Published online Jun 28, 2020. doi: 10.3748/wjg.v26.i24.3495
Peer-review started: February 14, 2020
First decision: April 22, 2020
Revised: May 19, 2020
Accepted: May 30, 2020
Article in press: May 30, 2020
Published online: June 28, 2020
The over-the-scope clip (OTSC) system has been increasingly utilized as a non-surgical option to endoscopically manage refractory gastrointestinal (GI) hemorrhage, perforations/luminal defects and fistulas. Limited data exist evaluating the efficacy and safety of OTSC.
To determine the clinical success and adverse event (AE) rates of OTSC across all GI indications.
A PubMed search was conducted for eligible articles describing the application of the OTSC system for any indication in the GI tract. Any article or case series reporting data for less than 5 total patients was excluded. The primary outcome was the rate of clinical success. Secondary outcomes included: Technical success rate, OTSC-related AE rate and requirement for surgical intervention despite-OTSC placement. Pooled rates (per-indication and overall) were calculated as the number of patients with the event of interest divided by the total number of patients.
A total of 85 articles met our inclusion criteria (n = 3025 patients). OTSC was successfully deployed in 94.4% of patients (n = 2856/3025). The overall rate of clinical success (all indications) was 78.4% (n = 2371/3025). Per-indication clinical success rates were as follows: (1) 86.0% (1120/1303) for GI hemorrhage; (2) 85.3% (399/468) for perforation; (3) 55.8% (347/622) for fistulae; (4) 72.6% (284/391) for anastomotic leaks; (5) 92.8% (205/221) for defect closure following endoscopic resection (e.g., following endoscopic mucosal resection or endoscopic submucosal dissection); and (6) 80.0% (16/20) for stent fixation. AE’s related to the deployment of OTSC were only reported in 64 of 85 studies (n = 1942 patients), with an overall AE rate of 2.1% (n = 40/1942). Salvage surgical intervention was required in 4.7% of patients (n = 143/3025).
This systematic review demonstrates that the OTSC system is a safe and effective endoscopic therapy to manage GI hemorrhage, perforations, anastomotic leaks, defects created by endoscopic resections and for stent fixation. Clinical success in fistula management appears limited. Further studies, including randomized controlled trials comparing OTSC with conventional and/or surgical therapies, are needed to determine which indication(s) are the most effective for its use.
Core tip: This systematic review demonstrates that the over-the-scope clip (OTSC) system is a safe and effective endoscopic therapy to manage gastrointestinal hemorrhage, perforations, anastomotic leaks, defects created by endoscopic resections and for stent fixation. Clinical success in fistula management appears limited. Further studies, including randomized controlled trials comparing OTSC with conventional and/or surgical therapies, are needed to determine which indication(s) are the most effective for its use.
- Citation: Bartell N, Bittner K, Kaul V, Kothari TH, Kothari S. Clinical efficacy of the over-the-scope clip device: A systematic review. World J Gastroenterol 2020; 26(24): 3495-3516
- URL: https://www.wjgnet.com/1007-9327/full/v26/i24/3495.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i24.3495
Acute (primary or refractory) gastrointestinal (GI) hemorrhage, perforation, GI fistulae, and anastomotic leaks are frequent occurrences in clinical GI practice that have been conventionally managed with surgery; however, the over-the-scope-clip (OTSC) system (Ovesco Endoscopy AG, Tübingen, Germany) has increasingly become an effective endoscopic treatment option in many cases as a primary and salvage treatment option, thereby decreasing the need for surgical intervention.
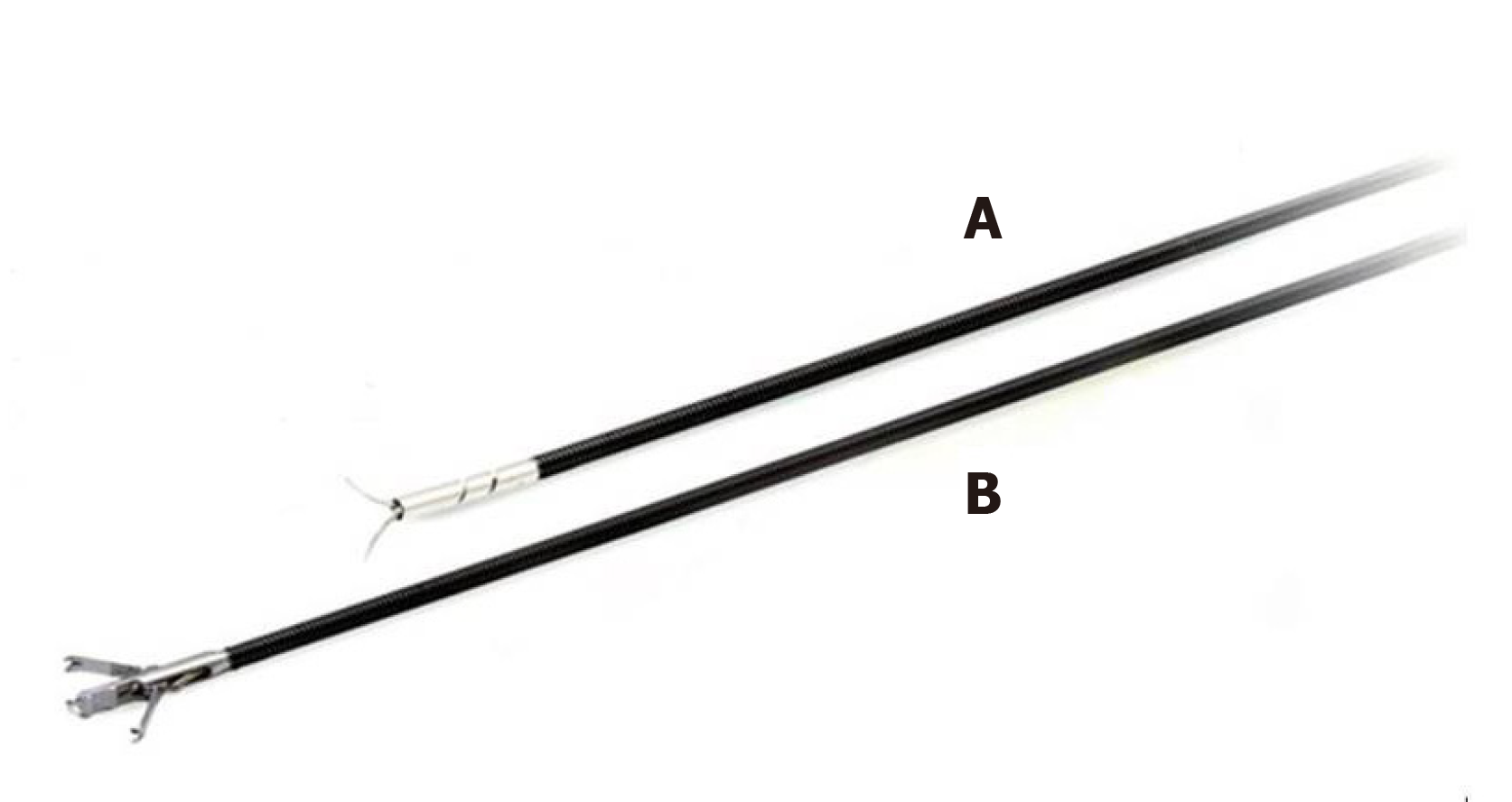
The OTSC system is a novel mechanical clipping device that allows for the endoscopic closure of large GI defects. It consists of an applicator cap, mounted clip, a hand wheel, thread, and thread retriever[1]. The clip is made of a super-elastic alloy (Nitinol), which is a biocompatible and magnetic resonance imaging conditional material (can be retained as a long-term implant)[1]. The applicator cap is available in a variety of sizes to accommodate endoscopes of different diameters (Table 1). The OTSC clips are offered in three different shapes (a, t, and gc) amenable to each indication: (1) Type “a” clips are blunted to provide compression of tissues and primarily used for hemostasis; (2) Type “t” clips have small spikes and blunted edges allowing for both compression and anchoring into tissues, and can be used for relatively thin walled portions of the GI tract such as the small intestine or colon; and (3) Type “gc” clips have elongated teeth (with spikes), which are primarily indicated for closure of gastric wall defects (Figure 1)[1]. Auxiliary accessories have recently become commercially available, including a clip designed for stent-fixation (Stentfix OTSC system; Ovesco Endoscopy AG, Tübingen, Germany), a smaller diameter applicator and clip for smaller lumens (mini OTSC; Ovesco Endoscopy AG, Tübingen, Germany), full thickness resection device (FTRD, Ovesco Endoscopy AG, Tübingen, Germany), and two forceps-like devices (OTSC Anchor, OTSC Twin Grasper; Ovesco Endoscopy AG, Tübingen, Germany). The Twin Grasper (TG) facilitates the approximation of gaping edges of a lesion prior to deployment of the OTSC clip (Figure 2), whereas the Anchor is able precisely align the target tissue and applicator cap, thus allowing for better approximation of tissue (especially when indurated)[1].
| OTSC cap options | ||||
| Mini (10) | 11 | 12 | 14 | |
| Scope outer diameter compatibility | 8.5-9.8 mm | 8.5-11 mm | 10.5-12 mm | 11.5-14 mm |
| Diagnostic gastroscopes | Diagnostic gastroscopes | 1T/2T gastroscopes, peds colonoscopes | Adult colonoscopes | |
| Maximum outer diameter of cap | 14.65 mm | 16.5 mm | 17.5 mm | 21 mm |
| Thread length | 165 cm | 165 cm | 165 cm or 220 cm | 220 cm |
| Depth of applicator cap | ||||
| 3 mm | a, t | a, t | a, t | a, t |
| 6 mm | N/A | a, t | a, t, gc1 | a, t |
The OTSC is delivered by means of an applicator cap mounted to the end of the endoscope using a thread retriever. If necessary, the TG or Anchor forceps may be used to allow for better approximation of the lesion. Turning the hand wheel attached to the working channel of the endoscope allows for the thread connected to the applicator cap to tighten, thus deploying the clip to the targeted defect[1]. An additional clip may be used if a single clip does not sufficiently achieve adequate closure.
Kirschniak et al[2] first reported the clinical application of OTSC in 2007. The authors described seven refractory bleeding events, two iatrogenic perforations and two defects following endoscopic resection that were successfully managed with OTSC. A significant advantage of the OTSC system is the ability to achieve closure of luminal defects, or complex bleeding lesions with the deployment of a single clip, thus making its deployment more efficient than prior endoscopic strategies which utilized multiple through the scope (TTS) clips[3,4]. Prior to the availability of OTSC, complex luminal defects encountered during endoscopic procedures were often unable to be closed with conventional TTS clips due to lack of their ability to adequately approximate the defect margins, thus requiring surgical intervention in many instances. Furthermore, in the context of GI hemorrhage, the literature supports the use of OTSC when conventional endoscopic therapies fail[5,6].
Advancements in therapeutic interventions across endoscopic practice currently facilitate larger and deeper resections of GI lesions, with a concurrent increase in iatrogenic injury[7-9]. OTSC has utility as a “real-time” intervention, allowing the endoscopist to effectively manage adverse events (AEs) quickly (such as bleeding and perforation) during the index procedure.
Since its inception, OTSC has become integrated into endoscopic practice internationally, with varying degrees of clinical success[10-12]. Though the OTSC system has been available for over ten years, it continues to benefit from iteration as further product development continues to take place. Data describing its use in the treatment of GI hemorrhage, perforation, anastomotic leaks, fistulae, defect closure after endoscopic resection and stent fixation is limited to primarily retrospective cohort studies and case series. Compiling and studying these published data in an organized manner would provide a more comprehensive understanding of the efficacy and safety profile of OTSC. This systematic review aims to determine the clinical success and AE rates of OTSC across various GI indications for use.
This systematic review was performed according to the preferred reporting items for systematic reviews and meta-analysis statement[13]. A thorough search of the literature was conducted in the PubMed database to identify articles that described the use of OTSC for any GI indication from January 1, 2007 to January 15, 2020. The search was performed using the following terms: “over-the-scope-clip”, “OTSC”, “endoscopic fistula closure,” “over-the-scope clip bleeding”, “stent fixation”, and “endoscopic perforation closure.”
