Published online Oct 16, 2012. doi: 10.4253/wjge.v4.i10.453
Revised: August 24, 2012
Accepted: October 13, 2012
Published online: October 16, 2012
Enteroscopy, defined as direct visualization of the small bowel with the use of a fiberoptic or capsule endoscopy, has progressed considerably over the past several years. The need for endoscopic access to improve diagnosis and treatment of small bowel disease has led to the development of novel technologies one of which is non-invasive, the video capsule, and a type of invasive technique, the device-assisted enteroscopy. In particular, the device-assisted enteroscopy consists then of three different types of instruments all able to allow, in skilled hands, to display partially or throughout its extension (if necessary) the small intestine. Newer devices, double balloon, single balloon and spiral endoscopy, are just entering clinical use. The aim of this article is to review recent advances in small bowel enteroscopy, focusing on indications, modifications to improve imaging and techniques, pitfalls, and clinical applications of the new instruments. With new technologies, the trials and tribulations of learning new endoscopic skills and determining their role in the diagnosis and treatment of small bowel disease come. Identification of small bowel lesions has dramatically improved. Studies are underway to determine the best strategy to apply new enteroscopy technologies for the diagnosis and management of small bowel disease, particularly obscure bleeding. Vascular malformations such as angiectasis and small bowel neoplasms as adenocarcinoma or gastrointestinal stromal tumors. Complete enteroscopy of the small bowel is now possible. However, because of the length of the small bowel, endoscopic examination and therapeutic maneuvers require significant skill, radiological assistance, the use of deep sedation with the assistance of the anesthetist. Prospective randomized studies are needed to guide diagnostic testing and therapy with these new endoscopic techniques.
- Citation: Riccioni ME, Urgesi R, Cianci R, Bizzotto A, Galasso D, Costamagna G. Current status of device-assisted enteroscopy: Technical matters, indication, limits and complications. World J Gastrointest Endosc 2012; 4(10): 453-461
- URL: https://www.wjgnet.com/1948-5190/full/v4/i10/453.htm
- DOI: https://dx.doi.org/10.4253/wjge.v4.i10.453
The diagnosis of small-bowel disorders has long been a challenge to gastroenterologists because of the length of the small intestine, its anatomy, and the lack of adequate diagnostic tools. The advent of capsule endoscopy and push-and-pull enteroscopy during the last decade revolutionized the management of small-bowel disorders.
Although capsule endoscopy can visualize the entire small intestine, a main disadvantage is the inability to obtain biopsy specimens or perform therapeutic manoeuvres via this procedure. In contrast, device-assisted enteroscopy techniques, including double-balloon enteroscopy (DBE), single-balloon enteroscopy (SBE), and spiral enteroscopy (SE), have both diagnostic and therapeutic capabilities.
DBE was first introduced by Sugano et al[1] in 2001 and has gained widespread acceptance since then. It is the most studied and established deep enteroscopy technique to date. Multiple studies have assessed the utility of DBE for the diagnosis and management of various small-bowel disorders, particularly obscure gastrointestinal bleeding (OGIB) and inflammatory bowel disease.
SBE and SE are the latest breakthrough techniques in endoscopic evaluation of the small bowel. Initial studies of deep enteroscopy focused on presenting narrative experiences with the individual techniques. Since then, comparative trials have been conducted to compare the utility of these various techniques in terms of their diagnostic yield, depth of maximal insertion, efficacy, and complications.
This review presents a detailed analysis of the current status of different types of device-assisted enteroscopy (DAE), with particular focus on indications, contraindications, sedation, choice of insertion route, complications, and relevant technical points.
There are currently 3 options available for the performance of deep enteroscopy, DBE, SBE, and spiral enteroscopy.
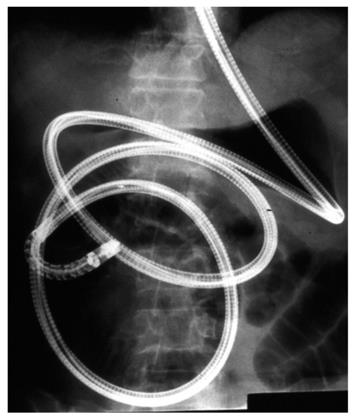
DAE allows deeper intubation of the small bowel compared with push enteroscopy (PE) and ileocolonoscopy. There are two DAEs currently available: the DBE (Fujinon, Wayne, NJ), and the SBE (Olympus America). The concept of DBE was introduced in 1997[1] and was subsequently introduced into the United States in 2004 (Fujinon Inc, Saitama, Japan). The development of DBE was based on the concept that “stretching” of the small intestinal wall prevents further endoscopic advancement, and that the usage of a balloon would grip the intestinal wall and prevent subsequent loop formation[2]. The diagnostic enteroscope (EN450P5) has a 200-cm working length, an endoscope diameter of 8.5 mm, and an accessory channel of 2.2 mm. The therapeutic enteroscope (EN450T5) has a diameter of 9.4 mm and an accessory channel of 2.8 mm. The DBE is composed by both an enteroscope and an overtube, both of which have balloons at the distal end. The two balloons on the DBE are latex made. Both enteroscopies have an overtube length of 140 cm. This type of examinations is generally performed under x-rays control (Figure 1).
Using the DBE entails a series of steps that use a push-and-pull technique[3]. This process facilitates pleating of the small bowel over the enteroscope, allowing for deep enteroscopy. Balloon Assisted Enteroscopy (BAE) can be performed with the antegrade (oral) or retrograde (aboral) approach. DBE allows intubation (240-360 cm antegrade and 102-140 cm retrograde) deeper than possible with PE (90-150 cm) or ileoscopy (50-80 cm).
