Abstract
The culotte technique provides near perfect coverage of the carina and side branch ostium at the expense of an excess of metal covering the proximal end. It can be used in almost all true bifurcation lesions, but should be avoided in bifurcations when there is a large mismatch between the proximal main branch and the side branch diameters. The main disadvantage of this technique is that rewiring of both branches through the stent struts is required, which can be difficult, technically demanding, and time-consuming.
Introduction
Although the provisional approach of implanting one stent in the main branch (MB) could be considered as the default approach for most bifurcation lesions, there is still a need for an individualised approach to every bifurcation, and two stents may be required in 20-30% of true bifurcations1. The operator’s decision to perform double stenting is predominantly based on side branch (SB) characteristics, such as lesion severity, distribution and extension in the side branch, diameter and territory of distribution, and bifurcation angle2. Several different double stenting techniques have been described. In 1998, Chevalier et al proposed the “culotte” technique, which was described as implantation of two similar bare metal stents in two steps in the MB and in the SB with overlapping of the two stents in the MB before bifurcation: it was used in 50 patients with true bifurcation lesions. They reported a 94% clinical success rate and a 24% target revascularisation rate, which improved when final kissing post-dilation was used3. However, later publications showed a high percentage of major adverse events and repeat interventions when the culotte technique was implemented with bare metal stents. Since the introduction of drug-eluting stents (DES), culotte stenting has regained its popularity.
The culotte technique, sometimes also referred to as Y stenting or trouser legs, provides near perfect coverage of the carina and SB ostium at the expense of an excess of metal covering the proximal end. It provides excellent immediate angiographic results in most cases and may guarantee a more homogeneous drug distribution at the site of the bifurcation. The culotte technique has been evaluated in several randomised studies4-6.
Technique description
The double stent technique is usually chosen by the operator based on individual experience and lesion morphology. Among the considered double stenting techniques, the rate of the culotte technique varies from 2% in the COBIS II registry up to 66% in Nordic Baltic Bifurcation Study IV7. This technique can be used in almost all true bifurcation lesions, but should be avoided in bifurcations when there is a large mismatch between the proximal MB and SB diameters due to the risk of incomplete SB stent apposition to the proximal MB8. A wide angle between the two branches has been suggested to be an independent predictor of restenosis after culotte stenting9. An historical schematic representation of the culotte stenting steps is shown in Figure 1.
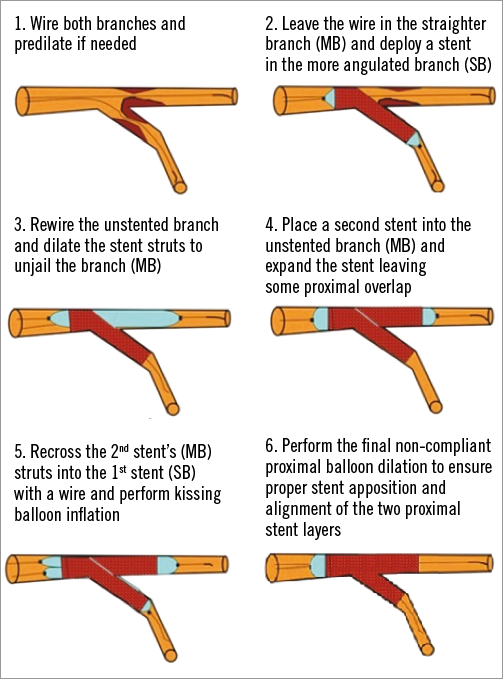
Figure 1. A schematic representation of the culotte technique. Adapted from Latib et al2, with permission from Europa Digital & Publishing.
The procedure can be performed using a 6 Fr or 7 Fr guiding catheter. It is possible to insert two balloons inside a large lumen 6 Fr guiding catheter, but a 7 Fr guiding catheter should be used if the operator anticipates using additional debulking devices, such as rotablators, cutting or scoring balloons. Intravascular imaging methods (intravascular ultrasound, optical coherence tomography) are recommended to assess the plaque distribution and characteristics, to guide the selection of stents and balloons and to evaluate optimal stent expansion.
Both branches are wired. Two different wire types can be helpful to reduce the risk of mixing the wires. Then, both branches are predilated if needed. It is worth noting that adequate plaque modification prior to stent implantation is a key element for treatment of calcified bifurcation lesions. The wire is left in the straighter branch (usually the MB), and the first stent is deployed in the more angulated branch, usually the SB. The non-stented branch (MB) is then rewired through the stent struts, and dilation is performed to unjail the branch and to facilitate passage of the second stent. Then, the second stent is placed and expanded into the non-stented branch (MB) leaving some proximal overlap. It is advisable to avoid a long overlap of stents in the proximal MV whenever possible. “Mini-culotte” with as least proximal a double layer of stent struts as possible is also recommended. When sizing the stent according to distal reference diameter, it is important to choose the stent that allows for adequate expansion in the proximal MB. Drug-eluting stents are recommended for culotte stenting. There is limited experience of bioabsorbable stents in double stenting in general, but conceptually their use should be discouraged in the culotte technique to prevent scaffold strut fractures and excessive strut protrusion in the proximal overlapping segment due to the thickness of the struts. The second stent’s (MB) struts are rewired (SB) and kissing balloon inflation is performed. For the final kissing balloon inflation we recommend using short non-compliant balloons. Each limb of the culotte should be dilated at very high pressure individually before simultaneously inflating both balloons to nominal pressure. In the Nordic Stent Technique Study, final kissing balloon dilatation reduced the long-term rates of MACE, non-procedural myocardial infarction, and stent thrombosis5. Adequate apposition in the proximal MB can be achieved by the proximal optimisation technique (POT), which is a method for expanding the stent from the proximal stent edge to just proximal to the carina with a short oversized balloon. The balloon must be sufficiently short to avoid inflation outside the stent. According to the most recent European Bifurcation Club consensus document, we recommend performing POT after the first stent placement to improve difficult recrossing into the non-stented branch, and after the second stent deployment and after kissing balloon inflation to ensure adequate stent apposition in the proximal MB10.
The main disadvantage of this technique is that rewiring of both branches through the stent struts is required, which can be technically demanding and time-consuming. Several factors can facilitate the success of the procedure. When rewiring the other branch after stent placement, it is reasonable always first to place the guidewire distal into the stented branch to ensure that the wire has not passed under the stent struts before recrossing into the branch. The branch with the sharpest angle should be stented first, because wire recrossing and advancement of the second stent through the first stent struts will be more easily accomplished. The proximal optimisation technique after each stent implantation may also facilitate easier SB access11.
In conclusion, the culotte technique is an attractive bifurcation stenting technique in feasible bifurcation lesion anatomies. Culotte is recommended for two-stent treatment of bifurcation lesions when there is no large mismatch between the proximal MB and SB diameters.
Conflict of interest statement
A. Erglis has received research support grants from Abbott Vascular, Boston Scientific and consulting fees/honoraria from Abbott Vascular, Biosensors, Biotronik, Boston Scientific, J&J Cordis and Medtronic. J.F. Lassen has received research support grants from Biosensors, Abbott Vascular, St. Jude Medical, Boston Scientific, Medtronic, Cordis J&J, Biotronix and Volcano. C. Di Mario has received grant support from Abbott Vascular and Boston Scientific.
Online data supplement
Moving image 1. Angiogram before intervention (left anterior oblique caudal view).
Moving image 2. Angiogram before intervention (left anterior oblique cranial view).
Moving image 3. Final angiogram (left anterior oblique caudal view).
Moving image 4. Final angiogram (left anterior oblique cranial view).
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Angiogram before intervention (left anterior oblique caudal view).
Moving image 2. Angiogram before intervention (left anterior oblique cranial view).
Moving image 3. Final angiogram (left anterior oblique caudal view).
Moving image 4. Final angiogram (left anterior oblique cranial view).