All English-language abstracts and/or full-text articles reporting original data of OTSC use (in humans, only) for the indication of fistulae, perforation, anastomotic leak closure, GI hemorrhage, endoscopic resection, and stent fixation were reviewed (authors: Bartell N and Bittner K) to assess eligibility for inclusion. Case reports and case series with fewer than five patients were excluded. Articles were also omitted if reported data did not include the rate of clinical success.
Data extraction included the following: Author(s), year of publication, study type/design, location(s), number of patients, indication(s) for OTSC use, clinical and technical success rates (TSR), duration of follow-up, and OTSC-related AEs. The primary outcome of interest was clinical success rate (CSR). Secondary outcomes included TSR, requirement for surgical intervention despite OTSC, and reported OTSC-related AEs. Pooled rates (per-indication and overall) were calculated as the number of patients with the event of interest divided by the total number of patients.
CSR was defined as complete and durable resolution of the respective defect, hemorrhage and/or stent fixation. TSR was defined as the successful deployment of the OTSC clip to the targeted lesion or defect. OTSC-related AEs were defined as unanticipated events probably or possibly directly related to the use of the OTSC clip.
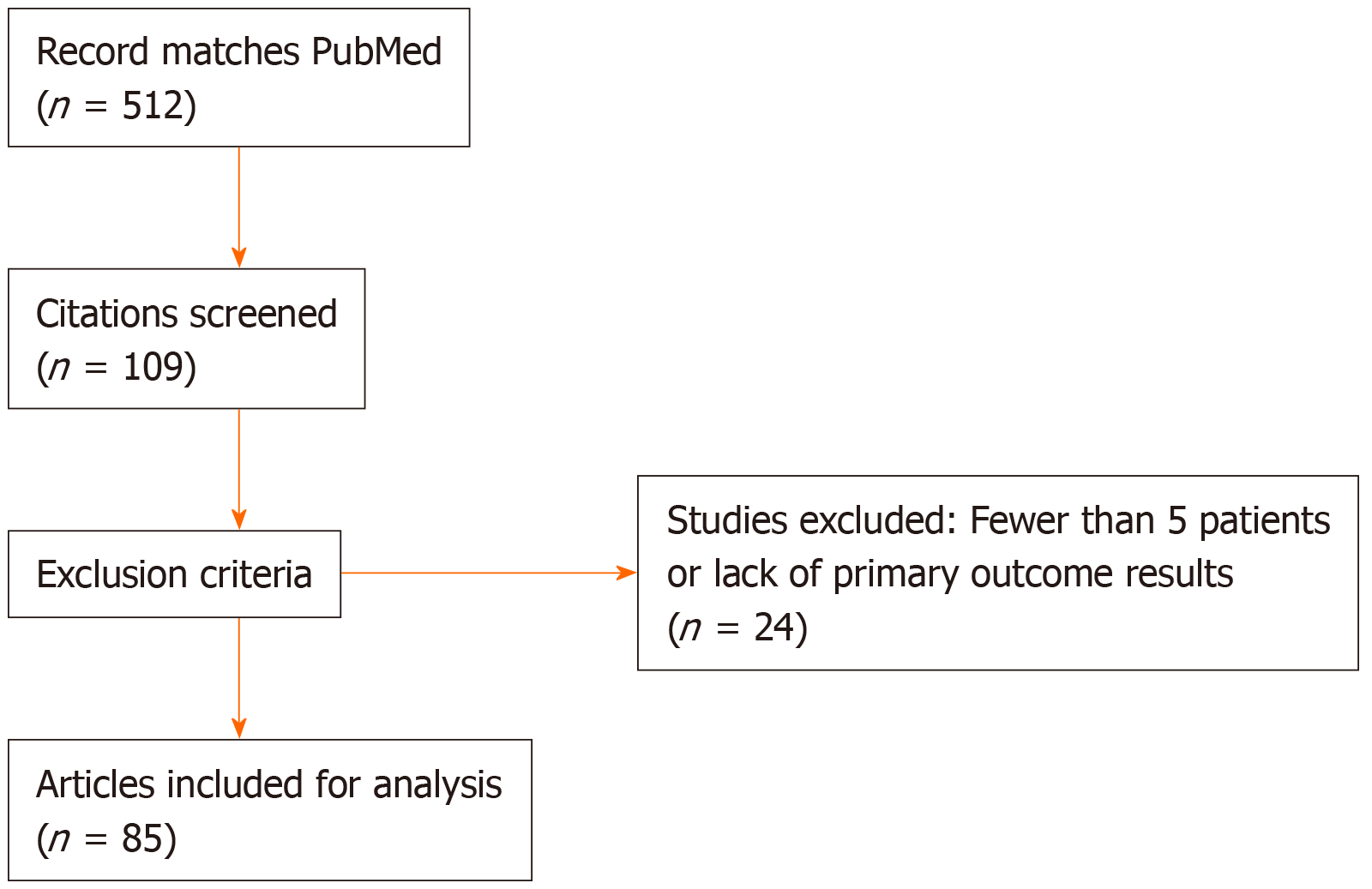
A total of 512 record matches were located in the PubMed database, per the literature search strategy. Two authors (Bartell N and Bittner K) reviewed each title, abstract and/or full-text article prior to applying the full exclusion criteria. A total of 109 publications were retrieved for full review, with 24 excluded from the final analysis (Figure 3). Eighty-five articles[2-6,14-92] (Table 2) met inclusion criteria (n = 3025 patients). Indications for OTSC use included: Fistulae (n = 622), GI hemorrhage (n = 1303), perforation (n = 468), anastomotic leak closure (n = 391), endoscopic resection defect closure (n = 221), and stent fixation (n = 20). The overall CSR (inclusive of all indications) and TSR for OTSC placement was 78.4% (n = 2371/3025) and 94.4% (n = 2856/3025), respectively. Per-indication CSR, TSR, and post-OTSC surgery rates are described in Table 3.
| Ref. | Year | Type of study | Country | Patients (n) | Overall clinical success rate (%) | Follow-up (wk) | Adverse events,n (%) | ||||||
| Indications | Total | ||||||||||||
| Fistula | Bleeding | Perforation | Leak | ER | Stent fixation | ||||||||
| Seebach et al[15] | 2010 | Case series Retrospective | Switzerland | 7 | - | - | 57.1 | - | - | - | 57.1 | 10-42 | NR |
| Kirschniak et al[2] | 2007 | Retrospective | Germany | 11 | - | 100 | 100 | - | 100 | - | 100 | 1-5 | 0.0 |
| Mudumubi et al[16] | 2014 | Retrospective | International1 | 12 | - | - | - | - | - | 83.3 | 83.3 | 3-40 | 0.0 |
| Sandmann et al[17] | 2011 | Case series Retrospective | Germany | 11 | 100 | - | 100 | 66 | 100 | - | 90.9 | 12.7 | NR |
| Albert et al[18] | 2011 | Retrospective | Germany | 19 | - | 57.1 | - | 66.7 | - | - | 63.2 | 1-68 | 0.0 |
| Repici et al[19] | 2009 | Case series Retrospective | Italy | 9 | - | 100 | - | - | 100 | - | 100 | 4-12 | 0.0 |
| Donatelli et al[20] | 2016 | Retrospective | International2 | 45 | 36.7 | - | 100 | - | - | - | 57.8 | 36-100 | 0.0 |
| Maekawa et al[21] | 2015 | Prospective | Japan | 12 | - | - | - | - | 91.7 | - | 91.7 | NR | 0.0 |
| Gautier et al[22] | 2015 | Retrospective Multi-center | France | 17 | 11.8 | - | - | - | - | - | 11.8 | 12 | NR |
| Nishiyama et al[23] | 2013 | Retrospective | Japan | 23 | 75 | 77.8 | 75 | - | 100 | - | 82.6 | 2-8 | 0.0 |
| Voermans et al[24] | 2012 | Prospective Multi-center | Netherlands | 36 | - | - | 88.9 | - | - | - | 88.9 | 1-26 | 0.0 |
| Lee et al[26] | 2017 | Prospective Multi-center | Korea | 19 | 25 | - | 100 | 83.3 | 100 | - | 73.7 | 72 | 0.0 |
| Angsuwatcharakon et al[27] | 2016 | Retrospective | Thailand | 6 | - | - | 83.3 | - | - | - | 83.3 | NR | NR |
| Arezzo et al[28] | 2012 | Case series Prospective | Italy | 14 | - | - | - | 85.7 | - | - | 85.7 | 16 | 0.0 |
| Schlag et al[29] | 2013 | Prospective | Germany | 6 | - | - | 100 | - | - | - | 100 | 4-12 | 0.0 |
| Disibeyaz et al[30] | 2012 | Case series Retrospective | Turkey | 9 | 33.3 | - | 100 | 60 | - | - | 55.6 | NR | 0.0 |
| Gubler et al[31] | 2012 | Case series Prospective | Switzerland | 14 | - | - | 85.7 | - | - | - | 85.7 | 4-48 | NR |
| Singhal et al[32] | 2014 | Case Series Prospective | United States | 10 | 90 | - | - | - | - | - | 90 | 7 | 0.0 |
| Mennigen et al[33] | 2013 | Case series Retrospective | Germany | 14 | 71.4 | - | 100 | 83.3 | - | - | 78.6 | 1-68 | 0.0 |
| Faehndrich et al[34] | 2015 | Retrospective | Germany | 17 | - | - | - | - | 94.1 | - | 94.1 | NR | 0.0 |
| Schmidt et al[4] | 2015 | Prospective Multi-center RCT | International3 | 24 | - | - | - | - | 75 | - | 75 | 4 | 2 (8.3) |
| Guo et al[35] | 2015 | Retrospective | China | 23 | - | - | - | - | 100 | - | 100 | 4-24 | 2 (8.7) |
| Correia et al[36] | 2014 | Case series Prospective | Portugal | 6 | 80 | - | 100 | - | - | - | 83.3 | NR | 0.0 |
| Goenka et al[37] | 2017 | Prospective | India | 12 | 66 | 100 | 100 | - | - | - | 91.7 | 4-8 | 0.0 |
| Surace et al[38] | 2011 | Prospective | Italy | 19 | 73.7 | - | - | - | - | - | 73.7 | 32 | 1 (5.3) |
| Kochhar et al[39] | 2017 | Case series Prospective | United States | 12 | - | - | - | 66.7 | - | - | 66.7 | 60 | 1 (8.3) |
| Manta et al[40] | 2017 | Prospective | Italy | 76 | - | - | - | 80.3 | - | - | 80.3 | NR | 0.0 |
| Parodi et al[41] | 2010 | Prospective | Italy | 10 | 80 | - | 100 | 50 | - | - | 80.0 | NR | 0.0 |
| Manta et al[42] | 2011 | Case series Retrospective | Italy | 12 | 87.5 | - | - | 75 | - | - | 83.3 | 4 | 0.0 |
| Honegger et al[43] | 2017 | Retrospective Cohort | Switzerland | 203 | 29.8 | 77.4 | 86.1 | 33.3 | - | 66.7 | 63.1 | 4 | 6 (3.0) |
| Manno et al[44] | 2015 | Retrospective | International4 | 40 | - | 100 | - | - | - | - | 100 | 4 | 0.0 |
| Richter-Schrag et al[45] | 2016 | Retrospective | Germany | 100 | - | 78 | - | - | - | - | 78 | NR | NR |
| Aepli et al[46] | 2016 | Retrospective | Switzerland | 24 | - | - | - | - | 87.5 | - | 87.5 | NR | 4 (16.7) |
| Law et al[48] | 2015 | Retrospective Multi-center | United States | 47 | 53.2 | - | - | - | - | - | 53.2 | 26 | 0.0 |
| Farnik et al[3] | 2015 | Retrospective Multi-center | International5 | 34 | - | - | 100 | 56.3 | - | - | 70.5 | 39 | 0.0 |