Its additional diagnostic and therapeutic advantages over capsule endoscopy include its facilitation of biopsies, tattoos, hemostasis, polypectomy, and foreign body removal, dilation and/or stent placement[4-7]. The diagnostic yield of DBE ranges from 60% to 80% in patients with OGIB and other small bowel pathologies. Total enteroscopy with DBE is defined as complete evaluation of the small bowel, with either a single approach or a combined antegrade-retrograde approach. However, it may not be feasible in all patients; the reported success rate is 16%-86%[2,8]. It is likely that the wide range of enteroscopy completion rate among the different Western and Asian study is attributable in part to the different types of patients subject to investigation and partly to the diversity of different chronological studies examined.
The main limitations of DBE include its invasive nature and prolonged duration. The reported complication rate for diagnostic procedures is 0.8% but can be as much as 4% with therapeutics such as electrocoagulation, polypectomy, or dilation. The main complications are pancreatitis, ileus and perforation[5,9,10]. Patients who are not medically stable should not undergo BAE. Those who have had extensive abdominal surgeries may be poor candidates because of adhesions or altered anatomy which may prevent the scope from advancing.
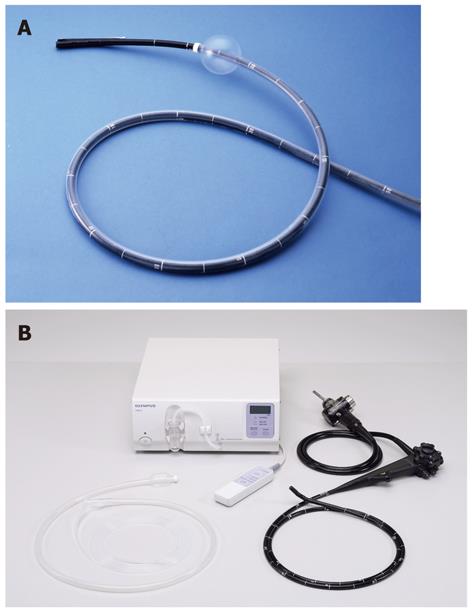
The SBE system includes the SIF-Q160 endoscope (Olympus Optical Company, Ltd, Tokyo, Japan) with a working length of 200 cm and 9.8 mm in diameter and contains a 2.8 mm diameter working channel (Figure 2A), the Balloon Control Unit OBCU (Figure 2B) and the ST-SB1 single-use splinting tube (overtube) with a length of 132 cm and an outer diameter of 13.2 mm (Figure 2B).
The splinting tube’s smooth glide, hydrophilic coating is activated with the simple addition of 30 mL of water. The SBE is controlled by repeatedly inflating and deflating a single balloon, attached to the distal end of the splinting tube, via the remote balloon controller.
Radiopaque material is used in the distal end of the ST-SB1 to allow confirmation of the splinting tube’s tip under fluoroscopy, further enhancing insertion performance into the deep small intestine. To improve manoeuvrability of insertion, the SIF-Q160 features a distal-end diameter of just 9.2 mm while maintaining a high-resolution image quality. By optimizing both the distal end length and bending section radius, the SIF-Q160 extensive angulation capability allows acute turns in the small intestine, which allows a smoother insertion. So the ST-SB1 single use splinting tubes used as over-tubes are made from silicone rubber to eliminate the risk of latex allergy[11,12].
Spiral enteroscopy is the newest enteroscope system available for clinical use (Figure 2B). The Endo-Ease Discovery SB (Spirus Medical, Stoughton, MA) is a spiral-shaped overtube 118 cm long; its hollow spiral is 5.5 mm high and 22 cm long, with a locking device on the proximal end. It is used for enteroscopy via the oral route and can be used only with enteroscopies < 9.4 mm in diameter. Spiral enteroscopy allows for advancement and withdrawal of the enteroscope through the small bowel with rotatory clockwise and counter clockwise movements. The distal end of the overtube is positioned 25 cm from the tip of the enteroscope and locked into place. The system is then advanced to the ligament of Treitz with gentle rotation. Once there, the collar is unlocked and the enteroscope is advanced past the ligament of Treitz[13]. There is also an overtube for a rectal approach called the Endo-Ease Vista Retrograde (Spirus Medical), which can be used for limited ileoscopy, as well as for difficult colonoscopy using a pediatric colonoscope.
Preliminary reports with spiral enteroscopy demonstrate insertion depths less than reported with DBE/SBE but carries the associated advantage of accelerated procedural times. A preliminary study of the Discovery SB suggested a diagnostic yield of 33% and an average depth of insertion of 176 cm from the ligament of Treitz[13]. Another study reported a mean ± SD depth of insertion of 262 ± 5 cm and a mean total procedure time of 33.6 ± 8 min[14]. This modality also allows performance of therapeutics, including biopsy, hemostasis, and polypectomy. The rate of severe complications is reported to be 0.3%, with a perforation rate of 0.27%[15]. No esophageal or gastric perforations have occurred. The device is easy to use and may be effectively operated in as few as five training cases[16,17]. The main characteristics of the three enteroscopic techniques are shown in Table 1.
| Single balloon | Double balloon | Spirus enteroscopy | |
| The depth of insertion | Similar | Similar | Similar |
| Diagnostic yield | Similar | Similar | Slightly lower |
| Therapeutic interventions | Similar | Similar | Similar |
| Complications rate | Similar | Similar | Slightly lower |
| Duration of the enteroscopy | Similar | Similar | Slightly lower |
| Duration of the sedoanalgesia | Similar | Similar | Slightly lower |
| Learning curve | Similar | Similar | Similar |
Preparation for DAE examination includes a 12 h overnight fast. Patients, who underwent anterograde and retrograde procedures, received 2 L and 4 L of polyethylene glycol electrolyte lavage solution the day before examination, respectively.
The starting insertion oral or anal route was chosen as per clinical judgement according to the probable location of the suspected lesions on the basis of clinical presentation and of previous investigations. Many of the procedures were performed under deep sedation or general anaesthesia.
