- Department of Neurosurgery, Fundación Santafe de Bogota University Hospital, Bogotá, Colombia
- Department of Radiology, Division of Neuroradiology, Fundación Santafe de Bogota University Hospital, Bogotá, Colombia
Correspondence Address:
Diego Fernando Gomez
Department of Radiology, Division of Neuroradiology, Fundación Santafe de Bogota University Hospital, Bogotá, Colombia
DOI:10.4103/2152-7806.177894
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Gomez DF, Mejia JA, Murcia DJ, Useche N. Isolated giant cerebral varix – A diagnostic and therapeutic challenge: A case report. Surg Neurol Int 02-Mar-2016;7:
How to cite this URL: Gomez DF, Mejia JA, Murcia DJ, Useche N. Isolated giant cerebral varix – A diagnostic and therapeutic challenge: A case report. Surg Neurol Int 02-Mar-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/isolated-giant-cerebral-varix-a-diagnostic-and-therapeutic-challenge-a-case-report/
Abstract
Background:Isolated giant cerebral varix (IGV) is an uncommon vascular lesion that represents a diagnostic challenge and requires dynamic vascular studies for its characterization. The IGV is considered a benign, low-flow venous lesion with very low risk of bleeding that might cause secondary symptoms mainly due to compression of the adjacent parenchyma.
Case Description:A 12-year-old female patient with non-contributory medical history presented with headache for the last 2 months. Upon admission, her neurological examination was unremarkable. Magnetic resonance imaging (MRI) and computed tomography angiography (CTA) images demonstrated a large varicose dilation of the superficial Sylvian vein, located anterior to the left temporal pole, with no evidence of abnormal arteriovenous connections or tumoral lesions. This finding was considered incidental and unrelated to her symptoms. In this case, we considered that the combination of CTA and MRIs was enough to establish an accurate diagnosis, excluding the need to perform invasive imaging studies. Taking into account these considerations, the patient was managed with conservative treatment and has been followed up for 1 year, remaining asymptomatic.
Conclusion:Cerebral IGVs are rare vascular lesions that are treated conservatively when asymptomatic and surgically in the case of rupture or compression of adjacent structures. Given our observation of a high unlikelihood of vascular connections to arteries, and the information obtained with non-invasive imaging techniques such as CTA and MRI was enough to make a clinical decision and avoid the evaluation with invasive procedures.
Keywords: Arteriovenous malformation, cerebral varix, developmental venous anomaly, venous aneurysm
INTRODUCTION
Cerebral varices are frequently associated with other vascular abnormalities such as arteriovenous malformations (AVMs) and developmental venous anomalies (DVA). Their etiology is usually explained by an increase in venous drainage pressure.[
CASE REPORT
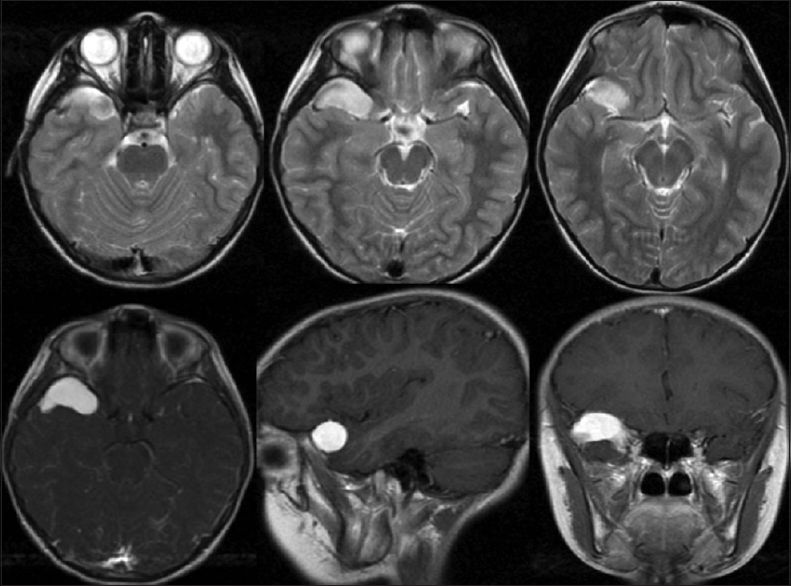
A 12-year-old female patient without relevant medical history complained of 2 months of right, unilateral, intermittent headache, associated with photophobia and hyperacusis that improved with the administration of analgesics. Upon admission, her neurological examination was unremarkable. Magnetic resonance images (MRIs) were performed, revealing an elongated well-defined extra-axial abnormality, located in the anterior aspect of the middle cranial fossa, showing high signal on T2-WI, intense homogeneous enhancement after intravenous contrast administration, and absence of flow voids or pulsation artifacts [
Figure 1
Cerebral magnetic resonance image. Top row: Axial T2-weighted images. Bottom row: Axial, sagittal, and coronal T1-weighted images with intravenous contrast. A well-defined elongated extra-axial lesion located anterior within the right middle cranial fossa, with slightly heterogeneous high signal intensity on T2-weighted images, and high homogeneous contrast enhancement
DISCUSSION
Cerebral varices are often associated with other vascular malformations, more frequently with AVMs and DVA.[
In most of the reported cases, isolated cerebral varices are subclinical entities discovered incidentally.[
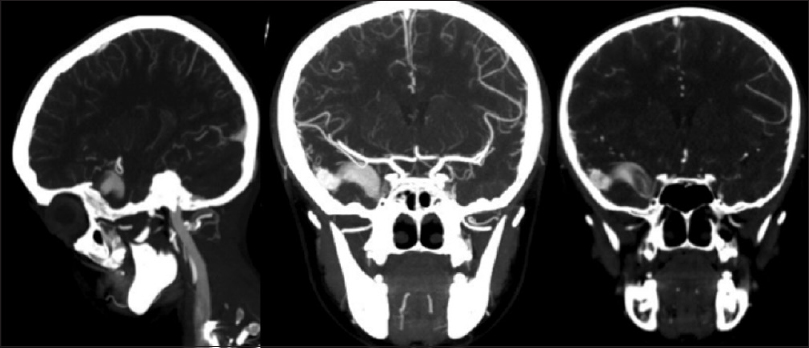
The diagnosis of an IGV is based on radiologic findings. On CT images of the brain without contrast, cerebral varices appear as extra-axial lesions with similar attenuation to the surrounding parenchyma. When the varix has contact with the skull, it causes bone remodeling, which allows ruling out the differential diagnosis of meningioma, which would cause hyperostosis in the adjacent bone.[
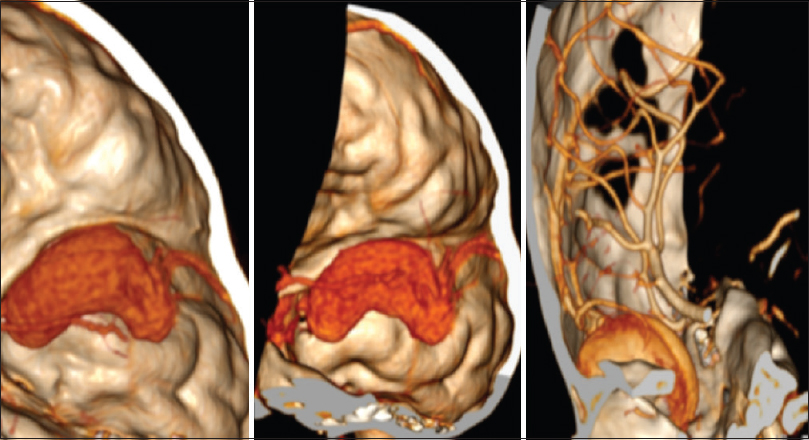
In our case, CTA images of the brain with three-dimensional reconstruction allowed the complete evaluation of the variceal lesion, and the determination of possible arterial pedicles, dilations, or arteriovenous communications that would suggest an AVM or cranial and spinal dural fistula. We were able to determine that the dilated vein was a right SSV, and we ruled out arterial communication or high-flow signs, concluding with the diagnosis of a giant cerebral varix. Invasive procedures such as conventional cerebral angiography were not considered due to patient age and the adequate evaluation of the lesion without invasive imaging techniques. CT imaging is seldom used in the diagnosis of this type of malformation, only found in a single case report by Asano et al. in which a subepicranial varix was diagnosed with CT imaging of the brain, showing a better diagnostic value than conventional cerebral angiography.
To the best of our knowledge, there is limited information in the literature regarding the definitive treatment of cerebral varices. Because these lesions are usually diagnosed incidentally without associated symptomatology, conservative treatment is generally considered the most appropriate course of action.[
CONCLUSION
Cerebral IGVs are extremely rare and, to the best of our knowledge, there is insufficient information available in the scientific literature. The incidence and the risk of rupture remain unclear, making this entity a diagnostic and therapeutic challenge. Currently, conservative management is the most appropriate treatment for asymptomatic lesions; however, in case of rupture or compression of adjacent neurovascular structures, endovascular or surgical treatment is warranted.
Given the MRI and CTA findings, the observation of a highly unlikelihood of abnormal connections to arterial feeders was sufficient to make a clinical decision and avoid interventional angiography procedures. We emphasize the use of noninvasive imaging techniques such as CTA and MRI for the diagnosis of this type of lesions, when AVMs and dural fistulas can be reliably excluded, avoiding the risk of invasive procedures particularly in children.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors thank to Gabriel A. Duran-Rehbein for his support.
References
1. Dietrich U, Forsting M. Isolated venous aneurysm (cerebral varicose vein) – A rare differential diagnosis. Rofo. 1998. 169: 441-3
2. Hamada J, Yano S, Kai Y, Koga K, Morioka M, Ishimaru Y. Histopathological study of venous aneurysms in patients with dural arteriovenous fistulas. J Neurosurg. 2000. 92: 1023-7
3. Hoell T, Hohaus C, Beier A, Holzhausen HJ, Meisel HJ. Cortical venous aneurysm isolated cerebral varix. Interv Neuroradiol. 2004. 10: 161-5
4. Kazumata K, Fujimoto S, Idosaka H, Kuroda S, Nunomura M, Houkin K. Multiple varices in the unilateral cerebral venous system. AJNR Am J Neuroradiol. 1999. 20: 1243-4
5. Kelly KJ, Rockwell BH, Raji MR, Altschuler EM, Martinez AJ. Isolated cerebral intraaxial varix. AJNR Am J Neuroradiol. 1995. 16: 1633-5
6. Lasjaunias P, Burrows P, Planet C. Developmental venous anomalies (DVA): The so-called venous angioma. Neurosurg Rev. 1986. 9: 233-42
7. Meyer JD, Baghai P, Latchaw RE. Cerebral varix and probable venous angioma: An unusual isolated anomaly. AJNR Am J Neuroradiol. 1983. 4: 85-7
8. Nishioka T, Kondo A, Nin K, Tashiro H, Ikai Y, Takahashi J. Solitary cerebral varix. Case report. Neurol Med Chir (Tokyo). 1990. 30: 904-7
9. Roda JM, Bencosme J, Isla A, Blázquez MG. Intraventricular varix causing hemorrhage. Case report. J Neurosurg. 1988. 68: 472-3
10. Shibata Y, Hyodo A, Tsuboi K, Yoshii Y, Nose T. Isolated cerebral varix with magnetic resonance imaging findings - Case report. Neurol Med Chir (Tokyo). 1991. 31: 156-8
11. Tanju S, Ustuner E, Deda H, Erden I. Cerebral varix simulating a meningioma: Use of 3D magnetic resonance venography for diagnosis. Curr Probl Diagn Radiol. 2006. 35: 258-60
12. Tyson GW, Jane JA, Strachan WE. Intracerebral hemorrhage due to ruptured venous aneurysm. Report of two cases. J Neurosurg. 1978. 49: 739-43
13. Uchino A, Hasuo K, Matsumoto S, Ikezaki K, Masuda K. Varix occurring with cerebral venous angioma: A case report and review of the literature. Neuroradiology. 1995. 37: 29-31
14. Valavanis A, Yasargil MG. The endovascular treatment of brain arteriovenous malformations. Adv Tech Stand Neurosurg. 1998. 24: 131-214
15. Viñuela F, Drake CG, Fox AJ, Pelz DM. Giant intracranial varices secondary to high-flow arteriovenous fistulae. J Neurosurg. 1987. 66: 198-203