| Jacobsen et al[49] | 2012 | Retrospective | United States | 10 | 0 | - | 100 | 80 | - | - | 70.0 | 12 | 0.0 |
| Haito-Chavez et al[50] | 2014 | Retrospective Multi-center | International6 | 161 | 42.9 | - | 90 | 73.3 | - | - | 60.2 | 18 – 30 | 0.0 |
| Winder et al[51] | 2016 | Retrospective | United States | 28 | 77.2 | - | - | 100 | - | - | 82.1 | 19 | 0.0 |
| Sulz et al[52] | 2014 | Case series Prospective | Switzerland | 19 | 54.5 | 100 | - | 66.7 | - | 100 | 63.1 | NR | 0.0 |
| Magdeburg et al[53] | 2015 | Prospective | Germany | 43 | - | - | 97.8 | - | - | - | 97.8 | NR | 3 (7.0) |
| Wedi et al[54] | 2016 | Retrospective | France | 84 | 100 | 89.3 | 57.1 | - | 100 | - | 89.3 | NR | 2 (2.4) |
| Keren et al[55] | 2014 | Case series Prospective | Israel | 26 | - | - | - | 80.8 | - | - | 80.8 | NR | 0.0 |
| Raithel et al[14] | 2017 | Retrospective Multi-center | Germany | 34 | - | - | 74.1 | 85.7 | - | - | 76.5 | NR | 3 (8.8) |
| Kobara et al[56] | 2017 | Retrospective Multi-center | Japan | 58 | 83.3 | 83.3 | - | 85.7 | - | - | 84.5 | 4+ | 1 (1.8) |
| Hagel et al[57] | 2012 | Case series Prospective | Germany | 17 | - | - | 64.7 | - | - | - | 64.7 | 4 | NR |
| Nasa et al[58] | 2016 | Case series Retrospective | India | 7 | 80 | 100 | 100 | - | - | - | 85.7 | 45 | NR |
| Skinner et al[6] | 2014 | Retrospective | United States | 12 | - | 83.3 | - | - | - | - | 83.3 | 10 – 30 | 0.0 |
| Al-Bawardy et al[59] | 2017 | Retrospective | United States | 7 | - | - | - | - | 100 | - | 100 | 1 – 86 | 0.0 |
| Sarker et al[60] | 2014 | Retrospective | United States | 8 | - | - | - | - | 100 | - | 100 | 4 – 52 | 0.0 |
| Mangiavillano et al[61] | 2016 | Retrospective | Italy | 20 | - | - | 90 | - | - | - | 90 | 12 | NR |
| Aiolfi et al[62] | 2014 | Retrospective | Italy | 7 | - | - | - | 85.7 | - | - | 85.7 | NR | NR |
| Manta et al[5] | 2013 | Case series Multi-center | Italy | 30 | - | 90 | - | - | - | - | 90 | 1 – 4 | 0.0 |
| Mangiafico et al[63] | 2017 | Case series Prospective | International7 | 7 | 100 | - | - | - | - | - | 100 | 2 – 8 | 0.0 |
| Niland et al[64] | 2017 | Retrospective | United States | 14 | 21.4 | - | - | - | - | - | 21.4 | 26 | 0.0 |
| Schmdtt et al[4] | 2018 | Prospective RCT | International8 | 33 | - | 84.8 | - | - | - | - | 84.8 | 4 | 0.0 |
| Heinrich et al[65] | 2017 | Case series Retrospective | Switzerland | 5 | 100 | - | - | - | - | - | 100 | 46 – 269 | 0.0 |
| Prosst et al[66] | 2015 | Prospective | Germany | 20 | 90 | - | - | - | - | - | 90 | 24 | 0.0 |
| Mizrahi et al[67] | 2016 | Prospective | United States | 51 | 35.3 | 75 | 75 | 50 | - | 50 | 49.0 | 48 | NR |
| Kirschniak et al[68] | 2011 | Retrospective | Germany | 46 | 37.5 | 93 | 100 | - | - | - | 84.8 | 1 – 2 | 0.0 |
| Mennigen et al[69] | 2015 | Retrospective | Germany | 10 | 70 | - | - | - | - | - | 70 | 22 – 75 | 0.0 |
| Wedi et al[70] | 2016 | Retrospective Case series | International9 | 6 | - | 100 | - | - | - | - | 100 | NR | NR |
| Baron et al[71] | 2012 | Retrospective Multi-center | United States | 43 | 67.9 | 100 | 80 | 33.3 | - | - | 72.1 | 4 – 11 | 2 (4.7) |
| Lamberts et al[72] | 2017 | Retrospective | Germany | 75 | - | 65.3 | - | - | - | - | 65.3 | NR | NR |
| Soetikno et al[73] | 2016 | Case series Retrospective | International10 | 5 | - | 100 | - | - | - | - | 100 | 60 | 0.0 |
| Wedi et al[74] | 2017 | Retrospective | International11 | 100 | - | 86 | - | - | - | - | 73 | NR | NR |
| Chan et al[75] | 2014 | Case series Prospective | China | 9 | - | 77.8 | - | - | - | - | 77.8 | 8 | NR |
| Keen et al[76] | 2019 | Prospective | United Kingdom | 59 | - | 93.2 | - | - | - | - | 93.2 | 4 | NR |
| Horenkamp-Sonntag et al[77] | 2019 | Retrospective | Germany | 92 | - | 82.4 | 87.9 | - | - | - | 92.4 | 14 | NR |
| Manta et al[78] | 2019 | Retrospective Multi-center | Italy | 286 | - | 94.4 | - | - | - | - | 94.4 | 4 | NR |
| Mercky et al[79] | 2015 | Retrospective | France | 30 | 73.3 | - | - | - | - | - | 73.3 | 42 | 3 (10) |
| Monkemuller et al[80] | 2014 | Case series Retrospective | Germany | 16 | 50 | 100 | - | 0 | 100 | 100 | 75 | 44 | 0.0 |
| Bonino et al[81] | 2014 | Case series Prospective | Italy | 26 | 90 | - | 68.8 | - | - | - | 76.9 | NR | 0.0 |
| Christophorou et al[82] | 2015 | Retrospective Multi-center | France | 14 | 78.5 | - | - | - | - | - | 78.5 | NR | NR |
| Lunse et al[83] | 2019 | Retrospective | Germany | 9 | 66.7 | - | - | - | - | - | 66.7 | 8 | 0.0 |
| Mosquera-Klinger et al[84] | 2019 | Retrospective Case series | Columbia | 14 | 70 | 100 | 100 | - | - | 100 | 78.6 | 20 | 0.0 |
| Brander et al[25] | 2017 | Retrospective | United States | 67 | - | 70.1 | - | - | - | - | 70.1 | 4 | NR |
| Meier et al[47] | 2017 | Retrospective | Germany | 10 | - | - | - | - | 100 | - | 100 | 12 | 0.0 |
| Tashima et al[85] | 2017 | Prospective | Japan | 50 | - | - | - | - | 94 | - | 94 | 2 | 4 (8) |
| Khater et al[86] | 2017 | Retrospective | France | 11 | - | - | 81.2 | - | - | - | 81.2 | NR | 1 (9) |
| Asokkumar et al[87] | 2018 | Retrospective | International12 | 19 | - | 100 | - | - | - | - | 100 | NR | 0.0 |
| Morrell et al[88] | 2019 | Retrospective | United States | 117 | 50.8 | - | - | 75 | - | - | 61.2 | 22 | 0.0 |
| Kappelle et al[89] | 2018 | Prospective | Netherlands | 13 | - | - | - | - | 84.6 | - | 84.6 | 24 | 5 (38.4) |
| Wei et al[90] | 2019 | Retrospective | China | 26 | - | - | 100 | - | - | - | 100 | 4 | 0.0 |
| Golder et al[91] | 2019 | Retrospective | Germany | 100 | - | 75 | - | - | - | - | 75 | NR | 0.0 |
| Wedi et al[92] | 2018 | Retrospective Multi-center | Germany | 118 | - | 92.4 | - | - | - | - | 92.4 | 4 | NR |
| Total | 3025 | 55.8% | 86.0% | 85.3% | 72.6% | 92.8% | 80.0% | 78.4% | - | 2.1% | |||
| 347/622 | 1120/1303 | 399/468 | 284/391 | 205/221 | 16/20 | 2371/3025 | - | 40/194213 | |||||
Endoscopic management of GI hemorrhage is well-established, with a number of available modalities to effectively achieve mechanical or coagulative hemostasis. Conventional endoscopic techniques are successful in managing GI hemorrhage in most cases; however, the rate of re-bleeding has been reported at 10%-20%[93]. Patients presenting with a re-bleed often require repeat endoscopic intervention, angiography (interventional radiology), or definitive management with surgery[93]. Mechanical hemostasis is often attempted with TTS clips which can be effective for smaller lesions; however, large and/or complex lesions may require a clip with larger diameter (up to 14 mm) and more tensile strength to achieve effective hemostasis.
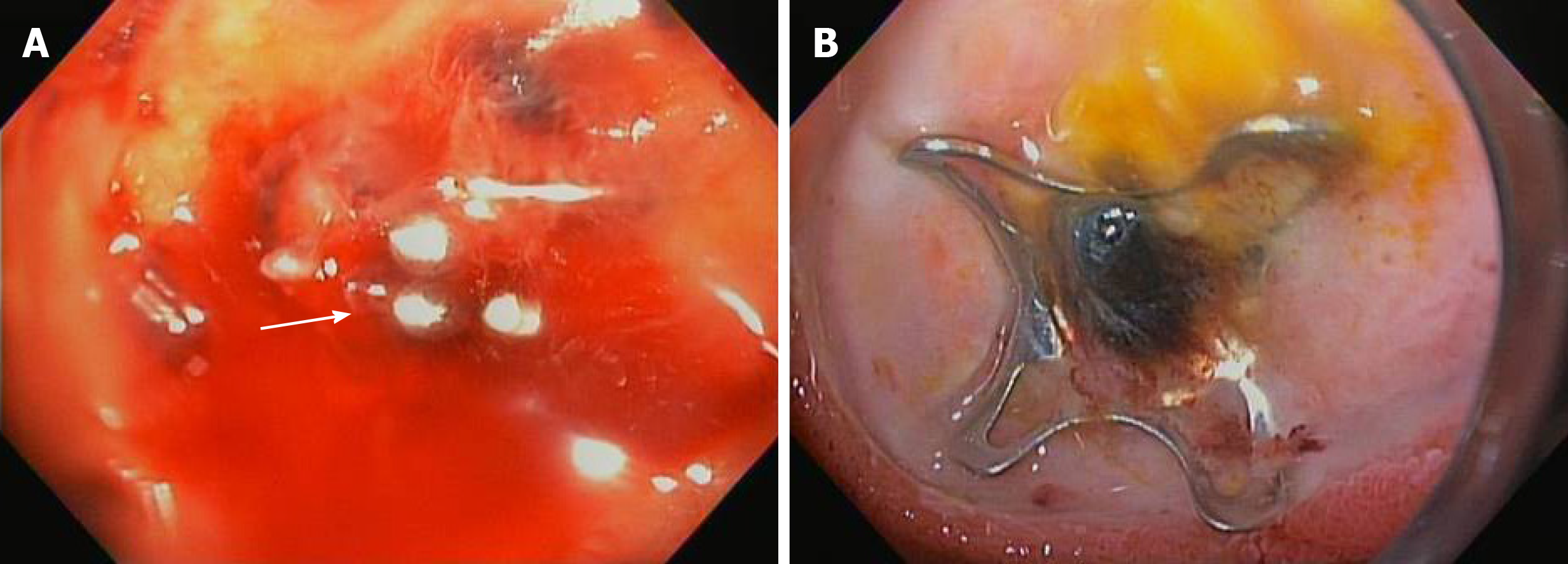
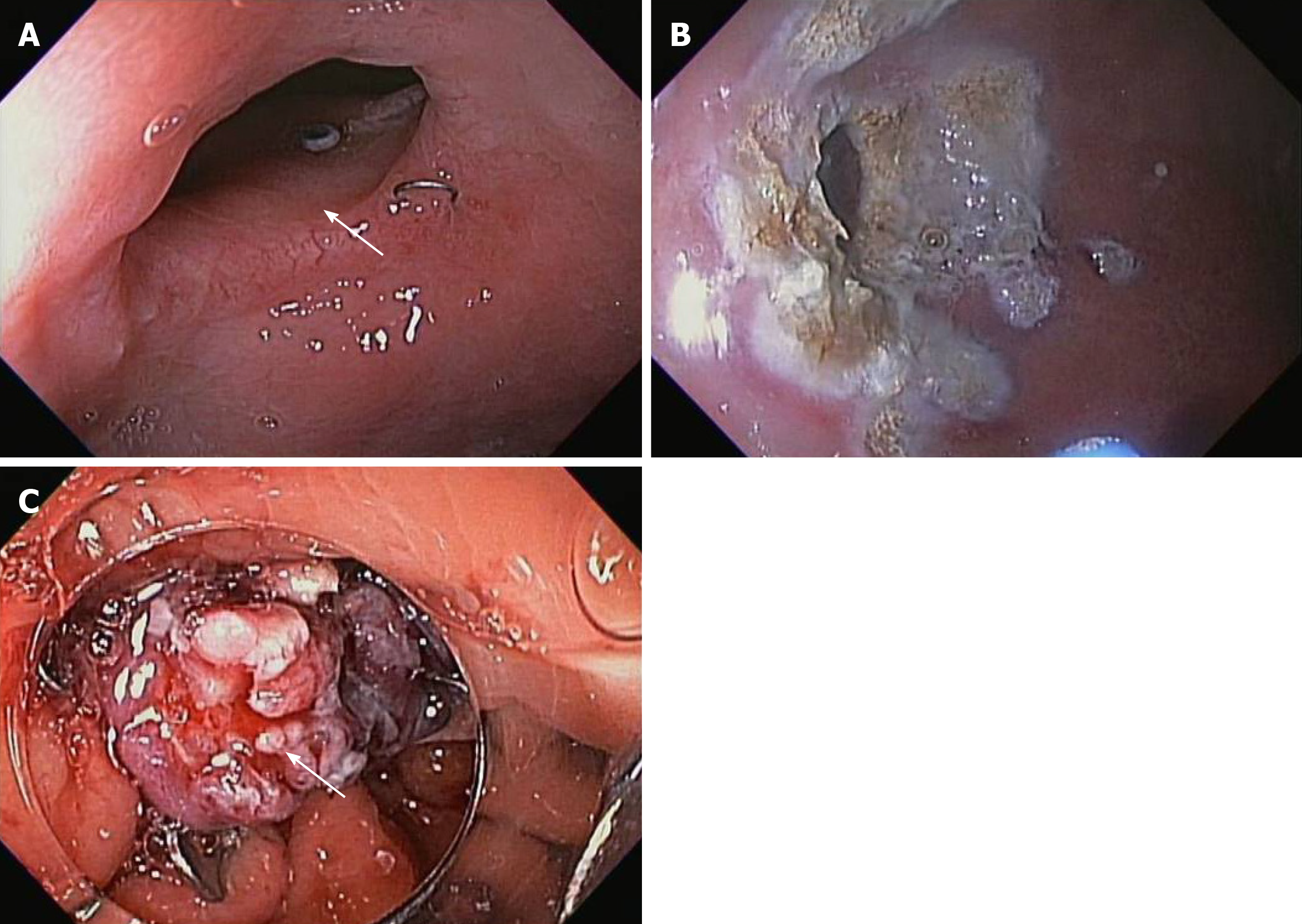
In current endoscopic practice, OTSC is mainly used in refractory bleeding cases (Figure 4) following a failure of conventional therapy; however, a head-to-head randomized control trial (RCT) is currently being conducted in Europe (ClinicalTrials.gov, NCT03551262) to evaluate its efficacy as a potential primary therapy for hemostasis. Manno et al[44] retrospectively reviewed 40 consecutive cases of high-risk non-variceal upper GI hemorrhage utilizing OTSC as a primary intervention. The authors reported a CSR of 100%, with no OTSC-related AEs (30-d follow up). In 2017, Wedi et al[74] highlighted the efficacy of OTSC in a retrospective review of 100 high-risk patients presenting with non-variceal upper GI bleeding. In this cohort, most (51%) of patients had severe cardiovascular comorbidities, with the majority (73%) on an antiplatelet regimen, thus potentially precluding a surgical approach in these patients. This article reported a CSR of 86% at 6 months of follow-up. In a subsequent study, Wedi et al[92] compared OTSC to standard of care treatment in non-variceal upper GI bleeding demonstrating superiority of OTSC, especially in high-risk patients. Specifically, patients with Rockall scores ≥ 8 showed significantly lower rates of re-bleeding when treated with OTSC as a first-line therapy as compared to patients treated with conventional modalities (10.9% vs 27.9%, respectively)[92]. Thus, OTSC can be used as the primary modality in high-risk patients such as those on anticoagulation, bleeding from large caliber vessels, or if they are not a good surgical candidate and/or as a rescue treatment for re-bleeding when conventional hemostasis options fail.
In our systematic review, the overall CSR and TSR for the indication of GI hemorrhage was 86.0% and 96.8%, respectively. Surgical intervention for control of GI hemorrhage following OTSC placement was only required in 1.6% (21/1303) of patients.
Though infrequent, perforation is an established risk of any endoscopic procedure, with average rates from 1 in 2500 to 1 in 11000 esophagogastroduodenoscopy’s and 5.8 per 10000 for colonoscopy[94-96]. Advanced endoscopic interventions (including resection), have a higher risk of perforation than diagnostic procedures. Conventional management of acute iatrogenic perforation often necessitates surgical intervention; however, an effective and minimally invasive endoscopic approach to close these lesions during the index procedure is preferential to a higher-morbidity surgical intervention. Several endoscopic interventions have been utilized to manage perforations with varying degrees of success including: Self-expanding metal stents (SEMSs), TTS clips, endoscopic suturing, and OTSC[97]. SEMSs have been primarily used in the management of esophageal perforation; however, they carry the risk of migration and incomplete seal. TTS clips have limited ability to achieve complete closure of large defects and endoscopic suturing is limited by operator expertise, tedium and endoscope length in cases of perforation in the small bowel. Endoscopic suturing can also be challenging when managing defects in difficult locations such as gastric cardia, esophagus, duodenum, and proximal colon.
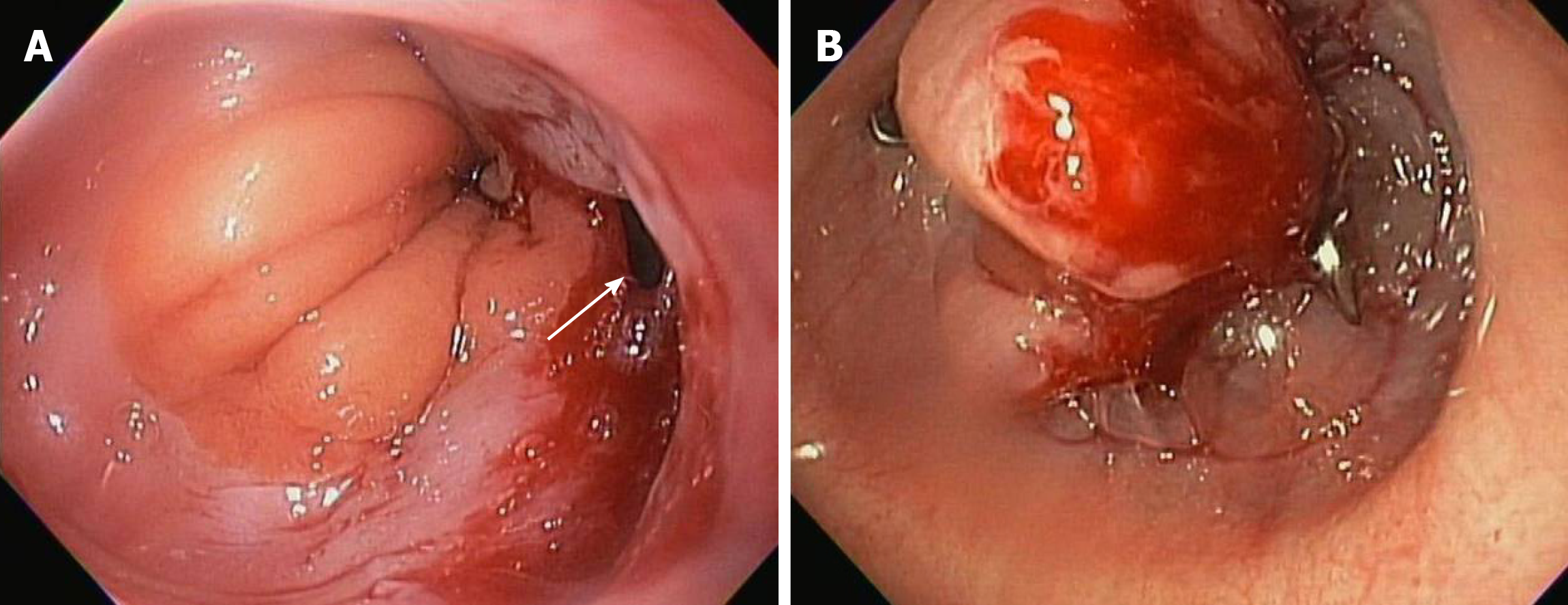
The European Society of GI Endoscopy currently recommends that endoscopic closure of iatrogenic perforations be considered during the index procedure[97]. OTSC is advantageous in this setting, as its ease of use, ability to close defects between 1-3 cm with a single clip application, and safety profile allow the endoscopist to effectively manage acute perforation immediately upon recognition (Figure 5)[97]. If the attempt to close perforation is delayed (> 72 h) or the defect is larger than 2 cm in diameter, endoscopic management is more likely to fail; however, the TG device can be utilized to approximate the edges of the defect for more effective closure with the OTSC, when dealing with larger defects (> 2 cm)[57,97]. Additionally, in cases of esophageal perforation, closure may be difficult with only suctioning the defect into the applicator cap (given the tangential orientation of the esophageal wall of to the endoscope). In this instance, the TG can help grasp the tissue to facilitate closure of the defect. Caution should be exercised while deploying the OTSC in difficult locations (e.g., gastro-esophageal junction, pylorus and the duodenal sweep) to avoid closing off the lumen entirely.
Honegger et al[43] reported on the efficacy of OTSC in a large cohort of patients (n = 72) with iatrogenic endoscopic perforations, with a stated CSR of 86.1%. Two patients experienced OTSC-related AEs, with one case of bleeding and one with a worsening of the index perforation. In a recent study, Wei et al[90] described the use of OTSC in patients with perforated peptic ulcer compared to a control group that was managed conventionally. The rate of clinical success in the OTSC group was 100% (n = 26/26) vs only 57.5% (n = 46/80) in controls. The requirement for surgical intervention in the OTSC cohort was significantly lower than controls (0% vs 30.0%, respectively, P < 0.001). No OTSC-related AEs were reported[90].
In our systematic review the overall CSR and TSR for the indication of perforation was 85.3% and 95.5%, respectively. Surgical intervention post-OTSC placement was required to achieve complete closure in 9.4% (n = 44/468) of patients.
Prior to the availability of OTSC, prophylactic closure of defects created by endoscopic resection of GI lesions would be managed with TTS clips. Prophylactic TTS clip closure following the resection of large (> 1 cm) proximal colonic lesions is an effective strategy that has reduced the incidence of post-procedure AEs (including post-polypectomy hemorrhage) and increased patient satisfaction[98-100]; however, TTS are limited by their diameter and often require a “suturing” technique involving the placement of multiple clips across the lesion. With the deployment of OTSC, a defect of 1-3 cm in diameter can be successfully closed utilizing a single clip[98].
The full-thickness resection device (FTRD; Ovesco Endoscopy AG, Tübingen, Germany) is now commercially available. This accessory combines the ability to complete resection and clipping with a single device. Aepli et al[46] reported the first clinical data in 2016 on the use of FTRD, demonstrating a CSR (n = 24 patients) of 87.5% and a post-OTSC AE rate of 12.5% (n = 4/24) with 3 post-procedure bleeding events and one post procedure perforation.
In our systematic review the overall CSR and TSR for the indication of defect closure following endoscopic resection was 92.8% and 95.9%, respectively. The necessity for post-OTSC surgical intervention was rare (n = 2/221; 0.9%).