The main therapeutical indications for BAE include the need for treatment of small intestinal lesions found on other gastrointestinal investigations, such as capsule endoscopy or radiological examinations. However, an initial capsule endoscopy study remained a preferred initial strategy owing to the higher complication rate associated with DAE. The procedure is not used in Western Countries as a first line therapy and is performed only after careful evaluation by a specially trained gastroenterologist[17]. The main indications are: bleeding lesions seen on capsule endoscopy, worrisome lesions or masses seen by other modalities, polyps in patients with hereditary syndromes, retained foreign objects (especially small-bowel capsules), and small bowel strictures[18]. Therapies include treatment of bleeding lesions such as angioectasias, dilation of strictures using a hydrostatic balloon dilator, removal by snare or biopsy of polyps or small bowel masses, retrieval and removal of foreign objects or retained capsules, and biopsy of abnormal tissue. Balloon assisted enteroscopy has also been used in gaining access to parts of the gastrointestinal tract in patients with surgically altered anatomy.
OGIB has been defined as bleeding from the gastrointestinal tract that persists or recurs after a negative initial evaluation of digestive system by upper and lower endoscopy[19].
BAE (including possible total enteroscopy) should be pursued after a negative CE but high clinical suspicion for a small bowel lesion[20].
In multiple large studies of patients with OGIB who underwent BAE, the diagnostic yield ranged from 43% to 81%[6,21-26]. Treatment success rates of between 43% and 84% have been reported[6,22-25]. Few studies have evaluated a combined antegrade and retrograde approach[6,23-25]. Multiple studies have been conducted to compare BAE with PE and CE. In one controlled, prospective trial of 52 patients with OGIB, BAE was superior to PE in length of small bowel visualized (230 cm vs 80 cm, P < 0.0001) and diagnostic yield (63% vs 44%, P < 0.0001)[27].
A meta-analysis of 11 studies comparing the yield of CE and BAE, including 375 patients with small-bowel disease, reported comparable diagnostic yields (60% vs 57%, respectively). The pooled yield for angiectasis in the 350 patients with OGIB was similar, with 24% for both CE and BAE[28]. A more recent retrospective study of 162 patients with OGIB also suggested no significant difference in overall diagnostic yield between CE (54%) and BAE (64%)[26]. Similar results were found in another meta analysis. In this study, a sub analysis of 191 patients undergoing only antegrade or retrograde BAE indicated a significantly higher yield of CE vs BAE (62% vs 50%, P < 0.05). However, when both antegrade and retrograde BAEs were performed in 24 patients, the yield of BAE was higher than that of CE (88% vs 46%, P < 0.01)[29]. Finally, in a retrospective study investigating the role of BAE prior to intraoperative endoscopy for those in whom BAE identified a source (53/56 patients), subsequent intraoperative endoscopy was negative in only one patient[30].
A modeled cost-minimization analysis of the management of occult OGIB proposed BAE as the most cost-effective initial test after standard endoscopy if the goal is treatment or definitive diagnosis[31]. Another model suggested that initial BAE was a cost-effective approach for patients with OGIB who likely have angiectasis in the small bowel accessible with a single antegrade approach[32]. However, comparative studies regarding existing deep enteroscopy techniques are controversial[30].
The yield of Crohn’s disease (CD) in patients who undergo DAE (DBE) for suspected small bowel disorders has been reported as 5%-13%[33], whereas the yield is substantially higher (74%-96%) in patients with known inflammatory bowel disease[34,35]. The diagnosis of CD, reached by BAE, influenced medical management in 63% but the procedure was unsuccessful in 26% of patients who underwent previous abdominal surgery[35]. In a recent study comparing the diagnostic yield of DBE and Small Bowel Follow Through, 60% of patients had small bowel involvement proximal to the distal 20 cm of the ileum that was not accessible to detection by ileocolonoscopy[36]. DBE and CE have an apparently equivalent yield for diagnosis of CD and appear to be complementary[37]. A meta-analysis of 11 studies comparing CE with DBE in 375 patients with suspected mild-gut disease found a comparable yield for detection of mild-gut inflammation (pooled yield, 16% with DBE and 18% with CE[28]). When ileocolonoscopy is negative, CE may be helpful because it is relatively non invasive and has a higher rate of success for achieving total enteroscopy, whereas BAE is useful for tissue diagnosis[28].
BAE can also help with regard to therapeutic interventions in CD. DBE appears useful in facilitating endoscopic dilation of strictures, thereby decreasing the need for surgery[38,39]. DBE has an additional role in retrieval of retained capsules, which also helps avoid surgery[40].
Primary tumors of the small bowel are approximately 5% of all primary gastrointestinal neoplasms[41]. Traditionally, they have been difficult to diagnose because of a vague clinical presentation and the limitations of the usual diagnostic techniques in SB visualization[42].
Several studies suggest that DBE is useful in the diagnosis and treatment of small bowel tumors and polyps, including neuroendocrine tumors, Peutz-Jeghers syndrome, and familial adenomatous polyposis[43-48]. One small study using DBE and intraoperative enteroscopy to evaluate 41 patients with familial adenomatous polyposis suggested that DBE is of equivalent value for evaluation of SB adenomas[49]. A meta-analysis found DBE and CE to be equal in diagnostic yield[28]. DBE can also identify single-mass lesions missed on capsule endoscopy[50].
In a published series is discussed the role of enteroscopy and endoscopic tattoos to facilitate minimal-invasive surgery[18].
Few published studies address the role of DAE in evaluating celiac disease. One study examined the role of DBE in patients with refractory disease[51]. Twenty-four procedures were performed in 21 patients. Enteropathy-associated T-cell lymphoma was found in 5 patients, and ulcerative jejunitis was found in 2 patients. In another study evaluating DBE in 12 patients with malabsorption, DBE yielded a diagnosis in 8 patients[52].
Overall, DBE had a diagnostic value of 42% in patients with malabsorption of unclear origin. The authors suggested reserving DBE for patients with unexplained malabsorption and normal duodenal biopsies.
