Abstract
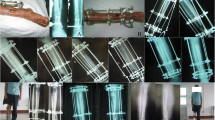
Infected nonunions of tibia pose many challenges to the treating surgeon and the patient. Challenges include recalcitrant infection, complex deformities, sclerotic bone ends, large bone gaps, shortening, and joint stiffness. They are easy to diagnose and difficult to treat. The ASAMI classification helps decide treatment. The nonunion severity score proposed by Calori measures many parameters to give a prognosis. The infection severity score uses simple clinical signs to grade severity of infection. This determines number of surgeries and allows choice of hardware, either external or internal for definitive treatment. Co-morbid factors such as smoking, diabetes, nonsteroidal anti-inflammatory drug use, and hypovitaminosis D influence the choice and duration of treatment. Thorough debridement is the mainstay of treatment. Removal of all necrotic bone and soft tissue is needed. Care is exercised in shaping bone ends. Internal fixation can help achieve union if infection was mild. Severe infections need external fixation use in a second stage. Compression at nonunion site achieves union. It can be combined with a corticotomy lengthening at a distant site for equalization. Soft tissue deficit has to be covered by flaps, either local or microvascular. Bone gaps are best filled with the reliable technique of bone transport. Regenerate bone may be formed proximally, distally, or at both sites. Acute compression can fill bone gaps and may need a fibular resection. Gradual reduction of bone gap happens with bone transport, without need for fibulectomy. When bone ends dock, union may be achieved by vertical or horizontal compression. Biological stimulus from iliac crest bone grafts, bone marrow aspirate injections, and platelet concentrates hasten union. Bone graft substitutes add volume to graft and help fill defects. Addition of rh-BMP-7 may help in healing albeit at a much higher cost. Regeneration may need stimulation and augmentation. Induced membrane technique is an alternative to bone transport to fill gaps. It needs large amounts of bone graft from iliac crest or femoral canal. This is an expensive method physiologically and economically. Infection can resorb the graft and cause failure of treatment. It can be done in select cases after thorough eradication of infection. Patience and perseverance are needed for successful resolution of infection and achieving union.
Similar content being viewed by others
References
Keating JF, Simpson AH, Robinson CM. The management of fractures with bone loss. J Bone Joint Surg Br. 2005 Feb; 87(2):142–50.
Bose D, Kugan R, Stubbs D, McNally M. Management of infected nonunion of the long bones by a multidisciplinary team. Bone Joint J 2015;97-B: 814–7.
Dendrinos GK, Kontos S, Lyritsis E. Use of the Ilizarov technique for treatment of nonunion of the tibia associated with infection. J Bone Joint Surg Am 1995;77:835–46.
Mora R, Pedrotti L, Bertani B, Quattrini F. Treatment of infected nonunions. In: Mora R, editor. Nonunion of the Long Bones: Diagnosis and Treatment with Compression-Distraction Techniques. New York: Springer; 2006. p. 199–223.
Borzunov DY, Balaev PI, Subramanyam KN. Reconstruction by bone transport after resection of benign tumors of tibia: A retrospective study of 38 patients. Indian J Orthop 2015;49:516–22.
Giannikas KA, Maganaris CN, Karski MT, Twigg P, Wilkes RA, Buckley JG. Functional outcome following bone transport reconstruction of distal tibial defects. J Bone Joint Surg Am 2005;87:145–52.
Aronson J. Limb-lengthening, skeletal reconstruction, and bone transport with the Ilizarov method. J Bone Joint Surg Am 1997;79:1243–58.
Iacobellis C, Berizzi A, Aldegheri R. Bone transport using the Ilizarov method: A review of complications in 100 consecutive cases. Strategies Trauma Limb Reconstr 2010;5:17–22.
Shapiro CN, Tokars JI, Chamberland ME. Use of the hepatitis-B vaccine and infection with hepatitis B and C among orthopaedic surgeons. The American Academy of Orthopaedic Surgeons Serosurvey Study Committee. J Bone Joint Surg Am 1996;78:1791–800.
Wijesekera MP, Graham SM, Lalloo DG, Simpson H, Harrison WJ. Fracture management in HIV positive individuals: A systematic review. Int Orthop 2016;40:2429–45.
Javidan P, Walker RH. Take care with type C: Serious considerations in the selection of patients with hepatitis C for total joint arthroplasty. J Bone Joint Surg Am 2015;97:e77.
Calori GM, Phillips M, Jeetle S, Tagliabue L, Giannoudis PV. Classification of nonunion: Need for a new scoring system? Injury 2008;39 Suppl 2:S59–63.
Chaudhary Milind M. Infected gap nonunions of femur. In: Kulkarni GS, Babhulkar S, editors. In Guidelines in Fracture Management, Nonunion in Long Bone II. Ch. 25. Noida: Thieme Publisher; 2016. p. 309–24.
Calhoun JH. Optimal timing of operative debridement: A known unknown: Commentary on an article by Mara L. Schenker, MD, et al.: “Does timing to operative debridement affect infectious complications in open long-bone fractures? A systematic review”. J Bone Joint Surg Am 2012;94:e90.
Schenker ML, Yannascoli S, Baldwin KD, Ahn J, Mehta S. Does timing to operative debridement affect infectious complications in open long-bone fractures? A systematic review. J Bone Joint Surg Am 2012;94:1057–64.
Lowenberg DW, Buntic RF, Buncke GM, Parrett BM. Long term results and costs of muscle flap coverage with Ilizarov bone transport in lower limb salvage. J Orthop Trauma 2013;27:576–81.
Graves DT, Alblowi J, Paglia DN, O’Connor JP, Lin S. Impact of Diabetes on Fracture Healing. J Exp Clin Med 2011;3:(1)3–8.
Flouzat-Lachaniette CH, Heyberger C, Bouthors C, Roubineau F, Chevallier N, Rouard H, Herigou P. Osteogenic progenitors in bone marrow aspirates have clinical potential for tibial nonunions healing in diabetic patients. International Orthopaedics (SICOT) 2016;40:1375–1379.
Varecka T.F., Wiesner L. The influence of hemorrhagic anemia on fracture healing. Orthopaedic Proceedings 2012 May; 94-B (SUPP XXI):60.
Patel RA, Wilson RF, Patel PA, Palmer RM. The effect of smoking on bone healing: A systematic review. Bone Joint Res 2013;2:102–11.
Bistolfi A, Massazza G, Verné E, Massè A, Deledda D, Ferraris S, et al. Antibiotic-loaded cement in orthopedic surgery: A review. ISRN Orthop 2011;2011:290851.
Gogia JS, Meehan JP, Di Cesare PE, Jamali AA. Local antibiotic therapy in osteomyelitis. Semin Plast Surg 2009;23:100–7.
Chang YH, Tai CL, Hsu HY, Hsieh PH, Lee MS, Ueng SW. Liquid antibiotics in bone cement: An effective way to improve the efficiency of antibiotic release in antibiotic loaded bone cement. Bone Joint Res 2014;3:246–51.
Craveiro-Lopes N. Treatment of open fractures of the tibia with locked intramedullary nail with a core release of antibiotics (Safe Dualcore Universal). Comparative study with a standard locked intramedullary nail. J Limb Lengthening Reconstr 2016;2:17–22.
Ślósarczyk A, Czechowska J, Paszkiewicz Z, Zima A. New bone implant material with calcium sulfate and Ti modified hydroxyapatite. J Achiev Mater Manuf Eng 2010;43:170–7.
Noel SP, Courtney H, Bumgardner JD, Haggard WO. Chitosan films: A potential local drug delivery system for antibiotics. Clin Orthop Relat Res 2008;466:1377–82.
Jones CB, Mayo KA. Nonunion treatment: Iliac crest bone graft techniques. J Orthop Trauma 2005;19 10 Suppl: S11–3.
Myeroff C, Archdeacon M. Autogenous bone graft: Donor sites and techniques. J Bone Joint Surg Am 2011;93:2227–36.
Simon JP, Stuyck J, Hoogmartens M, Fabry G. Posterolateral bone grafting for nonunion of the tibia. Acta Orthop Belg 1992;58:308–13.
Ryzewicz M, Morgan SJ, Linford E, Thwing JI, de Resende GV, Smith WR. Central bone grafting for nonunion of fractures of the tibia: A retrospective series. J Bone Joint Surg Br 2009;91:522–9.
Jayaswal A, Bhan S, Dave PK, Chandra P. Modified Phemister grafting in potentially infected nonunion of tibial shaft fractures. Int Surg 1985;70:67–70.
May JW Jr., Jupiter JB, Weiland AJ, Byrd HS. Clinical classification of posttraumatic tibial osteomyelitis. J Bone Joint Surg Am 1989;71:1422–8.
Kaushik SK, Solanki B, Pathania VP, Khan A. Outcome of modified Papineau technique with vacuum-assisted closer system in the treatment of chronic osteomyelitis and infected nonunion of tibia. Int J Sci Study 2016;3:231–4.
Baruah RK. Ilizarov methodology for infected nonunion of the Tibia: Classic circular transfixion wire assembly vs. hybrid assembly. Indian J Orthop 2007;41:198–203.
Kanakaris NK, Tosounidis TH, Giannoudis PV. Surgical management of infected nonunions: An update. Injury 2015;46 Suppl 5:S25–32.
Rohilla R, Wadhwani J, Devgan A, Singh R, Khanna M. Prospective randomised comparison of ring versus rail fixator in infected gap nonunion of tibia treated with distraction osteogenesis. Bone Joint J 2016;98-B: 1399–405.
Pelissier P, Masquelet AC, Bareille R, Pelissier SM, Amedee J. Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration. J Orthop Res 2004;22:73–9.
Masquelet AC, Begue T. The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am. 2010 Jan; 41(1):27–37.
El-Alfy BS, Ali AM. Management of segmental skeletal defects by the induced membrane technique. Indian J Orthop 2015;49:643–8.
Scholz AO, Gehrmann S, Glombitza M, Kaufmann RA, Bostelmann R, Flohe S, et al. Reconstruction of septic diaphyseal bone defects with the induced membrane technique. Injury 2015;46 Suppl 4:S121–4.
Aho OM, Lehenkari P, Ristiniemi J, Lehtonen S, Risteli J, Leskelä HV. The mechanism of action of induced membranes in bone repair. J Bone Joint Surg Am 2013;95:597–604.
Kovoor CC, Jayakumar R, George V, Padmanabhan V, Guild A, Viswanath S. Vascularized fibular graft in infected tibial bone loss. Indian J Orthop 2011;45:330–5.
Semaya Ael-S, Badawy E, Hasan M, El-Nakeeb RM. Management of posttraumatic bone defects of the tibia using vascularised fibular graft combined with Ilizarov external fixator. Injury 2016;47:969–75.
De Long WG Jr, Einhorn TA, Koval K, McKee M, Smith W, Sanders R, et al. Bone grafts and bone graft substitutes in orthopaedic trauma surgery. A critical analysis. J Bone Joint Surg Am 2007;89:649–58.
Finkemeier CG. Bone-grafting and bone-graft substitutes. J Bone Joint Surg Am 2002;84-A: 454–64.
Rozbruch SR, Pugsley JS, Fragomen AT, Ilizarov S. Repair of tibial nonunions and bone defects with the Taylor Spatial Frame. J Orthop Trauma 2008;22:88–95.
Eralp L, Kocaoglu M, Yusof NM, Bulbul M. Distal tibial reconstruction with use of a circular external fixator and an intramedullary nail. The combined technique. J Bone Joint Surg Am 2007;89:2218–24.
El-Rosasy MA. Acute shortening and re-lengthening in the management of bone and soft-tissue loss in complicated fractures of the tibia. J Bone Joint Surg Br 2007;89:80–8.
Nho SJ, Helfet DL, Rozbruch SR. Temporary intentional leg shortening and deformation to facilitate wound closure using the Ilizarov/Taylor spatial frame. J Orthop Trauma 2006;20:419–24.
Lovisetti G, Sala F, Miller AN, Thabet AM, Zottola V, Capitani D. Clinical reliability of closed techniques and comparison with open strategies to achieve union at the docking site. Int Orthop 2012;36:817–25.
Hatzokos I, Stavridis SI, Iosifidou E, Karataglis D, Christodoulou A. Autologous bone marrow grafting combined with demineralized bone matrix improves consolidation of docking site after distraction osteogenesis. J Bone Joint Surg Am 2011;93:671–8.
Calori GM, Tagliabue L, Gala L, d’Imporzano M, Peretti G, Albisetti W. Application of rhBMP-7 and platelet-rich plasma in the treatment of long bone nonunions: A prospective randomised clinical study on 120 patients. Injury 2008;39:1391–402.
Morgan BW, Rogers MJ, Jackson M, Livingstone JA, Monsell F, Atkins RM. The Technique of microdrilling: Stimulation of bone union in patients treated with circular frames with established nonunion. Orthopaedic Proceedings 2008 Aug; 90-B (Supp III):504.
Kiely P, Ward K, Bellemore CM, Briody J, Cowell CT, Little DG. Bisphosphonate rescue in distraction osteogenesis: A case series. J Pediatr Orthop 2007;27:467–71.
Pountos I, Georgouli T, Calori GM, Giannoudis PV. Do nonsteroidal anti-inflammatory drugs affect bone healing? A critical analysis. Scientific World Journal 2012;2012:606404.
Alzahrani MM, Anam EA, Makhdom AM, Villemure I, Hamdy RC. The effect of altering the mechanical loading environment on the expression of bone regenerating molecules in cases of distraction osteogenesis. Front Endocrinol (Lausanne) 2014;5:214.
Gorter EA, Krijnen P, Schipper IB. Vitamin D deficiency in adult fracture patients: Prevalence and risk factors. Eur J Trauma Emerg Surg 2016;42:369–78.
Kanakaris NK, Morell D, Gudipati S, Britten S, Giannoudis PV. Reaming Irrigator Aspirator system: Early experience of its multipurpose use. Injury 2011;42 Suppl 4:S28–34.
Giannoudis PV, Tzioupis C, Green J. Surgical techniques: How I do it? The Reamer/Irrigator/Aspirator (RIA) system. Injury 2009;40:1231–6.
Qvick LM, Ritter CA, Mutty CE, Rohrbacher BJ, Buyea CM, Anders MJ. Donor site morbidity with reamer-irrigator-aspirator (RIA) use for autogenous bone graft harvesting in a single centre 204 case series. Injury 2013;44:1263–9.
Pape HC, Tarkin IS. Reamer irrigator aspirator: A new technique for bone graft harvesting from the intramedullary canal. Oper Tech Orthop 2008;18:108–13.
Chaudhary M, Jain S, Vigneshwaran P, Lakhani P. Infected lower tibial nonunions without bone grafting – Reliable union using the Ilizarov technique. J Limb Lengthening Reconstr 2015;1:21–8.
Hernigou P, Trousselier M, Roubineau F, Bouthors C, Chevallier N, Rouard H, et al. Local transplantation of bone marrow concentrated granulocytes precursors can cure without antibiotics infected nonunion of polytraumatic patients in absence of bone defect. Int Orthop 2016;40:2331–8.
Hernigou P, Poignard A, Beaujean F, Rouard H. Percutaneous autologous bone-marrow grafting for nonunions. Influence of the number and concentration of progenitor cells. J Bone Joint Surg Am 2005;87:1430–7.
Mollon B, da Silva V, Busse JW, Einhorn TA, Bhandari M. Electrical stimulation for long-bone fracture-healing: A meta-analysis of randomized controlled trials. J Bone Joint Surg Am 2008;90:2322–30.
Biglari B, Yildirim TM, Swing T, Bruckner T, Danner W, Moghaddam A. Failed treatment of long bone nonunions with low intensity pulsed ultrasound. Arch Orthop Trauma Surg 2016;136:1121–34.
Shahid S. Role of systemic enzymes in infections. WebmedCentral Complement Med 2011;2:WMC002495.
Grbic R, Miric DJ, Kisic B, Popovic L, Nestorovic V, Vasic A. Sequential analysis of oxidative stress markers and Vitamin C status in acute bacterial osteomyelitis. Mediators Inflamm 2014;2014:975061.
Vernon D’ Silva BS, Suchetha Kumari N, Naveen P, Shetty V, Shetty L. A comparative study of oxidative stress in diabetic and non-diabetic osteomyelitis. RJPBCS 2011;2:342–7.
Giannoudis PV, Gudipati S, Harwood P, Kanakaris NK. Long bone nonunions treated with the diamond concept: A case series of 64 patients. Injury 2015;46 Suppl 8:S48–54.
Calori GM, Giannoudis PV. Enhancement of fracture healing with the diamond concept: The role of the biological chamber. Injury 2011;42:1191–3.
Giannoudis PV, Einhorn TA, Schmidmaier G, Marsh D. The diamond concept – Open questions. Injury 2008;39 Suppl 2:S5–8.
Kocaoglu M, Eralp L, Rashid HU, Sen C, Bilsel K. Reconstruction of segmental bone defects due to chronic osteomyelitis with use of an external fixator and an intramedullary nail. J Bone Joint Surg Am 2006;88:2137–45.
Emara KM, Allam MF. Ilizarov external fixation and then nailing in management of infected nonunions of the tibial shaft. J Trauma 2008;65:685–91.
Author information
Authors and Affiliations
Corresponding author
Additional information
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Rights and permissions
About this article
Cite this article
Chaudhary, M.M. Infected nonunion of tibia. IJOO 51, 256–268 (2017). https://doi.org/10.4103/ortho.IJOrtho_199_16
Published:
Issue Date:
DOI: https://doi.org/10.4103/ortho.IJOrtho_199_16