GI fistulae are difficult to manage with either endoscopic or surgical interventions, likely due to the chronicity of the problem, fibrotic non healing tracts and prior treatment attempts making subsequent closure increasingly difficult. In addition, the underlying pathogenesis combined with a presentation of impaired nutritional status contribute to slow or non-healing of the fistula. Conventional management of GI fistulae focuses on control/prevention of infection, optimization of nutrition/ hydration, and limiting of fistula output. Surgical management can be attempted as a definitive therapy in lower-risk patients; however, patients with complex fistulae may be too medically frail for surgical intervention and/or those presenting with a small bowel fistula may not have enough remnant bowel to allow for further resection.
In recent years, endoscopy been considered as a possible primary therapy for the closure of GI fistulae[101]. Prior to the advent of OTSC, endoscopic treatment of GI fistulae had been attempted with TTS, absorbable loop snares or glues to varying degrees of success[102]. OTSC has potential in the management of GI fistulae (Figure 6), as the suction utilized in the clip application can create a more robust closure than TTS; however, definitive closure of a fistula relies on the complete grasping of involved tissue within the clipping device, which may be difficult when fibrotic tissue is present, as in most fistulae. High rates of clinical success for fistula closure have not yet been reported with OTSC. Haito-Chavez et al[50] reported the largest study of OTSC use in patients with fistulae (n = 91 patients) secondary to percutaneous endoscopic gastrostomy or jejunostomy tubes, post-bariatric surgery, malignancy-related, trauma, inflammatory bowel disease or diverticulitis. Deployment of the OTSC was successful in 89.4% of patients; however, clinical success at a median of 121 d was only 42.9%[50]. Other studies have reported similar CSR for fistula closure with OTSC[48]. Haito-Chavez et al[50] discuss the likelihood that fistulae with fibrotic and retracted rims were most associated with clinical failure, possibly related to the difficulty in properly targeting and suctioning the tissue during OTSC application. Fistulae smaller than 1 cm could be considered for closure with OTSC; however, in cases with a large fistula (> 1 cm) more than one clip could be applied and/or utilized in combination with endoscopic suturing with reinforced OTSC or glue to successfully achieve closure.
In our systematic review the overall CSR and TSR for the indication of fistulae was 55.8% and 92.8%, respectively. Surgical intervention post-OTSC placement was required in 7.6% (n = 47/622) of patients.
Conventional management for anastomotic leaks often follows a conservative approach of broad-spectrum antibiotics for lower-risk lesions and/or repeated surgical intervention for higher-risk lesions. The probability of a post-surgical anastomotic leak is higher in patients with a low serum albumin, longer operative time, higher intraoperative blood loss, positive resection margins or the presence of inflammatory bowel disease[103]. An effective minimally invasive endoscopic approach is preferable, as many of these patients may be too high-risk for additional surgical intervention.
Manta et al[42] presented the largest case series of patients (n = 76) with anastomotic leaks included in this review. Post-surgical leaks appeared in both the upper (n = 47) and lower (n = 29) GI tract. Overall clinical success was achieved in 80.3% of patients (83% and 75.9% for upper and lower GI leaks, respectively)[42].
In our systematic review the overall CSR and TSR for the indication of anastomotic leak closure was 72.6% and 86.7%, respectively. Surgical intervention post-OTSC placement was required in 7.4% (29/391) of patients.
GI stenting (most often for tumor palliation) though effective in immediate symptomatic relief, is often plagued by stent migration, especially in the case of fully covered stents[104]. The availability of SEMSs has reduced the risk of migration; however, the potential still exists[105]. OTSC can be used to anchor SEMS to mitigate the risk of stent migration. Limited data exist on the application of OTSC in this setting. The largest paper in the literature was presented by Mudumbi et al[16], demonstrating a high CSR (83%) in 12 patients who underwent OTSC fixation of SEMS, with no reported OTSC-related AEs. If it is necessary to remove a stent anchored by OTSC, the clip itself will need to be detached to do so, which is neither easy nor predictable. Traditionally, the only feasible method to remove the OTSC was with argon plasma coagulation; however, a novel device (remOVE system; Ovesco Endoscopy AG, Tubingen, Germany) has since been developed to effectively detach the OTSC[106,107].
In our systematic review the overall CSR and TSR for the indication of stent fixation was 80.0% and 100%, respectively; however, only 20 patients were included due to the paucity of data regarding OTSC for stent fixation in the literature. No patients required surgical intervention following OTSC placement or as a result of removal.
Sixty-four studies (n = 1942 patients) reported OTSC-related AE data (Table 4), with an overall rate of 2.1% (n = 40/1,942). These events included: “incorrect placement site” (n = 11/40; 27.5%), perforation (n = 9/40; 22.5%), bleeding (n = 10/40; 25%), and infection (n = 10/40; 25%). No deaths occurred as a result of OTSC use.
| Clinical success rate (%), (n/N) | Technical success rate (%), (n/N) | Post-over the scope clip surgical rate (%), (n/N) | |
| Fistula | 55.8 (347/622) | 92.8 (577/622) | 7.6 (47/622) |
| Bleeding | 86.0 (1120/1303) | 96.8 (1261/1303) | 1.6 (21/1303) |
| Perforation | 85.3 (399/468) | 95.5 (447/468) | 9.4 (44/468) |
| Leak | 72.6 (284/391) | 86.7 (339/391) | 7.4 (29/391) |
| ER | 92.8 (205/221) | 95.9 (212/221) | 0.9 (2/221) |
| Stent fixation | 80.0 (16/20) | 100 (20/20) | 0.0 (0/20) |
| Overall | 78.4 (2371/3025) | 94.4 (2856/3025) | 4.7 (143/3025) |
A perforation was defined as an AE if the OTSC: (1) Caused a de novo perforation, or (2) Worsened an already existing perforation that the OTSC was intended to close. “Incorrect placement site” was defined as the placement of the OTSC in a location other than the targeted defect and/or the disruption of nearby tissue/structures by the OTSC. For instance, Honegger et al[43] reported three cases of inadvertent OTSC deployment on the tongue during withdrawal of the endoscope and one case of OTSC deployment in the rectum causing a pseudopolyp formation resulting in a clinically significant obstruction. Raithel et al[14] reported a case of colonic perforation managed with OTSC resulting in fixation of the small bowel to the colon and subsequent rupture of the small bowel requiring surgical intervention. Khater et al[86] further described the potential of the OTSC to disrupt nearby tissue/structures reporting a case of rectosigmoid perforation that was effectively closed with OTSC; however, follow-up imaging studies demonstrated dilation of the urinary tract and ureter obstruction as a result of the ureter being suctioned into the application cap during clip deployment. Ultimately this patient required surgical intervention[86]. Such cases highlight the potential hazards and drawbacks related to the application of the OTSC clip, therefore careful consideration of surrounding anatomy should be entertained prior to OTSC deployment. Though the incorrect placement of OTSC can be a significant AE (due to difficulty in OTSC removal), the remOVE device is now available to detach the OTSC if placement of the clip is not satisfactory. Preliminary data suggest successful fragmentation of the OTSC with remOVE in 97.3% of cases, with minimal AEs (bleeding in 2.7% of patients, and superficial mucosal tearing in 1.4% of patients)[107].
To our knowledge, this systematic review represents the most comprehensive data (3025 cases over a period of 12 years; 2007-2019) of OTSC use across all GI indications. A high CSR (> 75%) was reported in the majority of clinical applications of OTSC. Our review confirms the efficacy of OTSC in preventing surgical intervention in most cases, as only 4.7% (n = 143/3025) of patients required salvage surgery, despite OTSC placement. OTSC can be considered for patients that are too high-risk for surgery but who can still tolerate endoscopy. OTSC facilitates effective endoscopic management of iatrogenic complications and known complex defects that previously may have only been amenable to surgical repair.
When each indication for OTSC placement is evaluated individually, there are clear disparities in CSRs for certain indications. A CSR of greater than 85% was observed in the management of GI hemorrhage, perforation and defect closure following endoscopic resection with OTSC; however, fistula closure was comparatively much less successful with a CSR of 55.8%. The lower efficacy of OTSC in fistula closure compared to other indications is thought to be multifactorial from the chronicity of the underlying problem and other variables discussed above that can make subsequent closure attempts challenging. Further innovation in technology and accessories can help close this gap in effectiveness across various indications and improve the effectiveness of OTSC in challenging scenarios.
In one of the earlier published articles on OTSC, Seebach et al[15] noted that OTSC has the potential to “spare the surgeon”. Our review strengthens this opinion as there was no indication for OTSC placement in which a rate of post-OTSC surgery was greater than 10%. Prior to the use of OTSC, surgical intervention would have been required for most of the patients included in this review. The rates of surgery, and the AEs, morbidity and mortality associated with it, will decrease for patients as OTSC becomes more integrated into routine endoscopic practices. Furthermore, patients who previously were deemed to be poor surgical candidates may now be able to be successfully managed with a less invasive and effective endoscopic approach.
The main limitation of this review is the level of available evidence related to OTSC use, as there is a paucity of RCTs or large multi-center analyses in the literature. The majority of articles include a relatively small sample size and/or are a summation of a single-center’s experience with OTSC use across multiple indications. In addition, our review lacks a large cohort of patients that underwent OTSC placement following endoscopic resection or for stent fixation. The potential for selection bias in pooling results from case series or single-center retrospective studies is acknowledged. Case series are often likely to underrepresent AEs and negative outcomes, as often authors are interested in adding positive results to the literature. Our review attempted to limit this bias by including studies with five or more patients. When isolating studies with a prospective design only (Table 5), a similar overall CSR and OTSC-related AE rate was demonstrated, suggesting that pooled retrospective data may be truly representative of the efficacy and safety of OTSC. The potential for lack of generalizability to a community setting may exist due to the likelihood that the majority of endoscopists currently utilizing OTSC in their practice are considered “experts” and/or performing some level of advanced endoscopic procedures.