Papers related to the use and application of DBE in children and adolescents is limited. Small intestinal DAE in the paediatric population remains a relatively unknown and perhaps an undervalued diagnostic and therapeutic procedure when compared with the collective adult DBE experience in which the therapeutic benefits of this technique have been clearly established. This may be because of a different spectrum of digestive pathophysiology in children in whom small intestinal bleeding, the most common indication for DBE in the adult population, is relatively uncommon. As an essentially unknown procedure in paediatrics, the safety and efficacy of DBE in this population remains to be determined. Thus, the main indications in paediatric patients seem to be related to inflammatory bowel disease.
Recently, Lin et al[53] reported thirteen DBE procedures performed on eleven 8- to 20-year old patients. Clinically significant lesions were identified in 46% (6/13) of the procedures performed. 6 procedures (6/13, 46%) were diagnostic or therapeutic for the patient and positively influenced their clinical management. A diagnosis of Crohn’s disease was confirmed in 2 patients, and an antegrade DBE procedure for another patient with a cavernous hemangioma proved to be both diagnostic and therapeutic. Three procedures were therapeutic in the patients with Peutz-Jeghers syndrome with removal of symptomatic hamartomatous polyps, an intervention that would traditionally have required a surgical approach.
No serious procedure-related complications occurred. Self limited postprocedure abdominal pain and discomfort from gaseous distension was observed in several patients. DBE appears to be a safe endoscopic modality for the diagnosis and treatment of children and adolescents with suspected small bowel disease.
In recent studies using double balloon enteroscopy to complete previously failed colonoscopy successful cecal intubation was achieved in 88% to 100% of patients[54-59]. In the largest study[60], successful DBE colonoscopy was achieved in 93% of patients, with a mean time-to-cecum of 19 min. However, other studies of DBE colonoscopy have illustrated procedure times that are no faster than those in this study, with mean time-to-cecum of 28 min in one study[54] and mean total procedure time of 51 min in another[58]. No studies on these arguments are published on SBE.
In conclusion, balloon assisted colonoscopy seems a safe and effective method for completing colonoscopy in patients with a previously failed or difficult colonoscopy.
There have recently been reports on diagnostic and therapeutic ERCP using a DBE for pancreaticobiliary lesions in patients with a history of intestinal bypass surgery[61-65], in cases of surgical reconstruction, such as Roux-en-Y and Billroth II, and cases of anastomosis, such as choledochojejunostomy and hepaticojejunostomy.
As recently outlined by several other investigators in small patients series[63-68], our stepwise approach with push-enteroscope (PE) and DBE in 37 non-selected, consecutive post-surgical patients found that DBE-ERCP was clearly more efficient than PE. By the appropriate use of DBE in over two-thirds of cases, enteroanastomoses or papilla could be repeatedly reached, identified and satisfactorily visualized. DBE-ERCP could be successfully conducted in 74.1% of the cases via the enteroscope, while PE reached biliary anastomoses or papilla in only 16.2% of the patients, which resulted in successful ERCP in only a minority of patients. Both results are in good agreement with recently published data for the approach by double- or single-balloon enteroscopy[67-69].
The threading of the small intestine onto the DBE and the option to block the balloons at the enteroscope provides the enteroscope tip with a greater possibility of movement for identifying the biliary or pancreatic anastomoses or the papilla. In addition, sliding back of the enteroscope may be prevented by inflated balloons, which, compared with PE, explains the significantly higher effectiveness of interventions during DBE-ERCP.
In a recent study of Raithel et al[70] out of the 37 post-surgical patients with significant cholestasis and cholangitis, PE achieved a successful bile duct drainage in six (16.2%), whereas DBE facilitated successful ERCP with biliary interventional procedures leading to significant reduction of cholestasis or cholangitis in 23 of 31 patients (74.1%). Only one case of post-papillotomy bleeding (3.2%), two of post-ERCP pancreatitis (6.4%) and two perforations (6.4%) occurred following DBE-ERCP, but no cholangitis or mortality has been recorded to date.
Thus, this first prospective investigation from a university tertiary referral center confirms that DBE-ERCP has considerable potential to treat successfully benign (postoperative) or malignant biliary and papillary stenosis.
The key benefits of DBE-ERCP in the care of post-surgical patients with cholestasis/cholangitis and patients with installed percutaneous drainage are somewhat limited by the small caliber of bile duct prostheses that are applied via the enteroscope. According to the present state of technology, only an implantation of 5-8 Fr prostheses through an operating channel of 2.8 mm is possible. Consequently, several prostheses (1.5 ± 0.7) were implanted in our patients. Considering the enormous benefit of DBE-ERCP with an approximately 74% successful biliary drainage and a significantly smaller complication rate than Percutaneous Transhepatic Cholangio Draimage (PTCD)[71-73], the effort involved in such an examination seems justified.
In conclusion, DBE for direct cholangiography seems to be a possible option, particularly in patients with a past history of abdominal surgery.
The most commonly reported complications to date have included pancreatitis, hemorrhage, and intestinal perforation. In a 10-center study describing 2362 DBE procedures performed in Europe and Japan, there were 40 (1.7%) complications, including pancreatitis in 7 (0.3%), bleeding in 19 (0.8%), and perforation in 6 (0.3%)[10]. Perforation occurred after argon plasma coagulation therapy for AVMs in 3 (1.2%) patients and after stricture dilation in 2 (2.9%) cases. In another publication reporting complications in 178 therapeutic DBE procedures, severe treatment-associated complications occurred in 6 (3.4%): bleeding in 2 patients, perforation in 3 patients after polypectomy of large polyps and segmental enteritis after APC in 1 patient[74]. Although there are no published contraindications to date, inflation of the balloons resulting in distention of the small bowel may lead to perforation in patients with pre-existing weakened small intestine from inflammatory conditions or in areas of surgically altered anatomy.
