Changes of center of rotation and femoral offset in total hip arthroplasty
Introduction
During single-leg standing the body weight is counterbalanced by the abductor muscles strength (1). Any variation in the hip joint center of rotation (COR) after total hip arthroplasty (THA) influences the lever arm and tension of the abductor muscles as well as the lever arm of the body weight, and thus the force required by the muscles to balance the pelvis. Medialization of COR with reduced lever arm of the body weight positively affects hip function (2) and has been associated with increased survival of THA (3-6). Also, the height of COR determines the tension of the abductor muscles (7), and superior and lateral relocation after THA has been connected with an increased rate of aseptic loosening (8,9). Therefore medialization of the cup with a respective increase in femoral offset has been advocated (10,11). However, medialization of the COR in THA may have negative effects on joint reaction forces, and may cause bone loss and changes in proprioception.
Increased femoral offset improves the hip abductor strength, and, thereby, reduces limping and the patients need of crutches (12-16). It also increases hip range of motion (10,17,18) and reduces the risk of dislocation and polyethylene wear (19-21). Correspondingly, patients with reduced femoral offset perform lower on functional tests (22,23). For some reason, however, it seems that patients with a low femoral offset experience the greatest improvement on pain scores after THA (24).
Thus, we have performed a prospective radiological study in patients receiving an uncemented THA to address the controversies:
- How do we manage to preserve the hip COR;
- How do we manage to preserve femoral and global offset;
- How are femoral, acetabular and global offsets correlated.
Methods
Patients
The study was not interventional, the patients followed ordinary routines and they could not be identified. Specific ethics approval therefore was not needed. It was prospectively performed in 100 patients (hips) who underwent primary THA with an uncemented prosthesis in accordance with the ethical standards of the 1975 Declaration of Helsinki as revised in 2008. The reasons for THA were primary osteoarthritis (n=63) and developmental dysplasia of the hip (n=10). We followed our ordinary practice, so there was no need for patient consent. We excluded 27 patients who suffered from distorted anatomy like developmental dysplasia of the hip (n=19), Calve-Legg-Perthes disease (n=4), avascular necrosis of the hip (n=2 and protrusion of the acetabulum (n=2). The following 73 patients to be included: 40 were females and 33 were males with a mean age of 64 years (range, 35–90 years). We intended a descriptive analysis, so we did not perform power calculations for statistics.
Four senior surgeons at our hospital operated the patients with a lateral approach. In all patients we used an uncemented prosthesis with a porous coated hemispherical press fit cup (Trilogy, Zimmer, Warsaw, USA) and a hydroxyapatite coated straight and rectangular press fit stem (Corail, DePuy, Saint Priest, France). The stem had a standard neck with modular lengths. The cup was inserted first, and then the stem. We used cup sizes from 48 to 60 and stem sizes from 9 to 14. As a standard we aimed to obtain femoral anteversion of 10 to 30°, acetabular anteversion of 10 to 30° and a combined anteversion of 25 to 55°. Cup position was obtained with the aid of an acetabular cup impactor-positioner provided with the implant manufacturer. Stem position was obtained with the knee flexed 90° and the leg as the reference for anteversion. In all cases we used elevated liners to provide optimal femoral head coverage and we used a ceramic head with diameter of 28 mm.
Methods of assessment
All radiological examinations were performed at the same radiological center. We used a standardized format for anterior-posterior (AP) radiographs of the pelvis with the patients in the supine position with the lower limbs parallel with each other as the patella was pointing frontally. We considered radiographs to be standardized if there were symmetric appearances of the obturator foramina and the tip of the coccyx pointed toward the symphysis pubis (25). Two reference lines were used to establish the body axis; one inter-ischial line and one vertical body line drawn perpendicular to the inter-ischial line through the centre of pubic symphysis (Figure 1). With help of PACS circles superimposed on the femoral head and the acetabular border, the best fitting circle was used to determine the femoral head COR and the rim of the acetabulum, respectively.
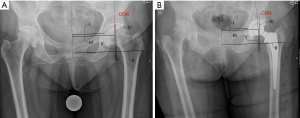
Preoperatively and postoperatively we measured five variables of biomechanical interest: (I) Distance between vertical midline—medial rim of acetabulum. (II) Distance between vertical midline proximal lateral femoral cortex (global offset). The end of the proximal lateral femoral cortex is defined as where cortical bone thickening ends beneath the trochanter area of the femoral metaphysis. (III) Distance between vertical midline and COR (acetabular offset). II subtracting III gives femoral offset. (IV) Distance between horizontal line and roof of acetabulum. (V) Distance between horizontal line and COR.
Statistical analysis
The distances were automatically calculated in PACS. Measurements were done twice and the mean value used in our data. Image magnification was accounted for by measuring the size of a metal ball with a known diameter. In a previous study we found this method to be applicable with intraclass correlation coefficient above 0.98 for all measurements (26). As there are sparse relevant data in the literature and our data are presented descriptively rather than statistically, we did not perform power analyses before the study. Data are expressed by mean ± standard deviations (SD), and we calculated Pearsons correlation coefficient (r). P value equal 0.05 or smaller was considered significant. For statistical analysis the SPSSTM software of the 12th version was used.
Results
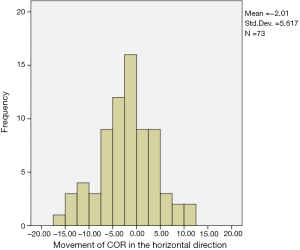
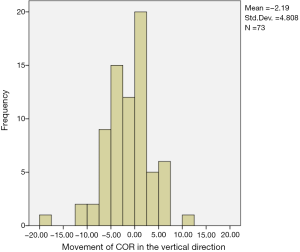
The changes of COR in horizontal direction (acetabular offset) ranged from −15 to +11 mm with a mean of −2.0±5.6 mm (Figure 2). In 20 of 73 cases there was a medial shift of COR by more than 5.0 mm, and in 7 cases there was a lateral shift by more than 5.0 mm. The changes of COR in the vertical direction ranged from 18 mm in proximal direction to 11 mm in distal direction with a mean of 1.3±4.8 mm in proximal direction (Figure 3). In 14 cases COR was moved more than 5.0 mm proximally, and in 6 cases it was moved more than 5.0 mm in distal direction.
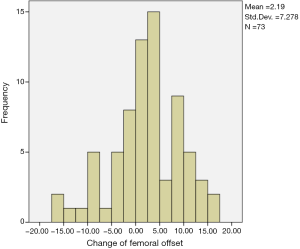
The change of femoral offset ranged from −17 to +17 mm with a mean of +2.2±7.3 mm (Figure 4). In 10 cases the femoral offset was reduced by more than 5.0 mm, and in 22 cases the femoral offset was increased by more than 5.0 mm.
The change in global offset ranged from −29 to +18 mm with a mean of +0.2±9.1 mm. In 17 cases global offset was reduced by more than 5.0 mm, and in 22 cases the global offset was increased by more than 5.0 mm.
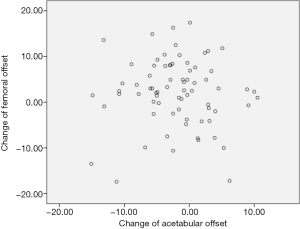
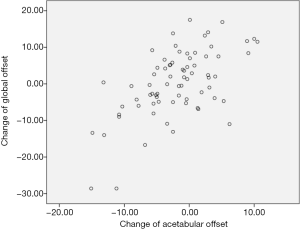
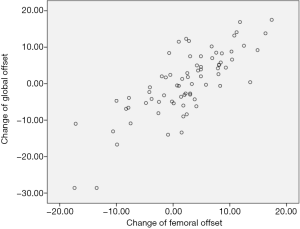
The correlation between changes in acetabular and femoral offset was not significant (r=−0.027, P=0.822), while the correlation between changes in acetabular and global offset (r=0.598, P<0.001), and the correlations between changes in femoral and global offset (r=0.786, P<0.001) were significant (Figures 5-7 respectively).
The postoperative course was uneventful in all patients, and at follow-up at 12 months they all had gluteal stability as evaluated by clinical testing (Trendelenburg sign).
Discussion
In this study we addressed the controversy how we manage to preserve the COR to the anatomic position with an uncemented total hip prosthesis implanted with free hand technique. In the literature there is agreement that an optimal reconstruction of COR in THA is within 5 mm from the anatomic location (8,27,28). We found that in 40 of 73 patients (hips) the COR was preserved within 5 mm from the preoperative anatomy. In all except one case with acetabular reaming of more than 10 mm in medial or proximal direction, COR was relocated more than 10 mm medially of proximally to the anatomic location. This finding supports the logical conclusion that the degree of acetabular reaming affects relocation of COR.
There are limitations to our study: it was restricted to patients with a well-defined femoral head and acetabular cavity. In patients with a deranged hip joint, relocation of the acetabular cavity can be necessary, and consequently the relocation of COR in a medial and/or superior direction can be even larger. Second, we relied on proper standardization of radiographs and measurement techniques, but radiographic interpretation relies heavily on the clinicians experience with reading radiographs. To minimize shortcomings, we calibrated with a ball of known size, and in a previous study this method proved to have high reliability and agreement of both within the same observer and between observers (26). Third, frontal X-rays only represent two-dimensional change of distances between the object of interest. When measuring the change of femoral offset, the possible change of femoral neck version might be a confounder (28). We did not measure the femoral neck angles, but compared the physiological femoral offset with the patella facing frontally.
In our series femoral offset was preserved within 5 mm in 34 cases. The optimal outcome in terms of stress has been observed when COR is medialized, but with an equivalent increase in femoral offset to restore global offset. This was obtained in 15 of our cases. Medialization of the cup decreases stress on the head-cup interface and on the abductor muscles (10,11). On the other hand, any increase of femoral and global offset significantly increases the length and the tension in the anterior bundles of the abductor muscles, and an increased expression of pain has been linked to increased femoral offset (27). The contribution of an offset increase is larger in a patient with little femoral torsion. Large femoral antetorsion and an increased femoral offset move the insertion of the abductor muscles on the greater trochanter more posteriorly and less laterally compared with a patient with little femoral antetorsion (29). Due to this a shift of femoral offset has been questioned. At least it seems that the effect of cup medialization is of less clinical importance than previously assumed.
A fair correlation was found between the changes of acetabular and global offset, and a better between femoral and global offset. This underlines that the surgeon has a greater influence on the femoral offset than the acetabular offset (8). The use of computer navigation may help to orientate the acetabular component in THA (30). Robotic computerized instrumentation that guides bone preparation and cup implantation was studied in 43 hips, and robotic instrumentation achieved precision of COR in 82% (31). However, the authors did not report how this affected offsets or clinical outcome.
Conclusions
In our study of the free hand technique, 40 patients (55%) had COR and 34 patients (47%) had femoral offset preserved within 5.0 mm limits after THA. Twenty-three patients (32%) had both their values of COR and femoral offset preserved within the preoperative 5.0 mm limits, as 15 patients (21%) had both their COR and femoral offset changed outside 5.0 mm limits. While a correlation was found between the changes of femoral and global offset, there was no correlation between the changes of acetabular and femoral offset that would have conserved the global offset. The variations had no influence on the function of the hip, but our results indicate a potential for better restoring the location of COR and femoral offset when planning and implanting an uncemented THA. The clinical consequences are, however, unknown.
Acknowledgements
None.
Footnote
Conflict of Interests: The authors have no conflicts of interest to declare.
References
- Lecerf G, Fessy MH, Philippot R, et al. Femoral offset: anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop Traumatol Surg Res 2009;95:210-9. [PubMed]
- Frain P. New geometric theory on the varization of the hip. Rev Chir Orthop Reparatrice Appar Mot 1978;64:563-8. [PubMed]
- Yoder SA, Brand RA, Pedersen DR, et al. Total hip acetabular component position affects component loosening rates. Clin Orthop Relat Res 1988.79-87. [PubMed]
- Callaghan JJ, Salvati EA, Pellicci PM, et al. Results of revision for mechanical failure after cemented total hip replacement, 1979 to 1982. A two to five-year follow-up. J Bone Joint Surg Am 1985;67:1074-85. [PubMed]
- Baghdadi YM, Larson AN, Sierra RJ. Restoration of the hip center during THA performed for protrusio acetabuli is associated with better implant survival. Clin Orthop Relat Res 2013;471:3251-9. [PubMed]
- Abolghasemian M, Samiezadeh S, Jafari D, et al. Displacement of the hip center of rotation after arthroplasty of Crowe III and IV dysplasia: a radiological and biomechanical study. J Arthroplasty 2013;28:1031-5. [PubMed]
- Delp SL, Wixson RL, Komattu AV, et al. How superior placement of the joint center in hip arthroplasty affects the abductor muscles. Clin Orthop Relat Res 1996.137-46. [PubMed]
- Liebs TR, Nasser L, Herzberg W, et al. The influence of femoral offset on health-related quality of life after total hip replacement. Bone Joint J 2014;96-B:36-42. [PubMed]
- Hirakawa K, Mitsugi N, Koshino T, et al. Effect of acetabular cup position and orientation in cemented total hip arthroplasty. Clin Orthop Relat Res 2001.135-42. [PubMed]
- Asayama I, Naito M, Fujisawa M, et al. Relationship between radiographic measurements of reconstructed hip joint position and the Trendelenburg sign. J Arthroplasty 2002;17:747-51. [PubMed]
- Krishnan SP, Carrington RW, Mohiyaddin S, et al. Common misconceptions of normal hip joint relations on pelvic radiographs. J Arthroplasty 2006;21:409-12. [PubMed]
- Devane P, Home G, Winemaker M, et al. The effect of restoring femoral offset during THR on 3D volumetric wear. J Bone Joint Surg (Br) 1997;79:385.
- Ramaniraka NA, Rakotomanana LR, Rubin PJ, et al. Noncemented total hip arthroplasty: influence of extramedullary parameters on initial implant stability and on bone-implant interface stresses. Rev Chir Orthop Reparatrice Appar Mot 2000;86:590-7. [PubMed]
- Bourne RB, Rorabeck CH. Soft tissue balancing: the hip. J Arthroplasty 2002;17:17-22. [PubMed]
- Yamaguchi T, Naito M, Asayama I, et al. Total hip arthroplasty: the relationship between posterolateral reconstruction, abductor muscle strength, and femoral offset. J Orthop Surg (Hong Kong) 2004;12:164-7. [PubMed]
- Bachour F, Marchetti E, Bocquet D, et al. Radiographic preoperative templating of extra-offset cemented THA implants: how reliable is it and how does it affect survival? Orthop Traumatol Surg Res 2010;96:760-8. [PubMed]
- Dolhain P, Tsigaras H, Bourne RB, et al. The effectiveness of dual offset stems in restoring offset during total hip replacement. Acta Orthop Belg 2002;68:490-9. [PubMed]
- Charles MN, Bourne RB, Davey JR, et al. Soft-tissue balancing of the hip: the role of femoral offset restoration. Instr Course Lect 2005;54:131-41. [PubMed]
- Ebied A, Hoad-Reddick DA, Raut V. Medium-term results of the Charnley low-offset femoral stem. J Bone Joint Surg Br 2005;87:916-20. [PubMed]
- Girard J, Touraine D, Soenen M, et al. Measurement of head penetration on digitalized radiographs: reproducibility and accuracy. Rev Chir Orthop Reparatrice Appar Mot 2005;91:137-42. [PubMed]
- Debarge R, Lustig S, Neyret P, et al. Confrontation of the radiographic preoperative planning with the postoperative data for uncemented total hip arthroplasty. Rev Chir Orthop Reparatrice Appar Mot 2008;94:368-75. [PubMed]
- Wegner A, Kauther MD, Landgraeber S, et al. Fixation method does not affect restoration of rotation center in hip replacements: a single-site retrospective study. J Orthop Surg Res 2012;7:25. [PubMed]
- Asayama I, Chamnongkich S, Simpson KJ, et al. Reconstructed hip joint position and abductor muscle strength after total hip arthroplasty. J Arthroplasty 2005;20:414-20. [PubMed]
- Woolson ST, Hartford JM, Sawyer A. Results of a method of leg-length equalization for patients undergoing primary total hip replacement. J Arthroplasty 1999;14:159-64. [PubMed]
- Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res 2003.241-8. [PubMed]
- Bjarnason JA, Pripp AH, Reikeras O. Reliability of measures used in radiographic evaluation of the adult hip. Skeletal Radiol 2015;44:935-9. [PubMed]
- Cassidy KA, Noticewala MS, Macaulay W, et al. Effect of femoral offset on pain and function after total hip arthroplasty. J Arthroplasty 2012;27:1863-9. [PubMed]
- Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty 2002;17:282-8. [PubMed]
- Terrier A, Levrero Florencio F, Rüdiger HA. Benefit of cup medialization in total hip arthroplasty is associated with femoral anatomy. Clin Orthop Relat Res 2014;472:3159-65. [PubMed]
- Honl M, Schwieger K, Salineros M, et al. Orientation of the acetabular component. A comparison of five navigation systems with conventional surgical technique. J Bone Joint Surg Br 2006;88:1401-5. [PubMed]
- Kanawade V, Dorr LD, Banks SA, et al. Precision of robotic guided instrumentation for acetabular component positioning. J Arthroplasty 2015;30:392-7. [PubMed]