| Ref. | Year | Type of study | Country | Patients (n) | Overall clinical success rate (%) | Follow-up (wk) | Adverse events, n (%) | ||||||
| Indications | Total | ||||||||||||
| Fistula | Bleeding | Perforation | Leak | ER3 | Stent fixation | ||||||||
| Maekawa et al[21] | 2015 | Prospective | Japan | 12 | - | - | - | - | 11/12 | - | 11/12 | NR | 0.0 |
| Voermans et al[24] | 2012 | Prospective Multi-center | Netherlands | 36 | - | - | 32/36 | - | - | - | 32/26 | 1-26 | 0.0 |
| Lee et al[26] | 2017 | Prospective Multi-center | Korea | 19 | 1/4 | - | 1/1 | 10/12 | 1/2 | - | 13/19 | 72 | 0.0 |
| Arezzo et al[28] | 2012 | Case series Prospective | Italy | 14 | - | - | - | 12/14 | - | - | 12/14 | 16 | 0.0 |
| Schlag et al[29] | 2013 | Prospective | Germany | 6 | - | - | 6/6 | - | - | - | 6/6 | 4-12 | 0.0 |
| Gubler et al [31] | 2012 | Case series Prospective | Switzerland | 14 | - | - | 12/14 | - | - | - | 12/14 | 4-48 | NR |
| Singhal et al[32] | 2014 | Case series Prospective | United States | 10 | 9/10 | - | - | - | - | - | 9/10 | 7 | 0.0 |
| Schmidt et al[4] | 2015 | Prospective Multi-center RCT | International1 | 24 | - | - | - | - | 18/24 | - | 18/24 | 4 | 2 (8.3) |
| Correia et al[36] | 2014 | Case series Prospective | Portugal | 6 | 4/5 | - | 1/1 | - | - | - | 5/6 | NR | 0.0 |
| Goenka et al[37] | 2017 | Prospective | India | 12 | 2/3 | 6/6 | 3/3 | - | - | - | 11/12 | 4-8 | 0.0 |
| Surace et al[38] | 2011 | Prospective | Italy | 19 | 14/19 | - | - | - | - | - | 14/19 | 32 | 1 (5.3) |
| Kochhar et al[39] | 2017 | Case series Prospective | United States | 12 | - | - | - | 8/12 | - | - | 8/12 | 60 | 1 (8.3) |
| Manta et al[40] | 2017 | Prospective | Italy | 76 | - | - | - | 61/76 | - | - | 61/76 | NR | 0.0 |
| Parodi et al[41] | 2010 | Prospective | Italy | 10 | 4/5 | - | 3/3 | 1/2 | - | - | 8/10 | NR | 0.0 |
| Sulz et al[52] | 2014 | Case series Prospective | Switzerland | 19 | 6/11 | 1/1 | - | 4/6 | - | 1/1 | 12/19 | NR | 0.0 |
| Magdeburg et al[53] | 2015 | Prospective | Germany | 43 | - | - | 42/43 | - | - | - | 42/43 | NR | 3 (7.0) |
| Keren et al[55] | 2014 | Case series Prospective | Israel | 26 | - | - | - | 21/26 | - | - | 21/26 | NR | 0.0 |
| Hagel et al[57] | 2012 | Case series Prospective | Germany | 17 | - | - | 11/17 | - | - | - | 11/17 | 4 | NR |
| Mangiafico et al[63] | 2017 | Case series Prospective | International2 | 7 | 7/7 | - | - | - | - | - | 7/7 | 2-8 | 0.0 |
| Schmdtt et al[4] | 2018 | Prospective RCT | International3 | 33 | - | 28/33 | - | - | - | - | 28/33 | 4 | 0.0 |
| Prosst et al[66] | 2015 | Prospective | Germany | 20 | 18/20 | - | - | - | - | - | 18/20 | 24 | 0.0 |
| Mizrahi et al[67] | 2016 | Prospective | United States | 51 | 6/17 | 3/4 | 3/4 | 12/24 | - | 1/2 | 25/51 | 48 | NR |
| Chan et al [75] | 2014 | Case series Prospective | China | 9 | - | 7/9 | - | - | - | - | 7/9 | 8 | NR |
| Keen et al[76] | 2019 | Prospective | United Kingdom | 59 | - | 55/59 | - | - | - | - | 55/59 | 4 | NR |
| Tashima et al[85] | 2017 | Prospective | Japan | 50 | - | - | - | - | 47/50 | - | 47/50 | 2 | 4 (8) |
| Kappelle et al[89] | 2018 | Prospective | Netherlands | 13 | - | - | - | - | 11/13 | - | 11/13 | 24 | 5 (38.4) |
| Total | 617 | 70.3% | 89.3% | 89.1% | 75.0% | 87.1% | 66.7% | 81.7% | - | 3.4% | |||
| 71/101 | 100/112 | 114/128 | 129/172 | 88/101 | 2/3 | 504/617 | - | 16/4674 | |||||
In conclusion, it is clear that the OTSC device represents a major advance in endoscopic practice and has enabled a “paradigm shift” in how we manage a variety of endoscopic challenges today. Our systematic review demonstrates that the OTSC system is a safe and effective endoscopic therapy to manage GI hemorrhage, perforation, anastomotic leaks, defects created by endoscopic resection, and for stent fixation; however, success in fistulae was limited. Further studies, including randomized controlled trials comparing OTSC with conventional and/or surgical therapies, are needed to determine which indication(s) are the most appropriate for its use and also to clarify the true AE rate, need for surgical salvage and any other technical aspects of OTSC use that may further clarify the role of OTSC in current and future endoscopic practice.
The over-the-scope-clip (OTSC) device has become widely utilized in endoscopic practice. Limited data exist evaluating the overall clinical success and adverse event (AE) rates of OTSC across gastrointestinal (GI) indications.
The key significance of this systematic review is to provide endoscopists with a real-world estimate of the efficacy and safety of OTSC in clinical practice.
The aim of this study was to determine the rates of clinical success (CSR), technical success (TSR), AE and post-OTSC (salvage) surgery rates.
A PubMed search was conducted for eligible articles describing the use of OTSC for any GI indication. Any article or case series reporting data for less than 5 total patients was excluded. Articles were included from January 1, 2007 to January 15, 2020. The following terms were used to perform the literature search: “over-the-scope-clip”, “OTSC”, “endoscopic fistula closure,” “over-the-scope clip bleeding”, “stent fixation”, and “endoscopic perforation closure.”
Eighty-five articles met inclusion criteria (n = 3025 patients). The overall CSR (inclusive of all indications) and TSR for OTSC placement was 78.4% (n = 2371/3025) and 94.4% (n = 2856/3025), respectively.
OTSCs are a novel advancement in endoscopic practice. They are safe and effective for use in GI hemorrhage, anastomotic leak, perforation, defects created by endoscopic resection and stent fixation; however, there is room for improvement in use for fistula closure.
Future large randomized control trials comparing OTSC with conventional and/or surgical interventions are needed to develop clinical guidelines for the most appropriate endoscopic application(s).
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: American Society for Gastrointestinal Endoscopy; and the American Gastroenterological Association.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chiu CC, Dohi O, Liu DL S-Editor: Yan JP L-Editor: A E-Editor: Qi LL
| 1. | Ovesco innovation in scope. OTSC System. [cited 27 January 2020]. Available from: https://ovesco.com/otsc-system/. [Cited in This Article: ] |
| 2. | Kirschniak A, Kratt T, Stüker D, Braun A, Schurr MO, Königsrainer A. A new endoscopic over-the-scope clip system for treatment of lesions and bleeding in the GI tract: first clinical experiences. Gastrointest Endosc. 2007;66:162-167. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 238] [Cited by in F6Publishing: 222] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 3. | Farnik H, Driller M, Kratt T, Schmidt C, Fähndrich M, Filmann N, Königsrainer A, Stallmach A, Heike M, Bechstein WO, Zeuzem S, Albert JG. Indication for 'Over the scope' (OTS)-clip vs. covered self-expanding metal stent (cSEMS) is unequal in upper gastrointestinal leakage: results from a retrospective head-to-head comparison. PLoS One. 2015;10:e0117483. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Schmidt A, Gölder S, Goetz M, Meining A, Lau J, von Delius S, Escher M, Hoffmann A, Wiest R, Messmann H, Kratt T, Walter B, Bettinger D, Caca K. Over-the-Scope Clips Are More Effective Than Standard Endoscopic Therapy for Patients With Recurrent Bleeding of Peptic Ulcers. Gastroenterology. 2018;155:674-686.e6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 88] [Cited by in F6Publishing: 88] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 5. | Manta R, Galloro G, Mangiavillano B, Conigliaro R, Pasquale L, Arezzo A, Masci E, Bassotti G, Frazzoni M. Over-the-scope clip (OTSC) represents an effective endoscopic treatment for acute GI bleeding after failure of conventional techniques. Surg Endosc. 2013;27:3162-3164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 77] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 6. | Skinner M, Gutierrez JP, Neumann H, Wilcox CM, Burski C, Mönkemüller K. Over-the-scope clip placement is effective rescue therapy for severe acute upper gastrointestinal bleeding. Endosc Int Open. 2014;2:E37-E40. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Iqbal CW, Cullinane DC, Schiller HJ, Sawyer MD, Zietlow SP, Farley DR. Surgical management and outcomes of 165 colonoscopic perforations from a single institution. Arch Surg. 2008;143:701-6; discussion 706-7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 140] [Cited by in F6Publishing: 149] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 8. | Gatto NM, Frucht H, Sundararajan V, Jacobson JS, Grann VR, Neugut AI. Risk of perforation after colonoscopy and sigmoidoscopy: a population-based study. J Natl Cancer Inst. 2003;95:230-236. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 354] [Cited by in F6Publishing: 325] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 9. | Fujiya M, Tanaka K, Dokoshi T, Tominaga M, Ueno N, Inaba Y, Ito T, Moriichi K, Kohgo Y. Efficacy and adverse events of EMR and endoscopic submucosal dissection for the treatment of colon neoplasms: a meta-analysis of studies comparing EMR and endoscopic submucosal dissection. Gastrointest Endosc. 2015;81:583-595. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 220] [Cited by in F6Publishing: 236] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 10. | Singhal S, Changela K, Papafragkakis H, Anand S, Krishnaiah M, Duddempudi S. Over the scope clip: technique and expanding clinical applications. J Clin Gastroenterol. 2013;47:749-756. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Schmidt A, Bauerfeind P, Gubler C, Damm M, Bauder M, Caca K. Endoscopic full-thickness resection in the colorectum with a novel over-the-scope device: first experience. Endoscopy. 2015;47:719-725. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 119] [Cited by in F6Publishing: 131] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 12. | Toshniwal J, Zabielski M, Fry LC, Mönkemüller K. Combination of the "bear claw" (over-the-scope-clip system) and fully covered stent for the treatment of post-operative anastomotic leak. Endoscopy. 2012;44 Suppl 2 UCTN:E288-E289. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47017] [Cited by in F6Publishing: 43253] [Article Influence: 2883.5] [Reference Citation Analysis (0)] |
| 14. | Raithel M, Albrecht H, Scheppach W, Farnbacher M, Haupt W, Hagel AF, Schellerer V, Vitali F, Neurath MF, Schneider HT. Outcome, comorbidity, hospitalization and 30-day mortality after closure of acute perforations and postoperative anastomotic leaks by the over-the-scope clip (OTSC) in an unselected cohort of patients. Surg Endosc. 2017;31:2411-2425. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 15. | Seebach L, Bauerfeind P, Gubler C. "Sparing the surgeon": clinical experience with over-the-scope clips for gastrointestinal perforation. Endoscopy. 2010;42:1108-1111. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 76] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 16. | Mudumbi S, Velazquez-Aviña J, Neumann H, Kyanam Kabir Baig KR, Mönkemüller K. Anchoring of self-expanding metal stents using the over-the-scope clip, and a technique for subsequent removal. Endoscopy. 2014;46:1106-1109. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 17. | Sandmann M, Heike M, Faehndrich M. Application of the OTSC system for the closure of fistulas, anastomosal leakages and perforations within the gastrointestinal tract. Z Gastroenterol. 2011;49:981-985. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Albert JG, Friedrich-Rust M, Woeste G, Strey C, Bechstein WO, Zeuzem S, Sarrazin C. Benefit of a clipping device in use in intestinal bleeding and intestinal leakage. Gastrointest Endosc. 2011;74:389-397. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 70] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 19. | Repici A, Arezzo A, De Caro G, Morino M, Pagano N, Rando G, Romeo F, Del Conte G, Danese S, Malesci A. Clinical experience with a new endoscopic over-the-scope clip system for use in the GI tract. Dig Liver Dis. 2009;41:406-410. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 20. | Donatelli G, Cereatti F, Dhumane P, Vergeau BM, Tuszynski T, Marie C, Dumont JL, Meduri B. Closure of gastrointestinal defects with Ovesco clip: long-term results and clinical implications. Therap Adv Gastroenterol. 2016;9:713-721. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 21. | Maekawa S, Nomura R, Murase T, Ann Y, Harada M. Complete closure of artificial gastric ulcer after endoscopic submucosal dissection by combined use of a single over-the-scope clip and through-the-scope clips (with videos). Surg Endosc. 2015;29:500-504. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Gautier M, Godeberge P, Ganansia R, Bozio G, Godart B, Bigard MA, Barthet M, Siproudhis L; Groupe de Recherche en Proctologie SNFCP France. Easy clip to treat anal fistula tracts: a word of caution. Int J Colorectal Dis. 2015;30:621-624. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 23. | Nishiyama N, Mori H, Kobara H, Rafiq K, Fujihara S, Kobayashi M, Oryu M, Masaki T. Efficacy and safety of over-the-scope clip: including complications after endoscopic submucosal dissection. World J Gastroenterol. 