Published online Dec 14, 2015. doi: 10.3748/wjg.v21.i46.13080
Peer-review started: July 20, 2015
First decision: August 26, 2015
Revised: September 7, 2015
Accepted: November 9, 2015
Article in press: November 9, 2015
Published online: December 14, 2015
AIM: To describe the ages at diagnosis and operation of biliary atresia (BA) and its incidence over a 15-year period in Taiwan.
METHODS: This was a population-based cohort study. BA cases were identified from the Taiwan National Health Insurance Research Database based on the International Classification of Diseases, Ninth Revision (ICD-9) code of BA 751.61 plus Kasai operation (ICD-9 procedure code 51.37) or liver transplantation (LT, ICD-9 procedure code 50.5). The patients’ characteristics including sex, age at diagnosis, age at receiving Kasai operation and age at receiving LT were compared among three birth cohorts: (1) 1997 to 2001; (2) 2002 to 2006; and (3) 2007 to 2011.
RESULTS: There were a total of 540 BA cases (275 females) with an incidence of 1.62 per 10000 live births. No seasonality of BA was noted. The mean ages at diagnosis of three cohorts were 57.9, 55.6 and 52.6 d. A linear regression model demonstrated a decreasing trend of the mean age at diagnosis (1.27 d per year). The proportion of BA cases that received the Kasai operation within 60 d of age increased from 76% to 81%. A total of 189 (35%) BA patients underwent LT. The mean age at LT was reduced from 3-year-old to 1-year-old. The rates of LT were 25.6% and 32.3% in patients who received the Kasai operation within 60 d or after 60 d of age, respectively. All patients who did not undergo a Kasai operation eventually required LT.
CONCLUSION: The ages at diagnosis and operation in BA cases have decreased over time. Kasai operation performed at younger age reduces the need for LT. The incidence of BA in Taiwan fluctuates, but without certain trend.
Core tip: Biliary atresia (BA) is an important liver disease of children. The age of diagnosis and operation for BA greatly affects its outcome. The incidence of BA varies among different studies and long-term trends are controversial. This study found the long-term incidence of BA in Taiwan has no increasing or decreasing trend. The age at diagnosis and operation of BA is continuously decreasing. The mean age at liver transplantation was reduced from 3-year-old to 1-year-old during the 15-year study period.
- Citation: Lin JS, Chen SCC, Lu CL, Lee HC, Yeung CY, Chan WT. Reduction of the ages at diagnosis and operation of biliary atresia in Taiwan: A 15-year population-based cohort study. World J Gastroenterol 2015; 21(46): 13080-13086
- URL: https://www.wjgnet.com/1007-9327/full/v21/i46/13080.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i46.13080
Biliary atresia (BA) is the leading cause of liver-related deaths and the most frequent reason for liver transplantation (LT) in children. Its outcome highly relates to the timing of diagnosis and surgical treatment[1-4]. The Kasai operation (hepatoportoenterostomy) as the primary surgical treatment for BA cases is recommended to be performed as early as possible[1,2,5,6], because increased age at the time of surgery may result in a deleterious effect on the outcomes of BA cases[2,4,7]. Usually, delayed identification of pale stools and delayed visits to a physician are the major causes of a delayed Kasai operation.
In 2004, Taiwan began a national screening program using an infant stool color card (SCC) to early detect BA case[8,9]. This program has been approved to be a very sensitive and specific screening method for BA in infants[9,10]. It can enhance earlier referral, which may lead to timely performance of the Kasai operation and better postoperative outcome in infants with BA[10-12]. One study found a significant decrease in the age at diagnosis and Kasai operation of BA cases following the implementation of this screening program[13]. However, this study just observed the BA cases until 2008, four years after the screening program. Whether the decreasing trend of the ages at diagnosis and Kasai operation after 2008 is continued is not clear.
In addition, we would like to update the incidences of BA and check its trend in Taiwan over a longer period from 1997 to 2011. The incidence of BA varies worldwide and tends to be higher in Asian countries than in Europe and North America[14]. It ranges 0.51-0.73 per 10000 in western countries[7,15,16], 1.04-1.10 per 10000 in Japan[17,18] and 1.46-1.85 per 10000 in Taiwan[10,19,20]. Two studies from Taiwan have reported contradicting trends[19,20]. Tiao et al[19] observed an increase in the incidence of BA in Taiwan from 1996 to 2003, but Lin et al[20] found a decrease in the BA incidence in Taiwan from 2004 to 2009. One possible explanation for the different conclusions is the different observation periods. Moreover, these observation periods may be too short to make any definitive conclusion regarding long-term trends. Therefore, the objectives of this study are to describe the ages of BA cases at their diagnosis and operation and to update their incidences from 1997 until 2011.
Taiwan’s National Health Insurance program is a government-managed, compulsory health insurance that covers more than 99% of the country’s total population. The National Health Insurance Research Database (NHIRD) is a research database that stores the claims data of the National Health Insurance; it comprises both inpatient and outpatient medical records and may be released to scientists in Taiwan for research purposes. The identification numbers of beneficiaries and institutions in the NHIRD have been scrambled prior to the release of data to protect the confidentiality of individuals. The Institutional Review Board of Ditmanson Medical Foundation Chia-Yi Christian Hospital has approved this study and waived the requirement for written informed consent from the patients as this study is a secondary data analysis (CYCH-IRB No. 102023).
We retrieved all inpatient records in the NHIRD from 1997 to 2011 to estimate the annual number of newly diagnosed BA. Following the criteria of previous studies (also based on the NHIRD)[13,19], BA cases were identified if they had been given a diagnosis code of BA [International Classification of Diseases, Ninth Revision (ICD-9) diagnosis code 751.61] and had received a Kasai operation (ICD-9 procedure code 51.37) or LT (ICD-9 procedure code 50.5) during the study period. The patients’ demographic and clinical characteristics, including sex, date of birth, first date of admission at which BA was suspected, records of LT, and age at Kasai operation were recorded by longitudinal linkage of the inpatient records in the NHIRD via an encrypted personal identification number.
The annual incidence rate was calculated by the number of cases of newly diagnosed BA divided by the number of newborns per year. The temporal trend of incidences was examined by testing the regression coefficient of the calendar year via Poisson regression. The patients’ characteristics, including sex, age at first admission for BA, age at receiving a Kasai operation and age at receiving LT were compared among three birth cohorts: (1) 1997 to 2001; (2) 2002 to 2006; and (3) 2007 to 2011. A linear regression model was performed to compare the calendar year with the age at receiving a Kasai operation and the first date of admission in which BA was suspected. The Cochrane-armitage trend test was performed to examine the temporal trend of the percentage of patients who received a Kasai operation before 60 d of age and the percentage of patients who received LT. Statistical analyses in this study were performed using SAS analytical software (version 9.3, SAS Institute Inc., Cary, NC, United States). A P value < 0.05 was considered to be statistically significant.
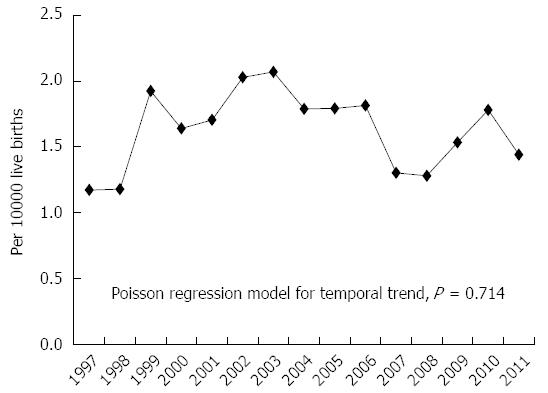
There were a total of 540 BA cases (265 males and 275 females) who received the Kasai operation or LT from 1997 to 2011. The number of newly diagnosed cases per year varied between 24 and 52, with a mean caseload of 36 new BA patients per year. The annual incidence of BA varied from 1.17 to 2.07 per 10000 live births, with an overall incidence of 1.62 per 10000 live births (Figure 1). A temporal trend of incidences from 1997 to 2011 was not observed via the Poisson regression model (Figure 1, P = 0.714).
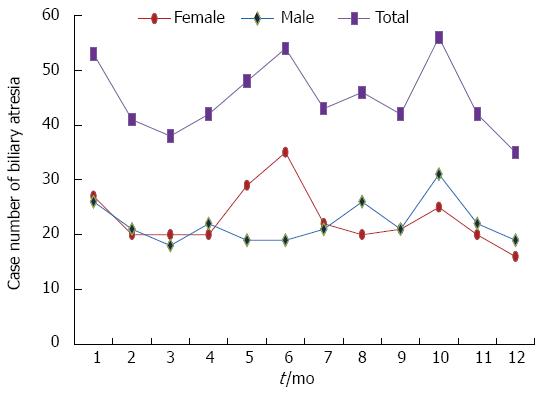
As shown in Figure 2, female BA cases had higher incidences in the months of May and June but male cases were homogenously distributed in all months. The months with the highest total number of BA births were January, June and October. However, there was no obvious seasonal distribution of the BA cases (Figure 2).
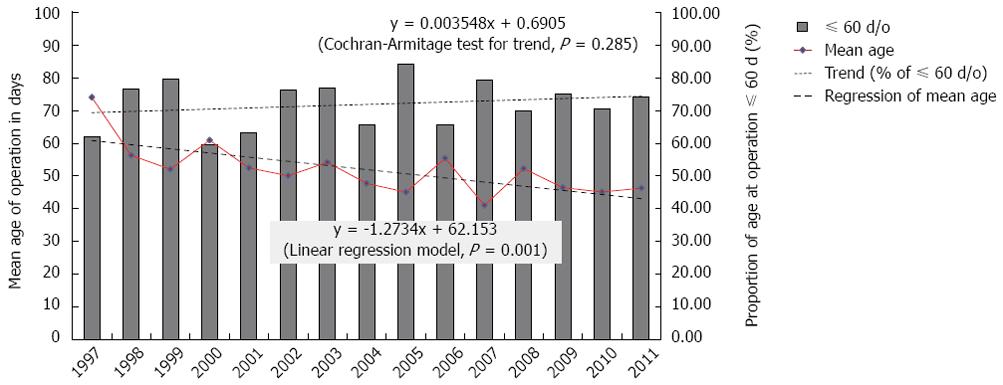
The mean age at the first admission for suspected BA decreased from 57.9 d in the first cohort to 52.6 d in the third cohort, with a significant trend (P = 0.035, Table 1). The SD of the ages at the first diagnosis was also gradually reduced (Table 1); this indicated less variation in the ages at diagnosis. Similarly, the means and SD of the ages of BA cases that underwent the Kasai operation were also significantly reduced from the first cohort to the third cohort (P < 0.05, Table 1). Meanwhile, the linear regression model for the mean age at operation demonstrated a significantly decreasing trend (Figure 3). Consequently, the average proportion of BA cases less than 60 d of age that received the Kasai operation increased from 76.6% to 81.1% over the studied period (Table 1); however, these changes were not statistically significant (P = 0.285 in Figure 3). In contrast, the mean age at LT was reduced from nearly three years old to less than one year old; the SD of the ages at LT was also greatly reduced (Table 1).
| 1997-2001 | 2002-2006 | 2007-2011 | P value | |
| Case number | 208 | 200 | 132 | |
| Male | 97 (46.6) | 101 (50.5) | 67 (50.8) | 0.421 |
| Incidence (per 10000 person-years) | 6.68 | 8.31 | 6.73 | 0.6992 |
| Age at diagnosis (d), mean ± SD | 57.9 ± 70.0 | 55.6 ± 55.4 | 52.6 ± 36.4 | 0.0353 |
| Age at Kasai operation (d), mean ± SD | 58.2 ± 42.0 | 50.5 ± 30.8 | 46.0 ± 23.8 | 0.0063 |
| Age at Liver transplant (d), mean ± SD | 958 ± 859 | 617 ± 638 | 353 ± 237 | 0.0063 |
| Kasai operation | 188 (90.4) | 174 (87.0) | 122 (92.4) | 0.702 |
| Kasai operation ≤ 60 d 1 | 144 (76.6) | 154 (88.5) | 99 (81.1) | 0.285 |
| Liver transplant | 68 (32.7) | 82 (41.0) | 39 (29.6) | 0.7824 |
There were a total of 189 (35%) BA patients had undergone LT during the study period. All BA patients who did not receive the Kasai operation ultimately needed LT (Table 2). The rates of LT were 25.6% among those patients who received the Kasai operation within 60 d of age and 32.3% among those who received the operation over 60 d of age (P = 0.133, Table 2).
This study was a 15-year population-based epidemiological analysis of BA. The overall incidence of BA in Taiwan was 1.62 (range, 1.17 to 2.07) per 10000 live births; this incidence is higher than that of western countries and Japan[7,15-18]. A systematic review has suggested that ethnicity may play some role in the occurrence of BA[21]. As shown in Figure 1, the incidence of BA increased from 1.17 per 10000 live births in 1997 to the highest rate of 2.07 per 10000 live births in 2003; this incidence then declined to an ultimate low of 1.28 per 10000 live births in 2008. These observations explain why Tiao et al[19] reported an increasing trend in the incidence of BA from 1996 to 2003, but Lin et al[20] observed a decreasing trend from 2004 to 2009. However, the incidence of BA returned to 1.53 per 10000 live births in 2009, 1.78 per 10000 live births in 2010, and 1.44 per 10000 live births in 2011. Thus, we may conclude that although there have been fluctuations in the incidence of BA, there is no significant trend in the long-term incidence in Taiwan.
Lin et al[20] said the decrease of BA incidence in Taiwan during 2004-2009 may be related to improvements of the general socioeconomic status and the popularity of rotavirus vaccination. However, as mentioned above, this present study found the decrease of BA incidence was not continued after 2010, though the general socioeconomic status and the coverage of rotavirus vaccination in Taiwan did not decline at that time. Moreover, as the recommended schedule for rotavirus vaccines is during the ages of 2 to 6 mo[22], it would be strange to expect the rotavirus vaccine to prevent the occurrence of BA which is usually diagnosed by the age of 2 mo. Therefore, we think the previous assumption about the association between rotavirus vaccination and BA incidence needs to be further examined.
Tseng et al[13] found that the median age at first admission for BA cases decreased from 47 d of age before implementing the SCC program to 43 d of age in the era of the SCC program. However, as shown in Figure 3, we found the reducing trend of the age at diagnosis has been started before 2004, when the national SCC screening was begun. The linear regression model demonstrated a decreasing trend in the age at diagnosis (1.27 d per year) (Figure 3). The age at diagnosis of the late cohort was averagely advanced 2-3 d earlier than that of the early cohort (Table 1). Therefore, this decrease in ages at BA diagnosis and subsequent operation was not entirely due to the SCC screening program alone. Other factors such as medical resource availability and better accessibility to surgical interventions may also have contributed to these changes. Regardless, we agree that SCC screening has the potential benefit of increasing BA awareness in both parents and physicians. Therefore, we would continue to recommend the widespread use of SCC screening. Notably, several countries have already implemented SCC as their national screening program[11,23,24].
As the observed decreasing trend in the age at diagnosis of BA continues, more BA cases can be treated in a timely manner. As shown in the Figure 3, the proportions of Kasai operations within 60 d of age increased from 60% in 1997 to 75% in 2011. One study in France estimated that 5.7% of all LTs might be avoided if all BA patients received a Kasai operation before 46 d of age[4]. Our data also found that the rate of LT was much less in BA patients who received a Kasai operation within 60 d of age than in those who received the operation at over 60 d of age (Table 2). We believe the need for LT can further be reduced if the average age at Kasai operation is reduced to 50 or even 45 d of age in the future.
One astonishing finding in this study is the decrease in the age at LT. The age at LT decreased from almost three years of age in the first cohort to one year of age in the third cohort (Table 1). Historically, the efficacy of LT and postoperative management of these patients have been limited; the donor pool for LT was also limited[25]. Therefore, the timing of LT was delayed. Over time, however, LT has become much more effective with an increase in satisfactory results[26-28]. In addition, the use of living-related donors has become more acceptable and there has been an overall increase in the general population’s attitude toward organ donation. Physicians therefore may perform an LT at an earlier stage in patients with potential hepatic failure before many complications occur. These factors help decrease the age at LT.
The seasonality of BA occurrence was controversial in the literature[14,15,17,29-32]. One review paper said the BA cases occurred mainly during the months of August to March[14]. Nakamizo et al[32] observed that the incidence of BA had a negative correlation with the average temperature of each month and found a higher incidence of BA during December to March in Japan. However, other studies did not find the seasonality of BA occurrence[15,17,29-31]. Our study did not show certain seasonal distribution of BA occurrence in Taiwan either, though May and June had more female cases (Figure 2).
In conclusion, The ages at diagnosis, Kasai operation and LT in BA cases have decreased over time. The need for LT in BA cases may be reduced if patients receive the Kasai operation as early as possible. The incidence of BA in Taiwan has fluctuated, and has no overall increasing or decreasing trend. No seasonality of BA was found in Taiwan.
This study was based in part on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health and Welfare and managed by National Health Research Institutes. The interpretations and conclusions mentioned in this report do not represent those of the Bureau of National Health Insurance, Department of Health and Welfare or National Health Research Institutes.
Biliary atresia (BA) is the leading cause of liver-related deaths and the most frequent reason for liver transplantation in children. Its outcome highly relates to the timing of diagnosis and Kasai operation.
To describe the ages at diagnosis and Kasai operation of BA cases and its incidence over a 15-year period in Taiwan, from 1997 to 2011.
The incidence of BA was 1.62 per 10000 live births. The ages at diagnosis and operation in BA cases have decreased over time. The mean age at liver transplant was reduced from 3 years-old to 1 year-old. The rates of LT were 25.6% and 32.3% in patients who received the Kasai operation within 60 d or after 60 d of age, respectively.
To advance the time of diagnosis and operation of BA cases can improve the outcome and reduce the need of liver transplant.
This is an interesting manuscript describing the decrease in time to kasai procedure for children with biliary atresia in Taiwan by the use of stool color cards to recognize the need for evaluation timely. Also, the study is well-designed, well-written and data are clearly presented. So it’s a nice epidemiologic manuscript that deserves to be highly cited.
P- Reviewer: Choe BH, Philip R, Sira MM, Wang GY S- Editor: Gong ZM L- Editor: A E- Editor: Zhang DN
| 1. | Chardot C, Carton M, Spire-Bendelac N, Le Pommelet C, Golmard JL, Auvert B. Prognosis of biliary atresia in the era of liver transplantation: French national study from 1986 to 1996. Hepatology. 1999;30:606-611. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 181] [Cited by in F6Publishing: 187] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 2. | Wildhaber BE, Coran AG, Drongowski RA, Hirschl RB, Geiger JD, Lelli JL, Teitelbaum DH. The Kasai portoenterostomy for biliary atresia: A review of a 27-year experience with 81 patients. J Pediatr Surg. 2003;38:1480-1485. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 91] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 3. | Hartley JL, Davenport M, Kelly DA. Biliary atresia. Lancet. 2009;374:1704-1713. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 608] [Cited by in F6Publishing: 569] [Article Influence: 37.9] [Reference Citation Analysis (0)] |
| 4. | Serinet MO, Wildhaber BE, Broué P, Lachaux A, Sarles J, Jacquemin E, Gauthier F, Chardot C. Impact of age at Kasai operation on its results in late childhood and adolescence: a rational basis for biliary atresia screening. Pediatrics. 2009;123:1280-1286. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 275] [Cited by in F6Publishing: 248] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 5. | Serinet MO, Broué P, Jacquemin E, Lachaux A, Sarles J, Gottrand F, Gauthier F, Chardot C. Management of patients with biliary atresia in France: results of a decentralized policy 1986-2002. Hepatology. 2006;44:75-84. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 117] [Cited by in F6Publishing: 109] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 6. | Lai HS, Chen WJ, Chen CC, Hung WT, Chang MH. Long-term prognosis and factors affecting biliary atresia from experience over a 25 year period. Chang Gung Med J. 2006;29:234-239. [PubMed] [Cited in This Article: ] |
| 7. | Chardot C, Buet C, Serinet MO, Golmard JL, Lachaux A, Roquelaure B, Gottrand F, Broué P, Dabadie A, Gauthier F. Improving outcomes of biliary atresia: French national series 1986-2009. J Hepatol. 2013;58:1209-1217. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 147] [Cited by in F6Publishing: 151] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 8. | Chen SM, Chang MH, Du JC, Lin CC, Chen AC, Lee HC, Lau BH, Yang YJ, Wu TC, Chu CH. Screening for biliary atresia by infant stool color card in Taiwan. Pediatrics. 2006;117:1147-1154. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 108] [Cited by in F6Publishing: 112] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 9. | Chang MH. Screening for biliary atresia. Chang Gung Med J. 2006;29:231-233. [PubMed] [Cited in This Article: ] |
| 10. | Hsiao CH, Chang MH, Chen HL, Lee HC, Wu TC, Lin CC, Yang YJ, Chen AC, Tiao MM, Lau BH. Universal screening for biliary atresia using an infant stool color card in Taiwan. Hepatology. 2008;47:1233-1240. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 201] [Cited by in F6Publishing: 202] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 11. | Santos JL, Carvalho E, Bezerra JA. Advances in biliary atresia: from patient care to research. Braz J Med Biol Res. 2010;43:522-527. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Lien TH, Chang MH, Wu JF, Chen HL, Lee HC, Chen AC, Tiao MM, Wu TC, Yang YJ, Lin CC. Effects of the infant stool color card screening program on 5-year outcome of biliary atresia in Taiwan. Hepatology. 2011;53:202-208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 125] [Cited by in F6Publishing: 127] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 13. | Tseng JJ, Lai MS, Lin MC, Fu YC. Stool color card screening for biliary atresia. Pediatrics. 2011;128:e1209-e1215. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 14. | Jimenez-Rivera C, Jolin-Dahel KS, Fortinsky KJ, Gozdyra P, Benchimol EI. International incidence and outcomes of biliary atresia. J Pediatr Gastroenterol Nutr. 2013;56:344-354. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 102] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 15. | Chardot C, Carton M, Spire-Bendelac N, Le Pommelet C, Golmard JL, Auvert B. Epidemiology of biliary atresia in France: a national study 1986-96. J Hepatol. 1999;31:1006-1013. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 153] [Cited by in F6Publishing: 118] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 16. | Yoon PW, Bresee JS, Olney RS, James LM, Khoury MJ. Epidemiology of biliary atresia: a population-based study. Pediatrics. 1997;99:376-382. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 177] [Cited by in F6Publishing: 141] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 17. | Wada H, Muraji T, Yokoi A, Okamoto T, Sato S, Takamizawa S, Tsugawa J, Nishijima E. Insignificant seasonal and geographical variation in incidence of biliary atresia in Japan: a regional survey of over 20 years. J Pediatr Surg. 2007;42:2090-2092. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 60] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 18. | Nio M, Ohi R, Miyano T, Saeki M, Shiraki K, Tanaka K. Five- and 10-year survival rates after surgery for biliary atresia: a report from the Japanese Biliary Atresia Registry. J Pediatr Surg. 2003;38:997-1000. [PubMed] [Cited in This Article: ] |
| 19. | Tiao MM, Tsai SS, Kuo HW, Chen CL, Yang CY. Epidemiological features of biliary atresia in Taiwan, a national study 1996-2003. J Gastroenterol Hepatol. 2008;23:62-66. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Lin YC, Chang MH, Liao SF, Wu JF, Ni YH, Tiao MM, Lai MW, Lee HC, Lin CC, Wu TC. Decreasing rate of biliary atresia in Taiwan: a survey, 2004-2009. Pediatrics. 2011;128:e530-e536. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 21. | Girard M, Jannot AS, Besnard M, Jacquemin E, Henrion-Caude A. Biliary atresia: does ethnicity matter? J Hepatol. 2012;57:700-701; author reply 702. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Krishnarajah G, Davis EJ, Fan Y, Standaert BA, Buikema AR. Rotavirus vaccine series completion and adherence to vaccination schedules among infants in managed care in the United States. Vaccine. 2012;30:3717-3722. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Schreiber RA, Masucci L, Kaczorowski J, Collet JP, Lutley P, Espinosa V, Bryan S. Home-based screening for biliary atresia using infant stool colour cards: a large-scale prospective cohort study and cost-effectiveness analysis. J Med Screen. 2014;21:126-132. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 24. | Wildhaber BE. Screening for biliary atresia: Swiss stool color card. Hepatology. 2011;54:367-368; author reply 369. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 25. | Hung PY, Chen CC, Chen WJ, Lai HS, Hsu WM, Lee PH, Ho MC, Chen TH, Ni YH, Chen HL. Long-term prognosis of patients with biliary atresia: a 25 year summary. J Pediatr Gastroenterol Nutr. 2006;42:190-195. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 103] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 26. | Chen CL, Concejero A, Wang CC, Wang SH, Lin CC, Liu YW, Yong CC, Yang CH, Lin TS, Chiang YC. Living donor liver transplantation for biliary atresia: a single-center experience with first 100 cases. Am J Transplant. 2006;6:2672-2679. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 92] [Cited by in F6Publishing: 92] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 27. | Wang SH, Chen CL, Concejero A, Wang CC, Lin CC, Liu YW, Yang CH, Yong CC, Lin TS, Chiang YC. Living donor liver transplantation for biliary atresia. Chang Gung Med J. 2007;30:103-108. [PubMed] [Cited in This Article: ] |
| 28. | Tiao MM, Chuang JH, Huang LT, Hsieh CS, Lee SY, Liang CD, Chen CL. Management of biliary atresia: experience in a single institute. Chang Gung Med J. 2007;30:122-127. [PubMed] [Cited in This Article: ] |
| 29. | Livesey E, Cortina Borja M, Sharif K, Alizai N, McClean P, Kelly D, Hadzic N, Davenport M. Epidemiology of biliary atresia in England and Wales (1999-2006). Arch Dis Child Fetal Neonatal Ed. 2009;94:F451-F455. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 92] [Cited by in F6Publishing: 93] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 30. | Fischler B, Haglund B, Hjern A. A population-based study on the incidence and possible pre- and perinatal etiologic risk factors of biliary atresia. J Pediatr. 2002;141:217-222. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 94] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 31. | Ayas MF, Hillemeier AC, Olson AD. Lack of evidence for seasonal variation in extrahepatic biliary atresia during infancy. J Clin Gastroenterol. 1996;22:292-294. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 32. | Nakamizo M, Toyabe S, Kubota M, Komata O, Suzuki H, Akazawa K. Seasonality in the incidence of biliary atresia in Japan. Acta Paediatr. 2006;95:509-510. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |