Abstract
Background
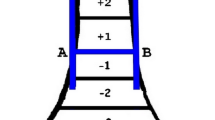
Supracondylar humerus fracture is the most common fracture around elbow in children. Closed reduction and percutaneous Kirschner wire (pin) fixation is the standard method of managing displaced extension type (Gartland Type II and Type III) supracondylar humerus fractures. The configuration of wires is debatable. Although two crossed K-wires are mechanically stable, there is an inherent risk of ulnar nerve injury. Lateral K-wires – parallel or divergent - are good alternative. This study was aimed at identifying the best configuration for the lateral wires.
Materials and Methods
Patients with Gartland type 3 supracondylar humerus fractures were randomized by envelope method to receive closed reduction and K-wire fixation in either a parallel or divergent fashion. The patients were followed up at 3 weeks for wire removal and at 6 weeks and 3 months after surgery. Baumann’s angle, functional outcome as per Flynn’s criteria, and range of motion were recorded in each visit. Effect of delay in surgery was also evaluated as a secondary outcome.
Results
Nineteen patients received fixation with parallel wires and 11 patients had divergent fixation. No loss of reduction was seen in any patient at 3 months. No statistically significant difference was seen in the Baumann’s angles and outcome according to Flynn’s criteria irrespective of the wire configuration (divergent or parallel). Furthermore, the delay in surgery was also found not to have a significant effect on the functional outcome.
Conclusions
Both parallel and divergent K-wire configurations provide satisfactory stability when accurate reduction and adequate fixation of the fracture has been done. Based on the limited number of patients in this study, one configuration cannot be judged to be superior to the other.
Similar content being viewed by others
References
Otsuka NY, Kasser JR. Supracondylar fractures of the humerus in children. J Am Acad Orthop Surg 1997;5:19–26.
Beaty JH, Kasser JR. Fractures about the elbow. Instr Course Lect 1995;44:199–215.
Boyd HB, Altenberg AR. Fractures about the elbow in children. Arch Surg 1944;49:213.
Swenson AL. The treatment of supracondylar fractures of the humerus by Kirschner-wire transfixion. J Bone Joint Surg Am 1948;30A: 993–7.
Casiano E. Reduction and fixation by pinning “banderillero” style-fractures of the humerus at the elbow in children. Mil Med 1960;125:262–4.
Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long term followup. J Bone Joint Surg Am 1974;56:263–72.
Ariño VL, Lluch EE, Ramirez AM, Ferrer J, Rodriguez L, Baixauli F, et al. Percutaneous fixation of supracondylar fractures of the humerus in children. J Bone Joint Surg Am 1977;59:914–6.
Skaggs DL, Hale JM, Bassett J, Kaminsky C, Kay RM, Tolo VT, et al. Operative treatment of supracondylar fractures of the humerus in children. The consequences of pin placement. J Bone Joint Surg Am 2001;83-A:735–40.
Lyons JP, Ashley E, Hoffer MM. Ulnar nerve palsies after percutaneous cross-pinning of supracondylar fractures in children’s elbows. J Pediatr Orthop 1998;18:43–5.
Rasool MN. Ulnar nerve injury after K-wire fixation of supracondylar humerus fractures in children. J Pediatr Orthop 1998;18:686–90.
Gordon JE, Patton CM, Luhmann SJ, Bassett GS, Schoenecker PL. Fracture stability after pinning of displaced supracondylar distal humerus fractures in children. J Pediatr Orthop 2001;21:313–8.
Lee SS, Mahar AT, Miesen D, Newton PO. Displaced pediatric supracondylar humerus fractures: Biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop 2002;22:440–3.
Zionts LE, McKellop HA, Hathaway R. Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children. J Bone Joint Surg Am 1994;76:253–6.
Kallio PE, Foster BK, Paterson DC. Difficult supracondylar elbow fractures in children: Analysis of percutaneous pinning technique. J Pediatr Orthop 1992;12:11–5.
Davis RT, Gorczyca JT, Pugh K. Supracondylar humerus fractures in children. Comparison of operative treatment methods. Clin Orthop Relat Res 2000;376:49–55.
Skaggs DL, Cluck MW, Mostofi A, Flynn JM, Kay RM. Lateral-entry pin fixation in the management of supracondylar fractures in children. J Bone Joint Surg Am 2004;86-A: 702–7.
Lee YH, Lee SK, Kim BS, Chung MS, Baek GH, Gong HS, et al. Three lateral divergent or parallel pin fixations for the treatment of displaced supracondylar humerus fractures in children. J Pediatr Orthop 2008;28:417–22.
Oztürkmen Y, Karamehmetoglu M, Azboy I. Closed reduction and percutaneous lateral pin fixation in the treatment of displaced supracondylar fractures of the humerus in children. Acta Orthop Traumatol Turc 2005;39:396–403.
Foead A, Penafort R, Saw A, Sengupta S. Comparison of two methods of percutaneous pin fixation in displaced supracondylar fractures of the humerus in children. J Orthop Surg (Hong Kong) 2004;12:76–82.
Chakraborty MK, Onta PR, Sathian B. Displaced supracondylar fracture of humerus in children treated with crossed pin versus lateral pin: A hospital based study. J Clin Diagn Res 2011;5:1260–3.
Balakumar B, Madhuri V. A retrospective analysis of loss of reduction in operated supracondylar humerus fractures. Indian J Orthop 2012;46:690–7.
Yen YM, Kocher MS. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. Surgical technique. J Bone Joint Surg Am 2008;90 Suppl 2(Pt 1):20–30.
Maity A, Saha D, Roy DS. A prospective randomised, controlled clinical trial comparing medial and lateral entry pinning with lateral entry pinning for percutaneous fixation of displaced extension type supracondylar fractures of the humerus in children. J Orthop Surg Res 2012;7:6.
Sapkota K, Shrestha B. Study of supracondylar fracture of distal humerus in children and its management with lateral k- wire fixation. Nepal J Med Sci 2014;3:38–43.
Guy SP, Ponnuru RR, Gella S, Tulwa N. Lateral entry fixation using three divergent pins for displaced paediatric supracondylar humeral fractures. ISRN Orthop 2011;2011:137372.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gopinathan, N.R., Sajid, M., Sudesh, P. et al. Outcome Analysis of Lateral Pinning for Displaced Supracondylar Fractures in Children Using Three Kirschner Wires in Parallel and Divergent Configuration. IJOO 52, 554–560 (2018). https://doi.org/10.4103/ortho.IJOrtho_462_17
Published:
Issue Date:
DOI: https://doi.org/10.4103/ortho.IJOrtho_462_17