2013;19:2752-2760. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 101] [Cited by in F6Publishing: 106] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 24. | Voermans RP, Le Moine O, von Renteln D, Ponchon T, Giovannini M, Bruno M, Weusten B, Seewald S, Costamagna G, Deprez P, Fockens P; CLIPPER Study Group. Efficacy of endoscopic closure of acute perforations of the gastrointestinal tract. Clin Gastroenterol Hepatol. 2012;10:603-608. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 153] [Cited by in F6Publishing: 137] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 25. | Brandler J, Baruah A, Zeb M, Mehfooz A, Pophali P, Wong Kee Song L, AbuDayyeh B, Gostout C, Mara K, Dierkhising R, Buttar N. Efficacy of Over-the-Scope Clips in Management of High-Risk Gastrointestinal Bleeding. Clin Gastroenterol Hepatol. 2018;16:690-696.e1. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 26. | Lee HL, Cho JY, Cho JH, Park JJ, Kim CG, Kim SH, Han JH. Efficacy of the Over-the-Scope Clip System for Treatment of Gastrointestinal Fistulas, Leaks, and Perforations: A Korean Multi-Center Study. Clin Endosc. 2018;51:61-65. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 27. | Angsuwatcharakon P, Prueksapanich P, Kongkam P, Rattanachu-Ek T, Sottisuporn J, Rerknimitr R. Efficacy of the Ovesco Clip for Closure of Endoscope Related Perforations. Diagn Ther Endosc. 2016;2016:9371878. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 28. | Arezzo A, Verra M, Reddavid R, Cravero F, Bonino MA, Morino M. Efficacy of the over-the-scope clip (OTSC) for treatment of colorectal postsurgical leaks and fistulas. Surg Endosc. 2012;26:3330-3333. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 29. | Schlag C, Wilhelm D, von Delius S, Feussner H, Meining A. EndoResect study: endoscopic full-thickness resection of gastric subepithelial tumors. Endoscopy. 2013;45:4-11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 30. | Dişibeyaz S, Köksal AŞ, Parlak E, Torun S, Şaşmaz N. Endoscopic closure of gastrointestinal defects with an over-the-scope clip device. A case series and review of the literature. Clin Res Hepatol Gastroenterol. 2012;36:614-621. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 31. | Gubler C, Bauerfeind P. Endoscopic closure of iatrogenic gastrointestinal tract perforations with the over-the-scope clip. Digestion. 2012;85:302-307. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 32. | Singhal S, Changela K, Culliford A, Duddempudi S, Krishnaiah M, Anand S. Endoscopic closure of persistent gastrocutaneous fistulae, after percutaneous endoscopic gastrostomy (PEG) tube placement, using the over-the-scope-clip system. Therap Adv Gastroenterol. 2015;8:182-188. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 25] [Article Influence: 2.8] [Reference Citation Analysis (1)] |
| 33. | Mennigen R, Colombo-Benkmann M, Senninger N, Laukoetter M. Endoscopic closure of postoperative gastrointestinal leakages and fistulas with the Over-the-Scope Clip (OTSC). J Gastrointest Surg. 2013;17:1058-1065. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 70] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 34. | Fähndrich M, Sandmann M. Endoscopic full-thickness resection for gastrointestinal lesions using the over-the-scope clip system: a case series. Endoscopy. 2015;47:76-79. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 35. | Guo J, Liu Z, Sun S, Liu X, Wang S, Ge N, Wang G, Qi Y. Endoscopic full-thickness resection with defect closure using an over-the-scope clip for gastric subepithelial tumors originating from the muscularis propria. Surg Endosc. 2015;29:3356-3362. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 66] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 36. | Correia T, Amaro P, Oliveria A, Fernandesa A, Branquinhoa D, Nunesb A, Portelaa F, Sofiaa C. Endoscopic management of digestive leaks with the Over-The-Scope Clip: A retrospective study. GE Port J Gastroenterol. 2014;21:184-91. [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 37. | Goenka MK, Rai VK, Goenka U, Tiwary IK. Endoscopic Management of Gastrointestinal Leaks and Bleeding with the Over-the-Scope Clip: A Prospective Study. Clin Endosc. 2017;50:58-63. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 38. | Surace M, Mercky P, Demarquay JF, Gonzalez JM, Dumas R, Ah-Soune P, Vitton V, Grimaud J, Barthet M. Endoscopic management of GI fistulae with the over-the-scope clip system (with video). Gastrointest Endosc. 2011;74:1416-1419. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 76] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 39. | Kochhar GS, Shen B. Endoscopic treatment of leak at the tip of the "J" ileal pouch. Endosc Int Open. 2017;5:E64-E66. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 40. | Manta R, Caruso A, Cellini C, Sica M, Zullo A, Mirante VG, Bertani H, Frazzoni M, Mutignani M, Galloro G, Conigliaro R. Endoscopic management of patients with post-surgical leaks involving the gastrointestinal tract: A large case series. United European Gastroenterol J. 2016;4:770-777. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 41. | Parodi A, Repici A, Pedroni A, Blanchi S, Conio M. Endoscopic management of GI perforations with a new over-the-scope clip device (with videos). Gastrointest Endosc. 2010;72:881-886. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 135] [Cited by in F6Publishing: 145] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 42. | Manta R, Manno M, Bertani H, Barbera C, Pigò F, Mirante V, Longinotti E, Bassotti G, Conigliaro R. Endoscopic treatment of gastrointestinal fistulas using an over-the-scope clip (OTSC) device: case series from a tertiary referral center. Endoscopy. 2011;43:545-548. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 111] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 43. | Honegger C, Valli PV, Wiegand N, Bauerfeind P, Gubler C. Establishment of Over-The-Scope-Clips (OTSC®) in daily endoscopic routine. United European Gastroenterol J. 2017;5:247-254. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 44. | Manno M, Mangiafico S, Caruso A, Barbera C, Bertani H, Mirante VG, Pigò F, Amardeep K, Conigliaro R. First-line endoscopic treatment with OTSC in patients with high-risk non-variceal upper gastrointestinal bleeding: preliminary experience in 40 cases. Surg Endosc. 2016;30:2026-2029. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 45. | Richter-Schrag HJ, Glatz T, Walker C, Fischer A, Thimme R. First-line endoscopic treatment with over-the-scope clips significantly improves the primary failure and rebleeding rates in high-risk gastrointestinal bleeding: A single-center experience with 100 cases. World J Gastroenterol. 2016;22:9162-9171. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 47] [Cited by in F6Publishing: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 46. | Aepli PR. Full thickness resection device (FTRD): a novel tool for colonoscopic adenoma resection. First clinical experience from two tertiary referral centers in Switzerland. UEG Week 2016; October 15-19, 2016; Vienna, Austria. [Cited in This Article: ] |
| 47. | Meier B, Caca K, Schmidt A. Hybrid endoscopic mucosal resection and full-thickness resection: a new approach for resection of large non-lifting colorectal adenomas (with video). Surg Endosc. 2017;31:4268-4274. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 48. | Law R, Wong Kee Song LM, Irani S, Baron TH. Immediate technical and delayed clinical outcome of fistula closure using an over-the-scope clip device. Surg Endosc. 2015;29:1781-1786. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 49. | Jacobsen GR, Coker AM, Acosta G, Talamini MA, Savides TJ, Horgan S. Initial experience with an innovative endoscopic clipping system. Surg Technol Int. 2012;22:39-43. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 50. | Haito-Chavez Y, Law JK, Kratt T, Arezzo A, Verra M, Morino M, Sharaiha RZ, Poley JW, Kahaleh M, Thompson CC, Ryan MB, Choksi N, Elmunzer BJ, Gosain S, Goldberg EM, Modayil RJ, Stavropoulos SN, Schembre DB, DiMaio CJ, Chandrasekhara V, Hasan MK, Varadarajulu S, Hawes R, Gomez V, Woodward TA, Rubel-Cohen S, Fluxa F, Vleggaar FP, Akshintala VS, Raju GS, Khashab MA. International multicenter experience with an over-the-scope clipping device for endoscopic management of GI defects (with video). Gastrointest Endosc. 2014;80:610-622. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 204] [Cited by in F6Publishing: 190] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 51. | Winder JS, Kulaylat AN, Schubart JR, Hal HM, Pauli EM. Management of non-acute gastrointestinal defects using the over-the-scope clips (OTSCs): a retrospective single-institution experience. Surg Endosc. 2016;30:2251-2258. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 52. | Sulz MC, Bertolini R, Frei R, Semadeni GM, Borovicka J, Meyenberger C. Multipurpose use of the over-the-scope-clip system ("Bear claw") in the gastrointestinal tract: Swiss experience in a tertiary center. World J Gastroenterol. 2014;20:16287-16292. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 40] [Cited by in F6Publishing: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 53. | Magdeburg R, Kaehler G. Natural orifice transluminal endoscopic surgery in humans: feasibility and safety of transgastric closure using the OTSC system. Surg Endosc. 2016;30:73-77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 54. | Wedi E, Gonzalez S, Menke D, Kruse E, Matthes K, Hochberger J. One hundred and one over-the-scope-clip applications for severe gastrointestinal bleeding, leaks and fistulas. World J Gastroenterol. 2016;22:1844-1853. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 71] [Cited by in F6Publishing: 66] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 55. | Keren D, Eyal O, Sroka G, Rainis T, Raziel A, Sakran N, Goitein D, Matter I. Over-the-Scope Clip (OTSC) System for Sleeve Gastrectomy Leaks. Obes Surg. 2015;25:1358-1363. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 56. | Kobara H, Mori H, Fujihara S, Nishiyama N, Chiyo T, Yamada T, Fujiwara M, Okano K, Suzuki Y, Murota M, Ikeda Y, Oryu M, AboEllail M, Masaki T. Outcomes of gastrointestinal defect closure with an over-the-scope clip system in a multicenter experience: An analysis of a successful suction method. World J Gastroenterol. 2017;23:1645-1656. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 30] [Cited by in F6Publishing: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 57. | Hagel AF, Naegel A, Lindner AS, Kessler H, Matzel K, Dauth W, Neurath MF, Raithel M. Over-the-scope clip application yields a high rate of closure in gastrointestinal perforations and may reduce emergency surgery. J Gastrointest Surg. 2012;16:2132-2138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 58. | Nasa M, Sharma ZD, Choudhary NS, Patil G, Puri R, Sud R. Over-the-scope clip placement for closure of gastrointestinal fistula, postoperative leaks and refractory gastrointestinal bleed. Indian J Gastroenterol. 2016;35:361-365. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 59. | Al-Bawardy B, Rajan E, Wong Kee Song LM. Over-the-scope clip-assisted endoscopic full-thickness resection of epithelial and subepithelial GI lesions. Gastrointest Endosc. 2017;85:1087-1092. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 62] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 60. | Sarker S, Gutierrez JP, Council L, Brazelton JD, Kyanam Kabir Baig KR, Mönkemüller K. Over-the-scope clip-assisted method for resection of full-thickness submucosal lesions of the gastrointestinal tract. Endoscopy. 2014;46:758-761. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 75] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 61. | Mangiavillano B, Caruso A, Manta R, Di Mitri R, Arezzo A, Pagano N, Galloro G, Mocciaro F, Mutignani M, Luigiano C, Antonucci E, Conigliaro R, Masci E. Over-the-scope clips in the treatment of gastrointestinal tract iatrogenic perforation: A multicenter retrospective study and a classification of gastrointestinal tract perforations. World J Gastrointest Surg. 2016;8:315-320. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 34] [Cited by in F6Publishing: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 62. | Aiolfi A, Bona D, Siboni S, Pogliani L, Bonavina L. Over-the-scope endoclipping for foregut leaks and perforations. Eur Surg. 2014;46:155-9. [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 63. | Mangiafico S, Caruso A, Manta R, Grande G, Bertani H, Mirante V, Pigò F, Magnano L, Manno M, Conigliaro R. Over-the-scope clip closure for treatment of post-pancreaticogastrostomy pancreatic fistula: A case series. Dig Endosc. 2017;29:602-607. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 64. | Niland B, Brock A. Over-the-scope clip for endoscopic closure of gastrogastric fistulae. Surg Obes Relat Dis. 2017;13:15-20. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 65. | Heinrich H, Gubler C, Valli PV. Over-the-scope-clip closure of long lasting gastrocutaneous fistula after percutaneous endoscopic gastrostomy tube removal in immunocompromised patients: A single center case series. World J Gastrointest Endosc. 2017;9:85-90. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 17] [Cited by in F6Publishing: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 66. | Prosst RL, Joos AK, Ehni W, Bussen D, Herold A. Prospective pilot study of anorectal fistula closure with the OTSC Proctology. Colorectal Dis. 2015;17:81-86. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 67. | Mizrahi I, Eltawil R, Haim N, Chadi SA, Shen B, Erim T, DaSilva G, Wexner SD. The Clinical Utility of Over-the-Scope Clip for the Treatment of Gastrointestinal Defects. J Gastrointest Surg. 2016;20:1942-1949. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 68. | Kirschniak A, Subotova N, Zieker D, Königsrainer A, Kratt T. The Over-The-Scope Clip (OTSC) for the treatment of gastrointestinal bleeding, perforations, and fistulas. Surg Endosc. 2011;25:2901-2905. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 169] [Cited by in F6Publishing: 193] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 69. | Mennigen R, Laukötter M, Senninger N, Rijcken E. The OTSC(®) proctology clip system for the closure of refractory anal fistulas. Tech Coloproctol. 2015;19:241-246. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 70. | Wedi E, von Renteln D, Jung C, Tchoumak I, Roth V, Gonzales S, Leroy J, Hochberger J. Treatment of acute colonic diverticular bleeding in high risk patients, using an over-the-scope clip: a case series. Endoscopy. 2016;48:E383-E385. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 71. | Baron TH, Song LM, Ross A, Tokar JL, Irani S, Kozarek RA. Use of an over-the-scope clipping device: multicenter retrospective results of the first U.S. experience (with videos). Gastrointest Endosc. 2012;76:202-208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 137] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 72. | Lamberts R, Koch A, Binner C, Zachäus M, Knigge I, Bernhardt M, Halm U. Use of over-the-scope clips (OTSC) for hemostasis in gastrointestinal bleeding in patients under antithrombotic therapy. Endosc Int Open. 2017;5:E324-E330. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 73. | Soetikno R, Asokkumar R, Sim D, Sato T, Kaltenbach T. Use of the over-the-scope clip to treat massive bleeding at the transitional zone of the anal canal: a case series. Gastrointest Endosc. 2016;84:168-172. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 74. | Wedi E, von Renteln D, Gonzalez S, Tkachenko O, Jung C, Orkut S, Roth V, Tumay S, Hochberger J. Use of the over-the-scope-clip (OTSC) in non-variceal upper gastrointestinal bleeding in patients with severe cardiovascular comorbidities: a retrospective study. Endosc Int Open. 2017;5:E875-E882. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 75. | Chan SM, Chiu PW, Teoh AY, Lau JY. Use of the Over-The-Scope Clip for treatment of refractory upper gastrointestinal bleeding: a case series. Endoscopy. 2014;46:428-431. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 81] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 76. | Keen T, Ochieng A, Boger P, Hollingworth T, Patal P, Rahman I. ATH-01 The OVESCO over the scope clip (OTSC) reduces gastrointestinal haemorrhage re-bleeding rates–first UK series. Gut. 2019;68 Suppl 2:A1-A269. [Cited in This Article: ] |
| 77. | Horenkamp-Sonntag D, Liebentraut J, Engel S, Koop H. Tu1972 Efficacy and safety of over-the-scope clips (OTSC) application in the colon: Evidence generated from administrative data for an innovative endoscopic procedure. Gastrointest Endosc. 2019;89:AB636-AB637. [Cited in This Article: ] |
| 78. | Manta R, Mangiafico S, Zullo A, Bertani H, Caruso A, Grande G, Zito FP, Mangiavillano B, Pasquale L, Parodi A, Germanà B, Bassotti G, Monica F, Zilli M, Pisani A, Mutignani M, Conigliaro R, Galloro G. First-line endoscopic treatment with over-the-scope clips in patients with either upper or lower gastrointestinal bleeding: a multicenter study. Endosc Int Open. 2018;6:E1317-E1321. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 79. | Mercky P, Gonzalez JM, Aimore Bonin E, Emungania O, Brunet J, Grimaud JC, Barthet M. Usefulness of over-the-scope clipping system for closing digestive fistulas. Dig Endosc. 2015;27:18-24. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 79] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 80. | Mönkemüller K, Peter S, Toshniwal J, Popa D, Zabielski M, Stahl RD, Ramesh J, Wilcox CM. Multipurpose use of the 'bear claw' (over-the-scope-clip system) to treat endoluminal gastrointestinal disorders. Dig Endosc. 2014;26:350-357. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 82] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 81. | Bonino MVM, Salvai A. Efficacy of the over-the-scope-clip (OTSC) for treatment of colorectal postsurgical leaks and fistulas. Poster Department of Surgical Sciences; Italy: University of Torino; 2014. [Cited in This Article: ] |
| 82. | Christophorou D, Valats JC, Funakoshi N, Duflos C, Picot MC, Vedrenne B, Prat F, Bulois P, Branche J, Decoster S, Coron E, Charachon A, Pineton De Chambrun G, Nocca D, Bauret P, Blanc P. Endoscopic treatment of fistula after sleeve gastrectomy: results of a multicenter retrospective study. Endoscopy. 2015;47:988-996. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 83. | Lünse S, Höhn J, Glitsch A, Keßler W, Simon P, Heidecke CD, Schreiber A. Over-the-Scope Clip Closure of Pancreatico-Colonic Fistula Secondary to Acute or Chronic Pancreatitis: A Case Series. J Laparoendosc Adv Surg Tech A. 2019;29:1000-1004. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 84. | Mosquera-Klinger G, Torres-Rincón R, Jaime-Carvajal J. Endoscopic closure of gastrointestinal perforations and fistulas using the Ovesco Over-The-Scope Clip system at a tertiary care hospital center. Rev Gastroenterol Mex. 2019;84:263-266. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 85. | Tashima T, Ohata K, Sakai E, Misumi Y, Takita M, Minato Y, Matsuyama Y, Muramoto T, Satodate H, Horiuchi H, Matsuhashi N, Nonaka K, Ryozawa S. Efficacy of an over-the-scope clip for preventing adverse events after duodenal endoscopic submucosal dissection: a prospective interventional study. Endoscopy. 2018;50:487-496. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 68] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 86. | Khater S, Rahmi G, Perrod G, Samaha E, Benosman H, Abbes L, Malamut G, Cellier C. Over-the-scope clip (OTSC) reduces surgery rate in the management of iatrogenic gastrointestinal perforations. Endosc Int Open. 2017;5:E389-E394. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 87. | Asokkumar R, Soetikno R, Sanchez-Yague A, Kim Wei L, Salazar E, Ngu JH. Use of over-the-scope-clip (OTSC) improves outcomes of high-risk adverse outcome (HR-AO) non-variceal upper gastrointestinal bleeding (NVUGIB). Endosc Int Open. 2018;6:E789-E796. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 88. | Morrell DJ, Winder JS, Johri A, Docimo S, Juza RM, Witte SR, Alli VV, Pauli EM. Over-the-scope clip management of non-acute, full-thickness gastrointestinal defects. Surg Endosc. 2020;34:2690-2702. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 89. | Kappelle WFW, Backes Y, Valk GD, Moons LMG, Vleggaar FP. Endoscopic full-thickness resection of gastric and duodenal subepithelial lesions using a new, flat-based over-the-scope clip. Surg Endosc. 2018;32:2839-2846. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 90. | Wei JJ, Xie XP, Lian TT, Yang ZY, Pan YF, Lin ZL, Zheng GW, Zhuang ZH. Over-the-scope-clip applications for perforated peptic ulcer. Surg Endosc. 2019;33:4122-4127. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 91. | Gölder S, Neuhas L, Freuer D, Probst A, Ebigbo A, Braun G, Brueckner J, Stueckle J, Meier A, Messmann H. Over-the-scope clip in peptic ulcer bleeding: clinical success in primary and secondary treatment and factors associated with treatment failure. Endosc Int Open. 2019;7:E846-E854. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 92. | Wedi E, Fischer A, Hochberger J, Jung C, Orkut S, Richter-Schrag HJ. Multicenter evaluation of first-line endoscopic treatment with the OTSC in acute non-variceal upper gastrointestinal bleeding and comparison with the Rockall cohort: the FLETRock study. Surg Endosc. 2018;32:307-314. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 93. | Hwang JH, Fisher DA, Ben-Menachem T, Chandrasekhara V, Chathadi K, Decker GA, Early DS, Evans JA, Fanelli RD, Foley K, Fukami N, Jain R, Jue TL, Khan KM, Lightdale J, Malpas PM, Maple JT, Pasha S, Saltzman J, Sharaf R, Shergill AK, Dominitz JA, Cash BD; Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy. The role of endoscopy in the management of acute non-variceal upper GI bleeding. Gastrointest Endosc. 2012;75:1132-1138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 232] [Cited by in F6Publishing: 197] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 94. | Sieg A, Hachmoeller-Eisenbach U, Eisenbach T. Prospective evaluation of complications in outpatient GI endoscopy: a survey among German gastroenterologists. Gastrointest Endosc. 2001;53:620-627. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 210] [Cited by in F6Publishing: 202] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 95. | Quine MA, Bell GD, McCloy RF, Matthews HR. Prospective audit of perforation rates following upper gastrointestinal endoscopy in two regions of England. Br J Surg. 1995;82:530-533. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 111] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 96. | Kothari ST, Huang RJ, Shaukat A, Agrawal D, Buxbaum JL, Abbas Fehmi SM, Fishman DS, Gurudu SR, Khashab MA, Jamil LH, Jue TL, Law JK, Lee JK, Naveed M, Qumseya BJ, Sawhney MS, Thosani N, Yang J, DeWitt JM, Wani S; ASGE Standards of Practice Committee Chair. ASGE review of adverse events in colonoscopy. Gastrointest Endosc. 2019;90:863-876.e33. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 86] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 97. | Paspatis GA, Dumonceau JM, Barthet M, Meisner S, Repici A, Saunders BP, Vezakis A, Gonzalez JM, Turino SY, Tsiamoulos ZP, Fockens P, Hassan C. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2014;46:693-711. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 197] [Cited by in F6Publishing: 173] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 98. | Verlaan T, Voermans RP, van Berge Henegouwen MI, Bemelman WA, Fockens P. Endoscopic closure of acute perforations of the GI tract: a systematic review of the literature. Gastrointest Endosc. 2015;82:618-28.e5. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 67] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 99. | Zhang QS, Han B, Xu JH, Gao P, Shen YC. Clip closure of defect after endoscopic resection in patients with larger colorectal tumors decreased the adverse events. Gastrointest Endosc. 2015;82:904-909. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 93] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 100. | Liaquat H, Rohn E, Rex DK. Prophylactic clip closure reduced the risk of delayed postpolypectomy hemorrhage: experience in 277 clipped large sessile or flat colorectal lesions and 247 control lesions. Gastrointest Endosc. 2013;77:401-407. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 194] [Cited by in F6Publishing: 196] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 101. | Kumar N, Larsen MC, Thompson CC. Endoscopic Management of Gastrointestinal Fistulae. Gastroenterol Hepatol (NY). 2014;10:495-452. [PubMed] [Cited in This Article: ] |
| 102. | Ashkenazi I, Turégano-Fuentes F, Olsha O, Alfici R. Treatment Options in Gastrointestinal Cutaneous Fistulas. Surg J (N Y). 2017;3:e25-e31. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 103. | Telem DA, Chin EH, Nguyen SQ, Divino CM. Risk factors for anastomotic leak following colorectal surgery: a case-control study. Arch Surg. 2010;145:371-6; discussion 376. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 146] [Cited by in F6Publishing: 150] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 104. | Cusumano A, Ruol A, Segalin A, Norberto L, Baessato M, Tiso E, Peracchia A. Push-through intubation: effective palliation in 409 patients with cancer of the esophagus and cardia. Ann Thorac Surg. 1992;53:1010-1014. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 42] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 105. | Schumacher B, Lübke H, Frieling T, Haussinger D, Niederau C. Palliative treatment of malignant esophageal stenosis: experience with plastic versus metal stents. Hepatogastroenterology. 1998;45:755-760. [PubMed] [Cited in This Article: ] |
| 106. | Kapadia S, Nagula S, Kumta NA. Argon plasma coagulation for successful fragmentation and removal of an over-the-scope clip. Dig Endosc. 2017;29:820-821. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 107. | Caputo A, Schmidt A, Caca K, Bauerfeind P, Schostek S, Ho CN, Gottwald T, Schurr MO. Efficacy and safety of the remOVE System for OTSC® and FTRD® clip removal: data from a PMCF analysis. Minim Invasive Ther Allied Technol. 2018;27:138-142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |