection of highly prevalent hepatitis B virus co-infection with HIV in Indonesia. Hepatol Res. 2013;43:1032-1039. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Anggorowati N, Yano Y, Heriyanto DS, Rinonce HT, Utsumi T, Mulya DP, Subronto YW, Hayashi Y. Clinical and virological characteristics of hepatitis B or C virus co-infection with HIV in Indonesian patients. J Med Virol. 2012;84:857-865. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Fibriani A, Wisaksana R, Alisjahbana B, Indrati A, Schutten M, van Crevel R, van der Ven A, Boucher CA. Hepatitis B virus prevalence, risk factors and genotype distribution in HIV infected patients from West Java, Indonesia. J Clin Virol. 2014;59:235-241. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Zaw SK, Tun ST, Thida A, Aung TK, Maung W, Shwe M, Aye MM, Clevenbergh P. Prevalence of hepatitis C and B virus among patients infected with HIV: a cross-sectional analysis of a large HIV care programme in Myanmar. Trop Doct. 2013;43:113-115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Kotaki T, Khairunisa SQ, Sukartiningrum SD, Arfijanto MV, Utsumi T, Normalina I, Handajani R, Widiyanti P, Rusli M, Rahayu RP. High prevalence of HIV-1 CRF01_AE viruses among female commercial sex workers residing in Surabaya, Indonesia. PLoS One. 2013;8:e82645. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Agustian D, Yusnita S, Susanto H, Sukandar H, de Schryver A, Meheus A. An estimation of the occupational risk of HBV, HCV and HIV infection among Indonesian health-care workers. Acta Med Indones. 2009;41 Suppl 1:33-37. [PubMed] [Cited in This Article: ] |
| 28. | Utsumi T, Wahyuni RM, Lusida MI, Yano Y, Priambada NP, Amin M, Purwono PB, Istimagfiroh A, Soetjipto A, Hotta H. Full genome characterization and phylogenetic analysis of hepatitis B virus in gibbons and a caretaker in Central Kalimantan, Indonesia. Arch Virol. 2015;160:685-692. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 29. | Hu KQ. Occult hepatitis B virus infection and its clinical implications. J Viral Hepat. 2002;9:243-257. [PubMed] [Cited in This Article: ] |
| 30. | Thedja MD, Roni M, Harahap AR, Siregar NC, Ie SI, Muljono DH. Occult hepatitis B in blood donors in Indonesia: altered antigenicity of the hepatitis B virus surface protein. Hepatol Int. 2010;4:608-614. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 31. | Utsumi T, Yano Y, Lusida MI, Amin M, Soetjipto H, Hayashi Y. Serologic and molecular characteristics of hepatitis B virus among school children in East Java, Indonesia. Am J Trop Med Hyg. 2010;83:189-193. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 32. | Darmawan E, Turyadi KE, Nursanty NK, Thedja MD, Muljono DH. Seroepidemiology and occult hepatitis B virus infection in young adults in Banjarmasin, Indonesia. J Med Virol. 2015;87:199-207. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 33. | Wijaya I, Hasan I. Reactivation of hepatitis B virus associated with chemotherapy and immunosuppressive agent. Acta Med Indones. 2013;45:61-66. [PubMed] [Cited in This Article: ] |
| 34. | Utsumi T, Yano Y, Hotta H. Molecular epidemiology of hepatitis B virus in Asia. World J Med Genet. 2014;4:19-26. [DOI] [Cited in This Article: ] [Cited by in CrossRef: 8] [Cited by in F6Publishing: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 35. | Heriyanto DS, Yano Y, Utsumi T, Anggorowati N, Rinonce HT, Lusida MI, Soetjipto C, Ratnasari N, Maduseno S, Purnama PB. Mutations within enhancer II and BCP regions of hepatitis B virus in relation to advanced liver diseases in patients infected with subgenotype B3 in Indonesia. J Med Virol. 2012;84:44-51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 36. | Lusida MI, Nugrahaputra VE, Soetjipto R, Nagano-Fujii M, Sasayama M, Utsumi T, Hotta H. Novel subgenotypes of hepatitis B virus genotypes C and D in Papua, Indonesia. J Clin Microbiol. 2008;46:2160-2166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 73] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 37. | Mulyanto SN, Surayah K, Tsuda F, Ichiyama K, Takahashi M, Okamoto H. A nationwide molecular epidemiological study on hepatitis B virus in Indonesia: identification of two novel subgenotypes, B8 and C7. Arch Virol. 2009;154:1047-1059. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 38. | Mulyanto SN, Surayah K, Tjahyono AA, Jirintai S, Takahashi M, Okamoto H. Identification and characterization of novel hepatitis B virus subgenotype C10 in Nusa Tenggara, Indonesia. Arch Virol. 2010;155:705-715. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 39. | Mulyanto SN, Wahyono A, Jirintai S, Takahashi M, Okamoto H. Analysis of the full-length genomes of novel hepatitis B virus subgenotypes C11 and C12 in Papua, Indonesia. J Med Virol. 2011;83:54-64. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 40. | Utsumi T, Nugrahaputra VE, Amin M, Hayashi Y, Hotta H, Lusida MI. Another novel subgenotype of hepatitis B virus genotype C from papuans of Highland origin. J Med Virol. 2011;83:225-234. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 41. | Mulyanto P, Depamede SN, Wahyono A, Jirintai S, Nagashima S, Takahashi M, Nishizawa T, Okamoto H. Identification of four novel subgenotypes (C13-C16) and two inter-genotypic recombinants (C12/G and C13/B3) of hepatitis B virus in Papua province, Indonesia. Virus Res. 2012;163:129-140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 42. | Utsumi T, Lusida MI, Yano Y, Nugrahaputra VE, Amin M, Juniastuti Y, Hotta H. Complete genome sequence and phylogenetic relatedness of hepatitis B virus isolates in Papua, Indonesia. J Clin Microbiol. 2009;47:1842-1847. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 43. | Tatematsu K, Tanaka Y, Kurbanov F, Sugauchi F, Mano S, Maeshiro T, Nakayoshi T, Wakuta M, Miyakawa Y, Mizokami M. A genetic variant of hepatitis B virus divergent from known human and ape genotypes isolated from a Japanese patient and provisionally assigned to new genotype J. J Virol. 2009;83:10538-10547. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 290] [Cited by in F6Publishing: 317] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 44. | Ruff TA, Gertig DM, Otto BF, Gust ID, Sutanto A, Soewarso TI, Kandun N, Marschner IC, Maynard JE. Lombok Hepatitis B Model Immunization Project: toward universal infant hepatitis B immunization in Indonesia. J Infect Dis. 1995;171:290-296. [PubMed] [Cited in This Article: ] |
| 45. | Lee CM, Chen CH, Lu SN, Tung HD, Chou WJ, Wang JH, Chen TM, Hung CH, Huang CC, Chen WJ. Prevalence and clinical implications of hepatitis B virus genotypes in southern Taiwan. Scand J Gastroenterol. 2003;38:95-101. [PubMed] [Cited in This Article: ] |
| 46. | Orito E, Mizokami M, Sakugawa H, Michitaka K, Ishikawa K, Ichida T, Okanoue T, Yotsuyanagi H, Iino S. A case-control study for clinical and molecular biological differences between hepatitis B viruses of genotypes B and C. Japan HBV Genotype Research Group. Hepatology. 2001;33:218-223. [PubMed] [Cited in This Article: ] |
| 47. | Zhang AM, Wang HF, Wang HB, Hu JH, He WP, Su HB, Chen J, Du N, Duan XZ. [Association between HBV genotype and chronic/severe liver disease with HBV infection in Chinese patients]. Zhonghua Shiyan He Linchuang Bingduxue Zazhi. 2010;24:178-180. [PubMed] [Cited in This Article: ] |
| 48. | Utama A, Purwantomo S, Siburian MD, Dhenni R, Gani RA, Hasan I, Sanityoso A, Miskad UA, Akil F, Yusuf I. Hepatitis B virus subgenotypes and basal core promoter mutations in Indonesia. World J Gastroenterol. 2009;15:4028-4036. [PubMed] [Cited in This Article: ] |
| 49. | Petta S, Cammà C, Di Marco V, Macaluso FS, Maida M, Pizzolanti G, Belmonte B, Cabibi D, Di Stefano R, Ferraro D. Hepatic steatosis and insulin resistance are associated with severe fibrosis in patients with chronic hepatitis caused by HBV or HCV infection. Liver Int. 2011;31:507-515. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 50. | Koike K. Steatosis, liver injury, and hepatocarcinogenesis in hepatitis C viral infection. J Gastroenterol. 2009;44 Suppl 19:82-88. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 51. | Takuma Y, Nouso K, Makino Y, Saito S, Takayama H, Takahara M, Takahashi H, Murakami I, Takeuchi H. Hepatic steatosis correlates with the postoperative recurrence of hepatitis C virus-associated hepatocellular carcinoma. Liver Int. 2007;27:620-626. [PubMed] [Cited in This Article: ] |
| 52. | Machado MV, Oliveira AG, Cortez-Pinto H. Hepatic steatosis in hepatitis B virus infected patients: meta-analysis of risk factors and comparison with hepatitis C infected patients. J Gastroenterol Hepatol. 2011;26:1361-1367. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 53. | Lin CL, Kao JH. The clinical implications of hepatitis B virus genotype: Recent advances. J Gastroenterol Hepatol. 2011;26 Suppl 1:123-130. [PubMed] [Cited in This Article: ] |
| 54. | Lesmana LA, Lesmana CR, Pakasi LS, Krisnuhoni E. Prevalence of hepatic steatosis in chronic hepatitis B patients and its association with disease severity. Acta Med Indones. 2012;44:35-39. [PubMed] [Cited in This Article: ] |
| 55. | Roemling C, Qaim M. Obesity trends and determinants in Indonesia. Appetite. 2012;58:1005-1013. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 56. | Sulaiman A, Lesmana LA. An observational study to evaluate the safety and efficacy of telbivudine in adults with chronic hepatitis B. Acta Med Indones. 2014;46:38-43. [PubMed] [Cited in This Article: ] |
| 57. | Wahidin M, Noviani R, Hermawan S, Andriani V, Ardian A, Djarir H. Population-based cancer registration in Indonesia. Asian Pac J Cancer Prev. 2012;13:1709-1710. [PubMed] [Cited in This Article: ] |
| 58. | Sulaiman HA. Hepatitis B virus infection in liver cirrhosis and hepatocellular carcinoma in Jakarta Indonesia. Gastroenterol Jpn. 1989;24:434-441. [PubMed] [Cited in This Article: ] |
| 59. | Marwoto W, Diana S, Roostini ES. Epidemiology of liver cancer in Indonesia. Southeast Asian J Trop Med Public Health. 1985;16:607-608. [PubMed] [Cited in This Article: ] |
| 60. | Wang BE, Ma WM, Sulaiman A, Noer S, Sumoharjo S, Sumarsidi D, Tandon BN, Nakao K, Mishiro S, Miyakawa Y. Demographic, clinical, and virological characteristics of hepatocellular carcinoma in Asia: survey of 414 patients from four countries. J Med Virol. 2002;67:394-400. [PubMed] [Cited in This Article: ] |
| 61. | Qu LS, Liu JX, Liu TT, Shen XZ, Chen TY, Ni ZP, Lu CH. Association of hepatitis B virus pre-S deletions with the development of hepatocellular carcinoma in Qidong, China. PLoS One. 2014;9:e98257. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 62. | Liao Y, Hu X, Chen J, Cai B, Tang J, Ying B, Wang H, Wang L. Precore mutation of hepatitis B virus may contribute to hepatocellular carcinoma risk: evidence from an updated meta-analysis. PLoS One. 2012;7:e38394. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 63. | Utama A, Siburian MD, Fanany I, Intan MD, Dhenni R, Kurniasih TS, Lelosutan SA, Achwan WA, Zubir N, Arnelis B. Hepatitis B virus pre-S2 start codon mutations in Indonesian liver disease patients. World J Gastroenterol. 2012;18:5418-5426. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 64. | Liu S, Zhang H, Gu C, Yin J, He Y, Xie J, Cao G. Associations between hepatitis B virus mutations and the risk of hepatocellular carcinoma: a meta-analysis. J Natl Cancer Inst. 2009;101:1066-1082. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 279] [Cited by in F6Publishing: 314] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 65. | Kamatani Y, Wattanapokayakit S, Ochi H, Kawaguchi T, Takahashi A, Hosono N, Kubo M, Tsunoda T, Kamatani N, Kumada H. A genome-wide association study identifies variants in the HLA-DP locus associated with chronic hepatitis B in Asians. Nat Genet. 2009;41:591-595. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 396] [Cited by in F6Publishing: 403] [Article Influence: 26.9] [Reference Citation Analysis (0)] |
| 66. | Guo X, Zhang Y, Li J, Ma J, Wei Z, Tan W, O’Brien SJ. Strong influence of human leukocyte antigen (HLA)-DP gene variants on development of persistent chronic hepatitis B virus carriers in the Han Chinese population. Hepatology. 2011;53:422-428. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 114] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 67. | Hu L, Zhai X, Liu J, Chu M, Pan S, Jiang J, Zhang Y, Wang H, Chen J, Shen H. Genetic variants in human leukocyte antigen/DP-DQ influence both hepatitis B virus clearance and hepatocellular carcinoma development. Hepatology. 2012;55:1426-1431. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 127] [Cited by in F6Publishing: 139] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 68. | Png E, Thalamuthu A, Ong RT, Snippe H, Boland GJ, Seielstad M. A genome-wide association study of hepatitis B vaccine response in an Indonesian population reveals multiple independent risk variants in the HLA region. Hum Mol Genet. 2011;20:3893-3898. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 88] [Article Influence: 6.8] [Reference Citation Analysis (0)] |