Published online Dec 14, 2017. doi: 10.3748/wjg.v23.i46.8256
Peer-review started: June 28, 2017
First decision: July 13, 2017
Revised: August 23, 2017
Accepted: September 13, 2017
Article in press: September 13, 2017
Published online: December 14, 2017
A 47-year-old woman presented to our hospital with complaints of dysphagia. Esophagogastroduodenoscopy identified a submucosal tumor in the left wall of the esophagus that was diagnosed as a benign schwannoma on biopsy. Computed tomography revealed a tumor of length 60 mm in the thoracic esophagus, with its cranial edge at the level of the aortic arch. On endoscopy, a submucosal tunnel was created 40 mm proximal to the cranial edge of the tumor, and its oral end was dissected from the mucosal and muscular layers. This was followed by the resection of the entire tumor by left-sided thoracoscopy. The esophageal defect was closed in layer by continuous suture from the thoracic side. Endoscopic closure was achieved by using clips. No postoperative complications were observed. Oral diet was resumed from postoperative day 7 and the patient was discharged on postoperative day 9. This combined approach has not been described for similar tumors. Our experience demonstrated that large esophageal tumors can be safely excised with minimally invasive surgery by using a combination of thoracoscopy and endoscopy.
Core tip: A 47-year-old woman was diagnosed with a benign schwannoma of length 60 mm in the thoracic esophagus. On endoscopy, a submucosal tunnel was created 40 mm proximal to the cranial edge of the tumor, and its only oral end was dissected from the mucosal and muscular layers. This was followed by the resection of the entire tumor by left-sided thoracoscopic procedure. Endoscopic closure was achieved by using clips. No postoperative complications were observed. Our experience demonstrated that large esophageal tumors can be safely excised with minimally invasive surgery by using a combination of thoracoscopy and endoscopy.
- Citation: Onodera Y, Nakano T, Takeyama D, Maruyama S, Taniyama Y, Sakurai T, Heishi T, Sato C, Kumagai T, Kamei T. Combined thoracoscopic and endoscopic surgery for a large esophageal schwannoma. World J Gastroenterol 2017; 23(46): 8256-8260
- URL: https://www.wjgnet.com/1007-9327/full/v23/i46/8256.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i46.8256
Esophageal schwannoma is a relatively rare benign esophageal submucosal tumor (SMT). Enucleation is the treatment of choice, and minimally invasive surgery using thoracoscopy has been the usual approach[1-4]. The left thoracic approach, although considered better for tumors involving the left esophageal wall, is limited by the presence of the aortic arch and the trachea. In addition, the choice between thoracoscopy or thoracotomy is made depending on the size and/or location of the tumor[1,5,6]. Submucosal endoscopic tumor resection (SET) for esophageal SMT, was recently reported by Inoue et al[7], using the technique of submucosal tunnel described for per-oral endoscopic myotomy (POEM) for esophageal achalasia[8]. Laparoscopic and endoscopic cooperative surgery (LECS) has been performed for gastric SMT or duodenal tumor recently[9-12], while the treatment method combined thoracoscopy and endoscopy has not been established in esophageal SMT. In the present case report, we describe a combined technique of submucosal endoscopic resection and thoracoscopic surgery in successfully resecting a large benign schwannoma.
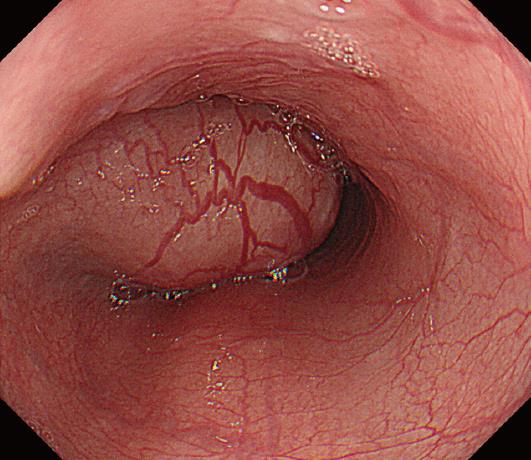
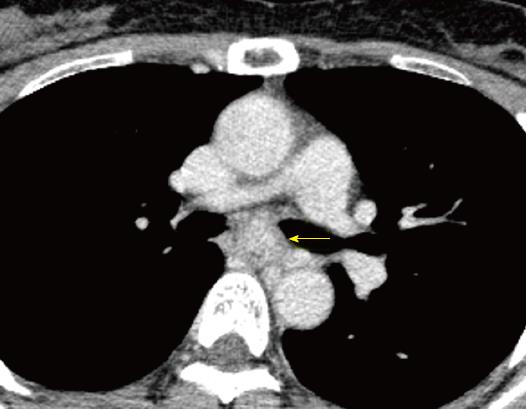
A 47-year-old woman presented to the Tohoku University Hospital with complaints of dysphagia. Esophagogastroduodenoscopy identified a smooth elevated lesion located about 27-33 cm from her incisors (Figure 1). Endoscopic ultrasonography (EUS) demonstrated a large tumor mass in the esophageal wall that was hypoechoic and appeared to originate from either the submucosal or the muscular layer. Enhanced computed tomography (CT) confirmed this to be a 60-mm-long tumor, with its cranial edge identified at the level of the aortic arch (Figure 2). Ultrasound-guided fine-needle aspiration biopsy (Liner echoendoscope [GF-UC240P-AL5], Olympus Corporation, Tokyo, Japan; Aspiration needle [Expect], Boston Scientific, MA, United States) demonstrated spindle-shaped cells without abnormal mitosis. Immunohistochemical staining was positive for S-100 protein and the expression level of Ki-67 was 2%-3%. These findings were strongly suggestive of a benign esophageal schwannoma. In view of the large tumor size, recent increase in size, and the patient’s symptoms, resection of the tumor by a combined endoscopic and thoracoscopic approach was planned.
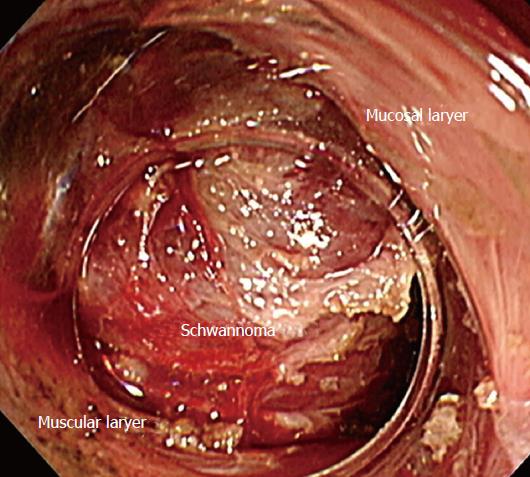
General anesthesia was administered using single-lumen endotracheal intubation for bilateral lung ventilation. The endoscopic procedure was performed in the supine position. We created a submucosal tunnel 40 mm proximal to the oral edge of the tumor and dissected its cranial end from the mucosal and muscular layers (Figure 3). We used two kinds of electrocautery knives [triangle-tip knife (KD-640L), and insulated-tip knife (KD-611L), Olympus Corporation, Tokyo, Japan] combined with an electrosurgical unit (ERBE VIO 300D, ERBE Corporation, Tuebingen, Germany). Endoscopic dissection was limited to about 30 mm of the tumor and could not proceed further owing to the limited mobility of the tumor within the submucosal tunnel. Thereafter, the patient was placed in the prone position, and a left thoracoscopic access was achieved under 8 mmHg of artificial pneumothorax. The following ports were placed: 5-mm ports at the mid-axillary line in the 3rd intercostal space (ICS), and the posterior axillary line in the 5th ICS, respectively, for the assistant; a 5-mm port at the mid-axillary line in the 8th ICS for grasping forceps; a 12-mm operating port at the posterior axillary line in the 7th ICS; and a 12-mm optical port at the posterior axillary line in the 9th ICS.
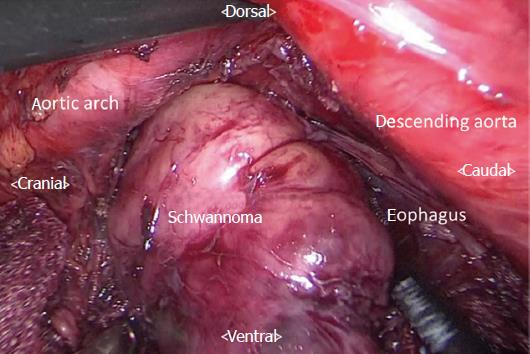
The surface of the tumor was easily identified on incising the esophageal muscular layer and dissection was performed along the tumor surface to enable its enucleation (Figure 4). The resected tumor was delivered out through the 12-mm operating port (7th ICS). We repaired the mucosal layer away from the site of mucosal entry since it was damaged partially during the thoracoscopic procedure. The muscular layer of the esophagus was sutured separately by using a continuous barbed absorbable suture (V-Loc180, Medtronics, United States). The endoscopic defect, created for gaining mucosal entry for tunneling, was closed by using endoscopic clips. The total operation time was 498 min (thoracoscopic procedure: 317 min) and the total blood loss was 40 g. The post-operative course of the patient was uneventful. Oral diet was resumed from postoperative day 7 and the patient was discharged on postoperative day 9.
Esophageal SMTs constitute less than 1% of all esophageal tumors. The most common among them are leiomyomas, with esophageal schwannomas accounting for 2%-3.4% of all esophageal SMTs[5,13]. Enucleation is considered as the treatment of choice for benign tumors that are symptomatic or rapidly increasing in size[1]. Video-assisted thoracoscopic surgery including thoracoscopic enucleation is described as a minimally invasive surgical procedure for esophageal SMT[5]. Performing thoracoscopic enucleation in the prone position, as compared with thoracotomy or thoracoscopic surgery in the decubitus position, has the advantages of adequate working area, minimal blood loss, and short postoperative stay[2,3]. However, the possibility of thoracoscopic enucleation may be limited by the tumor location and size. Sato et al. reported that cases with tumor size of 50 mm or more, and tumor location at the upper esophagus, usually required thoracotomy[1]. Watanabe et al[6] reported the need to convert from thoracoscopic enucleation to thoracoscopic subtotal esophagectomy owing to the location of an esophageal schwannoma at the upper thoracic esophagus, and its size being in excess of 50 mm. Therefore, thoracotomy or esophagectomy would be usually chosen for tumors that are 50 mm or more in size or located in the upper and middle thirds of the thoracic esophagus. The laterality of the tumor may determine the side of thoracic access. Esophageal surgery, especially for esophagectomy, is usually performed through the right thoracic cavity. Although, the left thoracic approach may provide direct access to a tumor on the left esophageal wall, the aortic arch and the trachea may restrict this access, especially for tumors located in the upper and middle thoracic esophagus. The left thoracic approach is usually applied for tumors located in the lower thoracic esophagus or at the esophagogastric junction[13,14].
SET is a recently developed technique for the treatment of esophageal SMT and was described by Inoue et al[7]. This technique allows for a complete endoscopic tumor resection, and is associated with earlier onset of per-oral intake, shorter hospital stay, and minimal short-term complications. On the other hand, SET is only recommended for tumors up to 40 mm in size owing to the limited submucosal space available.
In the present case, the tumor originated in the left wall of the mid-thoracic esophagus and had a maximal diameter of 60 mm. Since the aortic arch and the main bronchus restricted left-sided thoracoscopic access, and SET alone was not applicable owing to the tumor size, we combined the two procedures to overcome their respective limitations. To avoid the aortic arch and the left bronchus in the thoracoscopic approach, we attempted to remove the cranial side of the tumor to the maximum extent possible by endoscopic dissection.
To our knowledge, this combined approach has not been reported for tumors involving the upper and middle thoracic esophagus. Kanetaka et al[15] applied a similar approach for a large esophageal leiomyoma that originated from the lower thoracic esophagus. However, lower mediastinal tumors may be relatively easily resected by thoracoscopy alone. In our case, endoscopic tunneling was required since the tumor was located in the middle thoracic esophagus, and complete tumor resection by the thoracoscopic approach was considered difficult. Indications for such a combined procedure may be further expanded to avoid unnecessary esophagectomy or thoracotomy.
Recently, the submucosal tunneling endoscopic resection (STER) technique has been used for the resection of esophageal GISTs[7,16,17]. The combined approach can aid in the removal of GISTs without disrupting the tumor capsule. However, further studies are necessary to evaluate whether this procedure is applicable for malignant tumors such as GISTs[7].
In conclusion, this case report describes the successful resection of a large esophageal schwannoma by a combined method of endoscopic and thoracoscopic surgery. This method may be a possible minimally invasive treatment option for large esophageal SMT.
A 47-year-old woman with no significant medical history presented with dysphagia.
Esophageal submucosal tumor located in the middle thoracic esophagus.
Leiomyoma, gastrointestinal stromal tumor, schwannoma, or other submucosal tumor.
All laboratory results were within normal limits.
Computed tomography imaging demonstrated a 60-mm-long tumor located in the middle thoracic esophagus, adjacent to the aortic arch.
Benign esophageal schwannoma.
Combined thoracoscopic and endoscopic tumor resection.
Esophageal schwannoma is a relatively rare esophageal submucosal tumor. Large esophageal schwannomas usually require thoracotomy or esophagectomy for their successful resection.
Combined thoracoscopic and endoscopic tumor resection can facilitate the resection of large esophageal submucosal tumors located in the upper or middle thoracic esophagus by minimally invasive surgery.
The paper is well written.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Gupta V, Tsolakis AV S- Editor: Gong ZM L- Editor: A E- Editor: Ma YJ
| 1. | Sato S, Takagi M, Watanabe M, Nagai E, Kyoden Y, Ohata K, Oba N, Suzuki M, Fukuchi K, Iseki J. A case report of benign esophageal schwannoma with FDG uptake on PET-CT and literature review of 42 cases in Japan. Esophagus. 2012;9:165-171. [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Claus CM, Cury Filho AM, Boscardim PC, Andriguetto PC, Loureiro MP, Bonin EA. Thoracoscopic enucleation of esophageal leiomyoma in prone position and single lumen endotracheal intubation. Surg Endosc. 2013;27:3364-3369. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Palanivelu C, Rangarajan M, Senthilkumar R, Annapoorni S, Jategaonkar PA. Thoracoscopic management of benign tumors of the mid-esophagus: a retrospective study. Int J Surg. 2007;5:328-331. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Palanivelu C, Prakash A, Senthilkumar R, Senthilnathan P, Parthasarathi R, Rajan PS, Venkatachlam S. Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position--experience of 130 patients. J Am Coll Surg. 2006;203:7-16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 314] [Cited by in F6Publishing: 357] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 5. | Shin S, Choi YS, Shim YM, Kim HK, Kim K, Kim J. Enucleation of esophageal submucosal tumors: a single institution’s experience. Ann Thorac Surg. 2014;97:454-459. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Watanabe T, Miyazaki T, Saito H, Yoshida T, Kumakura Y, Honjyo H, Yokobori T, Sakai M, Sohda M, Kuwano H. Resection of an esophageal schwannoma with thoracoscopic surgery: a case report. Surg Case Rep. 2016;2:127. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Inoue H, Ikeda H, Hosoya T, Onimaru M, Yoshida A, Eleftheriadis N, Maselli R, Kudo S. Submucosal endoscopic tumor resection for subepithelial tumors in the esophagus and cardia. Endoscopy. 2012;44:225-230. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 197] [Cited by in F6Publishing: 223] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 8. | Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265-271. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1168] [Cited by in F6Publishing: 1109] [Article Influence: 79.2] [Reference Citation Analysis (0)] |
| 9. | Hiki N, Yamamoto Y, Fukunaga T, Yamaguchi T, Nunobe S, Tokunaga M, Miki A, Ohyama S, Seto Y. Laparoscopic and endoscopic cooperative surgery for gastrointestinal stromal tumor dissection. Surg Endosc. 2008;22:1729-1735. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 297] [Cited by in F6Publishing: 317] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 10. | Ntourakis D, Mavrogenis G. Cooperative laparoscopic endoscopic and hybrid laparoscopic surgery for upper gastrointestinal tumors: Current status. World J Gastroenterol. 2015;21:12482-12497. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 43] [Cited by in F6Publishing: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 11. | Irino T, Nunobe S, Hiki N, Yamamoto Y, Hirasawa T, Ohashi M, Fujisaki J, Sano T, Yamaguchi T. Laparoscopic-endoscopic cooperative surgery for duodenal tumors: a unique procedure that helps ensure the safety of endoscopic submucosal dissection. Endoscopy. 2015;47:349-351. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Ichikawa D, Komatsu S, Dohi O, Naito Y, Kosuga T, Kamada K, Okamoto K, Itoh Y, Otsuji E. Laparoscopic and endoscopic co-operative surgery for non-ampullary duodenal tumors. World J Gastroenterol. 2016;22:10424-10431. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 36] [Cited by in F6Publishing: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 13. | Kang SK, Yun JS, Kim SH, Song SY, Jung Y, Na KJ. Retrospective analysis of thoracoscopic surgery for esophageal submucosal tumors. Korean J Thorac Cardiovasc Surg. 2015;48:40-45. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Shichinohe T, Kato K, Ebihara Y, Kurashima Y, Tsuchikawa T, Matsumoto J, Nakamura T, Tanaka E, Hirano S. Thoracoscopic enucleation of esophageal submucosal tumor by prone position under artificial pneumothorax by CO2 insufflation. Surg Laparosc Endosc Percutan Tech. 2014;24:e55-e58. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Kanetaka K, Minami H, Kuroki T, Nakao K, Eguchi S. Successful resection of large esophageal leiomyoma by a combined thoracoscopic-endoscopic submucosal tunneling method. Gastrointestinal endoscopy. 2016;83:1027-1028. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Tan Y, Tang X, Guo T, Peng D, Tang Y, Duan T, Wang X, Lv L, Huo J, Liu D. Comparison between submucosal tunneling endoscopic resection and endoscopic full-thickness resection for gastric stromal tumors originating from the muscularis propria layer. Surgical endoscopy. 2017;31:3376-3382. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 17. | Jiao CH, Yang SP, Li XL, Ding J, Xu YH, Tao G, Chen L, Zhang DQ, He X, Chen WK. [Preliminary exploration on submucosal tunneling endoscopic resection for middle and lower esophagus submucosal tumors]. Zhonghua Yixue Zazhi. 2013;93:2388-2391. [PubMed] [Cited in This Article: ] |