Perforations have been described in patients with small bowel lymphoma undergoing chemotherapy[33], in patients with recently created intestinal anastomoses[24], in the scenario of stricturing ileal Crohn’s disease[33], and in patients with altered surgical anatomy, including ileal anal anastomoses[75]. In a retrospective analysis of 2478 DBE examinations performed in 9 United States centers[76,77] (1691 anterograde examinations and 722 retrograde DBEs), there were a total of 22 (0.9%) major complications, including perforation in 11 (0.4%), pancreatitis in 6 (0.2%), and bleeding in 4 (0.2%). Perforations occurred in 3 of 1691 (0.2%) oral examinations and in 8 of 722 (1.2%) rectal DBEs. Eight (73%) perforations occurred during diagnostic DBE examinations.
Four of 8 rectal DBE perforations occurred in patients with prior ileoanal or ileocolonic anastomoses. In the subset of patients with available data regarding altered surgical anatomy, perforations occurred in 7 (3%) patients. On the basis of these data, the presence of altered surgical anatomy and the execution of therapeutic procedures should be considered to be a higher risk conditions in the performance of balloon-assisted enteroscopy.
In the end, in literature have been reported same cases of unrecognized aspiration pneumonitis during enteroscopy resolved with medical therapy[78,79].
The advent of balloon-assisted enteroscopy has allowed the endoscopist access to areas of the small intestine that were not previously accessible. This article was designed to review the history of small-bowel enteroscopy, the technical aspects of balloon-assisted enteroscopy, and common problems encountered by endoscopists performing DAE.
With this rapidly evolving technology, our ability to diagnose and treat patients with mid-gut diseases has improved enormously, resulting in a substantial change in the management paradigm for these previously elusive disorders. This new technology has improved our ability to diagnose and monitor and treat artero-venous-malformations (AVMs), CD and small bowel neoplasms. In many cases, the ability to perform therapeutic interventions has eliminated the need for invasive surgical procedures. However, larger studies are needed to determine the impact on clinical outcomes. None of the available techniques in this moment seems to be superior to another.
Peer reviewer: Carlo M Girelli, MD, 1st Department of Internal Medicine, Service of Gastroenterology and Digestive Endoscopy, Hospital of Busto Arsizio, Via Arnaldo da Brescia, 121052 Busto Arsizio (VA), Italy
S- Editor Song XX L- Editor A E- Editor Zhang DN
| 1. | Sugano KYH, Kita H. Double-balloon endoscopy: theory and practice. New York: Springer 2006; . [DOI] [Cited in This Article: ] |
| 2. | Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216-220. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 896] [Cited by in F6Publishing: 828] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 3. | Mönkemüller K, Fry LC, Bellutti M, Malfertheiner P. Balloon-assisted enteroscopy: unifying double-balloon and single-balloon enteroscopy. Endoscopy. 2008;40:537; author reply 539. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Nakamura M, Niwa Y, Ohmiya N, Miyahara R, Ohashi A, Itoh A, Hirooka Y, Goto H. Preliminary comparison of capsule endoscopy and double-balloon enteroscopy in patients with suspected small-bowel bleeding. Endoscopy. 2006;38:59-66. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 171] [Cited by in F6Publishing: 189] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 5. | Heine GD, Hadithi M, Groenen MJ, Kuipers EJ, Jacobs MA, Mulder CJ. Double-balloon enteroscopy: indications, diagnostic yield, and complications in a series of 275 patients with suspected small-bowel disease. Endoscopy. 2006;38:42-48. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 295] [Cited by in F6Publishing: 317] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 6. | May A, Ell C. Push-and-pull enteroscopy using the double-balloon technique/double-balloon enteroscopy. Dig Liver Dis. 2006;38:932-938. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Ross AS, Semrad C, Waxman I, Dye C. Enteral stent placement by double balloon enteroscopy for palliation of malignant small bowel obstruction. Gastrointest Endosc. 2006;64:835-837. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 60] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Ell C, May A. Mid-gastrointestinal bleeding: capsule endoscopy and push-and-pull enteroscopy give rise to a new medical term. Endoscopy. 2006;38:73-75. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 80] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | May A, Nachbar L, Ell C. Double-balloon enteroscopy (push-and-pull enteroscopy) of the small bowel: feasibility and diagnostic and therapeutic yield in patients with suspected small bowel disease. Gastrointest Endosc. 2005;62:62-70. [PubMed] [Cited in This Article: ] |
| 10. | Mensink PB, Haringsma J, Kucharzik T, Cellier C, Pérez-Cuadrado E, Mönkemüller K, Gasbarrini A, Kaffes AJ, Nakamura K, Yen HH. Complications of double balloon enteroscopy: a multicenter survey. Endoscopy. 2007;39:613-615. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 261] [Cited by in F6Publishing: 273] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 11. | Tsujikawa T, Saitoh Y, Andoh A, Imaeda H, Hata K, Minematsu H, Senoh K, Hayafuji K, Ogawa A, Nakahara T. Novel single-balloon enteroscopy for diagnosis and treatment of the small intestine: preliminary experiences. Endoscopy. 2008;40:11-15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 215] [Cited by in F6Publishing: 200] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 12. | Vargo JJ, Upchurch B, Dumot JA. Clinical utility of the Olympus single balloon enteroscope: the initial US experience [abstract]. Gastrointest Endosc. 2007;65:AB90. [DOI] [Cited in This Article: ] |
| 13. | Akerman PA, Agrawal D, Chen W, Cantero D, Avila J, Pangtay J. Spiral enteroscopy: a novel method of enteroscopy by using the Endo-Ease Discovery SB overtube and a pediatric colonoscope. Gastrointest Endosc. 2009;69:327-332. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 94] [Cited by in F6Publishing: 97] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 14. | Buscaglia JM, Dunbar KB, Okolo PI, Judah J, Akerman PA, Cantero D, Draganov PV. The spiral enteroscopy training initiative: results of a prospective study evaluating the Discovery SB overtube device during small bowel enteroscopy (with video). Endoscopy. 2009;41:194-199. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 62] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 15. | Akerman PA, Cantero D. Complications of spiral enteroscopy in the first 2950 patients [abstract]. Available from: http// www.gastro2009.org/scien_prog/abstract_detail.php?navId=93&ssid=760. [Cited in This Article: ] |
| 16. | Nagula S, Gaidos J, Draganov PV, Bucobo JC, Cho B, Hernandez Y, Buscaglia JM. Retrograde spiral enteroscopy: feasibility, success, and safety in a series of 22 patients. Gastrointest Endosc. 2011;74:699-702. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Riccioni ME, Bizzotto A, Cianci R. How can we compare apples and oranges? Am J Gastroenterol. 2010;105:2504; author reply 2504-2505. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Riccioni ME, Cianci R, Urgesi R, Bizzotto A, Spada C, Rizzo G, Coco C, Costamagna G. Advance in diagnosis and treatment of small bowel tumors: a single-center report. Surg Endosc. 2012;26:438-441. [PubMed] [Cited in This Article: ] |
| 19. | Raju GS, Gerson L, Das A, Lewis B. American Gastroenterological Association (AGA) Institute technical review on obscure gastrointestinal bleeding. Gastroenterology. 2007;133:1697-1717. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 379] [Cited by in F6Publishing: 404] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 20. | Pasha SF, Leighton JA. How useful is capsule endoscopy for the selection of patients for double-balloon enteroscopy? Nat Clin Pract Gastroenterol Hepatol. 2008;5:490-491. [PubMed] [Cited in This Article: ] |
| 21. | Zhi FC, Yue H, Jiang B, Xu ZM, Bai Y, Xiao B, Zhou DY. Diagnostic value of double balloon enteroscopy for small-intestinal disease: experience from China. Gastrointest Endosc. 2007;66:S19-S21. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Zhong J, Ma T, Zhang C, Sun B, Chen S, Cao Y, Wu Y. A retrospective study of the application on double-balloon enteroscopy in 378 patients with suspected small-bowel diseases. Endoscopy. 2007;39:208-215. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 99] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 23. | Cazzato IA, Cammarota G, Nista EC, Cesaro P, Sparano L, Bonomo V, Gasbarrini GB, Gasbarrini A. Diagnostic and therapeutic impact of double-balloon enteroscopy (DBE) in a series of 100 patients with suspected small bowel diseases. Dig Liver Dis. 2007;39:483-487. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Mehdizadeh S, Ross A, Gerson L, Leighton J, Chen A, Schembre D, Chen G, Semrad C, Kamal A, Harrison EM. What is the learning curve associated with double-balloon enteroscopy? Technical details and early experience in 6 U.S. tertiary care centers. Gastrointest Endosc. 2006;64:740-750. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 201] [Cited by in F6Publishing: 214] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 25. | Manabe N, Tanaka S, Fukumoto A, Nakao M, Kamino D, Chayama K. Double-balloon enteroscopy in patients with GI bleeding of obscure origin. Gastrointest Endosc. 2006;64:135-140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 83] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 26. | Arakawa D, Ohmiya N, Nakamura M, Honda W, Shirai O, Itoh A, Hirooka Y, Niwa Y, Maeda O, Ando T. Outcome after enteroscopy for patients with obscure GI bleeding: diagnostic comparison between double-balloon endoscopy and videocapsule endoscopy. Gastrointest Endosc. 2009;69:866-874. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 133] [Cited by in F6Publishing: 148] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 27. | May A, Nachbar L, Schneider M, Ell C. Prospective comparison of push enteroscopy and push-and-pull enteroscopy in patients with suspected small-bowel bleeding. Am J Gastroenterol. 2006;101:2016-2024. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 99] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 28. | Pasha SF, Leighton JA, Das A, Harrison ME, Decker GA, Fleischer DE, Sharma VK. Double-balloon enteroscopy and capsule endoscopy have comparable diagnostic yield in small-bowel disease: a meta-analysis. Clin Gastroenterol Hepatol. 2008;6:671-676. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 270] [Cited by in F6Publishing: 248] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 29. | Chen X, Ran ZH, Tong JL. A meta-analysis of the yield of capsule endoscopy compared to double-balloon enteroscopy in patients with small bowel diseases. World J Gastroenterol. 2007;13:4372-4378. [PubMed] [Cited in This Article: ] |
| 30. | Lin MB, Yin L, Li JW, Hu WG, Qian QJ. Double-balloon enteroscopy reliably directs surgical intervention for patients with small intestinal bleeding. World J Gastroenterol. 2008;14:1936-1940. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 13] [Cited by in F6Publishing: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 31. | Somsouk M, Gralnek IM, Inadomi JM. Management of obscure occult gastrointestinal bleeding: a cost-minimization analysis. Clin Gastroenterol Hepatol. 2008;6:661-670. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Gerson L, Kamal A. Cost-effectiveness analysis of management strategies for obscure GI bleeding. Gastrointest Endosc. 2008;68:920-936. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 97] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 33. | Yamamoto H, Kita H, Sunada K, Hayashi Y, Sato H, Yano T, Iwamoto M, Sekine Y, Miyata T, Kuno A. Clinical outcomes of double-balloon endoscopy for the diagnosis and treatment of small-intestinal diseases. Clin Gastroenterol Hepatol. 2004;2:1010-1016. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 471] [Cited by in F6Publishing: 499] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 34. | Kodama M, Uto H, Numata M, Hori T, Murayama T, Sasaki F, Tsubouchi N, Ido A, Shimoda K, Tsubouchi H. Usefulness of double-balloon endoscopy as a diagnostic and therapeutic method for small-intestinal involvement in patients with inflammatory bowel disease [abstract]. Gastrointest Endosc. 2007;65:AB188. [DOI] [Cited in This Article: ] |
| 35. | Ross A, Mehdizadeh S, Tokar J, Leighton JA, Kamal A, Chen A, Schembre D, Chen G, Binmoeller K, Kozarek R. Double balloon enteroscopy in Crohn’s disease: fi ndings and impact on management [abstract]. Gastroenterology. 2007;132:A654. [Cited in This Article: ] |
| 36. | Oshitani N, Yukawa T, Yamagami H, Inagawa M, Kamata N, Watanabe K, Jinno Y, Fujiwara Y, Higuchi K, Arakawa T. Evaluation of deep small bowel involvement by double-balloon enteroscopy in Crohn's disease. Am J Gastroenterol. 2006;101:1484-1489. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 100] [Cited by in F6Publishing: 84] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 37. | Kenji W, Hosomi S, Hirata N. Useful diagnostic strategy in combination capsule endoscopy with double balloon endoscopy for Crohnâs disease [abstract]. 5th International Conference on Capsule Endoscopy, Program and Abstracts. 2006;. [Cited in This Article: ] |
| 38. | Sunada K, Yamamoto H, Kita H, Yano T, Sato H, Hayashi Y, Miyata T, Sekine Y, Kuno A, Iwamoto M. Clinical outcomes of enteroscopy using the double-balloon method for strictures of the small intestine. World J Gastroenterol. 2005;11:1087-1089. [PubMed] [Cited in This Article: ] |
| 39. | Pohl J, May A, Nachbar L, Ell C. Diagnostic and therapeutic yield of push-and-pull enteroscopy for symptomatic small bowel Crohn's disease strictures. Eur J Gastroenterol Hepatol. 2007;19:529-534. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 40. | Lee BI, Choi H, Choi KY, Ji JS, Kim BW, Cho SH, Park JM, Lee IS, Choi MG, Chung IS. Retrieval of a retained capsule endoscope by double-balloon enteroscopy. Gastrointest Endosc. 2005;62:463-465. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 52] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 41. | Giuliani A, Caporale A, Teneriello F, Alessi G, Serpieri S, Sammartino P. Primary tumors of the small intestine. Int Surg. 1985;70:331-334. [PubMed] [Cited in This Article: ] |
| 42. | Schwartz GD, Barkin JS. Small bowel tumors. Gastrointest Endosc Clin N Am. 2006;16:267-275. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 43. | Almeida N, Figueiredo P, Lopes S, Gouveia H, Leitão MC. Double-balloon enteroscopy and small bowel tumors: a South-European single-center experience. Dig Dis Sci. 2009;54:1520-1524. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 44. | Fry LC, Neumann H, Kuester D, Kuhn R, Bellutti M, Malfertheiner P, Monkemuller K. Small bowel polyps and tumours: endoscopic detection and treatment by double-balloon enteroscopy. Aliment Pharmacol Ther. 2009;29:135-142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 45. | Koornstra JJ, de Vries EG, Porte RJ. Improvements in small bowel carcinoid diagnosis and staging: 18F-DOPA PET, capsule endoscopy and double balloon enteroscopy. Dig Liver Dis. 2009;41:e35-e38. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 46. | Bellutti M, Fry LC, Schmitt J, Seemann M, Klose S, Malfertheiner P, Mönkemüller K. Detection of neuroendocrine tumors of the small bowel by double balloon enteroscopy. Dig Dis Sci. 2009;54:1050-1058. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 47. | Mönkemüller K, Fry LC, Ebert M, Bellutti M, Venerito M, Knippig C, Rickes S, Muschke P, Röcken C, Malfertheiner P. Feasibility of double-balloon enteroscopy-assisted chromoendoscopy of the small bowel in patients with familial adenomatous polyposis. Endoscopy. 2007;39:52-57. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 48. | Gao H, van Lier MG, Poley JW, Kuipers EJ, van Leerdam ME, Mensink PB. Endoscopic therapy of small-bowel polyps by double-balloon enteroscopy in patients with Peutz-Jeghers syndrome. Gastrointest Endosc. 2010;71:768-773. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 49. | Matsumoto T, Esaki M, Yanaru-Fujisawa R, Moriyama T, Yada S, Nakamura S, Yao T, Iida M. Small-intestinal involvement in familial adenomatous polyposis: evaluation by double-balloon endoscopy and intraoperative enteroscopy. Gastrointest Endosc. 2008;68:911-919. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 50. | Ross A, Mehdizadeh S, Tokar J, Leighton JA, Kamal A, Chen A, Schembre D, Chen G, Binmoeller K, Kozarek R. Double balloon enteroscopy detects small bowel mass lesions missed by capsule endoscopy. Dig Dis Sci. 2008;53:2140-2143. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 144] [Cited by in F6Publishing: 134] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 51. | Hadithi M, Al-toma A, Oudejans J, van Bodegraven AA, Mulder CJ, Jacobs M. The value of double-balloon enteroscopy in patients with refractory celiac disease. Am J Gastroenterol. 2007;102:987-996. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 80] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 52. | Fry LC, Bellutti M, Neumann H, Malfertheiner P, Monkemuller K. Utility of double-balloon enteroscopy for the evaluation of malabsorption. Dig Dis. 2008;26:134-139. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 53. | Lin TK, Erdman SH. Double-balloon enteroscopy: pediatric experience. J Pediatr Gastroenterol Nutr. 2010;51:429-432. [PubMed] [Cited in This Article: ] |
| 54. | Kaltenbach T, Soetikno R, Friedland S. Use of a double balloon enteroscope facilitates caecal intubation after incomplete colonoscopy with a standard colonoscope. Dig Liver Dis. 2006;38:921-925. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 45] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 55. | Gay G, Delvaux M. Double-balloon colonoscopy after failed conventional colonoscopy: a pilot series with a new instrument. Endoscopy. 2007;39:788-792. [PubMed] [Cited in This Article: ] |
| 56. | Kita H, Yamamoto H. New indications of double balloon endoscopy. Gastrointest Endosc. 2007;66:S57-S59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 57. | Mönkemüller K, Knippig C, Rickes S, Fry LC, Schulze A, Malfertheiner P. Usefulness of the double-balloon enteroscope in colonoscopies performed in patients with previously failed colonoscopy. Scand J Gastroenterol. 2007;42:277-278. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 58. | Pasha SF, Harrison ME, Das A, Corrado CM, Arnell KN, Leighton JA. Utility of double-balloon colonoscopy for completion of colon examination after incomplete colonoscopy with conventional colonoscope. Gastrointest Endosc. 2007;65:848-853. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 77] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 59. | Teshima CW, Aktas H, Haringsma J, Kuipers EJ, Mensink PB. Single-balloon-assisted colonoscopy in patients with previously failed colonoscopy. Gastrointest Endosc. 2010;71:1319-1323. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 60. | Moreels TG, Macken EJ, Roth B, Van Outryve MJ, Pelckmans PA. Cecal intubation rate with the double-balloon endoscope after incomplete conventional colonoscopy: a study in 45 patients. J Gastroenterol Hepatol. 2010;25:80-83. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 61. | Chu YC, Yang CC, Yeh YH, Chen CH, Yueh SK. Double-balloon enteroscopy application in biliary tract disease-its therapeutic and diagnostic functions. Gastrointest Endosc. 2008;68:585-591. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 68] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 62. | Koornstra JJ. Double balloon enteroscopy for endoscopic retrograde cholangiopancreaticography after Roux-en-Y reconstruction: case series and review of the literature. Neth J Med. 2008;66:275-279. [PubMed] [Cited in This Article: ] |
| 63. | Emmett DS, Mallat DB. Double-balloon ERCP in patients who have undergone Roux-en-Y surgery: a case series. Gastrointest Endosc. 2007;66:1038-1041. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 150] [Cited by in F6Publishing: 160] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 64. | Mönkemüller K, Bellutti M, Neumann H, Malfertheiner P. Therapeutic ERCP with the double-balloon enteroscope in patients with Roux-en-Y anastomosis. Gastrointest Endosc. 2008;67:992-996. [PubMed] [Cited in This Article: ] |
| 65. | Haruta H, Yamamoto H, Mizuta K, Kita Y, Uno T, Egami S, Hishikawa S, Sugano K, Kawarasaki H. A case of successful enteroscopic balloon dilation for late anastomotic stricture of choledochojejunostomy after living donor liver transplantation. Liver Transpl. 2005;11:1608-1610. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 96] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 66. | Aabakken L, Bretthauer M, Line PD. Double-balloon enteroscopy for endoscopic retrograde cholangiography in patients with a Roux-en-Y anastomosis. Endoscopy. 2007;39:1068-1071. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 146] [Cited by in F6Publishing: 145] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 67. | Spahn TW, Grosse-Thie W, Spies P, Mueller MK. Treatment of choledocholithiasis following Roux-en-Y hepaticojejunostomy using double-balloon endoscopy. Digestion. 2007;75:20-21. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 68. | Chahal P, Baron TH, Poterucha JJ, Rosen CB. Endoscopic retrograde cholangiography in post-orthotopic liver transplant population with Roux-en-Y biliary reconstruction. Liver Transpl. 2007;13:1168-1173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 59] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 69. | Neumann H, Fry LC, Meyer F, Malfertheiner P, Monkemuller K. Endoscopic retrograde cholangiopancreatography using the single balloon enteroscope technique in patients with Roux-en-Y anastomosis. Digestion. 2009;80:52-57. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 70. | Raithel M, Dormann H, Naegel A, Boxberger F, Hahn EG, Neurath MF, Maiss J. Double-balloon-enteroscopy-based endoscopic retrograde cholangiopancreatography in post-surgical patients. World J Gastroenterol. 2011;17:2302-2314. [PubMed] [Cited in This Article: ] |
| 71. | Cohan RH, Illescas FF, Saeed M, Perlmutt LM, Braun SD, Newman GE, Dunnick NR. Infectious complications of percutaneous biliary drainage. Invest Radiol. 1986;21:705-709. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 25] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 72. | Hamlin JA, Friedman M, Stein MG, Bray JF. Percutaneous biliary drainage: complications of 118 consecutive catheterizations. Radiology. 1986;158:199-202. [PubMed] [Cited in This Article: ] |
| 73. | Farrell J, Carr-Locke D, Garrido T, Ruymann F, Shields S, Saltzman J. Endoscopic retrograde cholangiopancreatography after pancreaticoduodenectomy for benign and malignant disease: indications and technical outcomes. Endoscopy. 2006;38:1246-1249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 74. | May A, Nachbar L, Pohl J, Ell C. Endoscopic interventions in the small bowel using double balloon enteroscopy: feasibility and limitations. Am J Gastroenterol. 2007;102:527-535. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 168] [Cited by in F6Publishing: 166] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 75. | Mehdizadeh S, Han NJ, Cheng DW, Chen GC, Lo SK. Success rate of retrograde double-balloon enteroscopy. Gastrointest Endosc. 2007;65:633-639. [PubMed] [Cited in This Article: ] |
| 76. | Gerson LB, Tokar J, Chiorean M, Lo S, Decker GA, Cave D, Bouhaidar D, Mishkin D, Dye C, Haluszka O. Complications associated with double balloon enteroscopy: The US experience. Am J Gastroenterol. 2008;103:A283. [Cited in This Article: ] |
| 77. | Ross AS, Waxman I, Semrad C, Dye C. Balloon-assisted intubation of the ileocecal valve to facilitate retrograde double-balloon enteroscopy. Gastrointest Endosc. 2005;62:987-988. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 78. | Raksakietisak M. Unrecognised aspiration pneumonitis during enteroscopy: two cases report. J Med Assoc Thai. 2009;92:869-871. [PubMed] [Cited in This Article: ] |
| 79. | Tanaka S, Mitsui K, Yamada Y, Ehara A, Kobayashi T, Seo T, Tatsuguchi A, Fujimori S, Gudis K, Sakamoto C. Diagnostic yield of double-balloon endoscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2008;68:683-691. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 72] [Article Influence: 4.5] [Reference Citation Analysis (0)] |