Published online Jul 16, 2014. doi: 10.4253/wjge.v6.i7.328
Revised: April 25, 2014
Accepted: June 10, 2014
Published online: July 16, 2014
Intraductal papillary mucinous neoplasm (IPMN) of the bile duct is still rare and not yet understood despite of its increased incidence and similar clinicopathologic characteristics compared with IPMN of the pancreas. The fistula formation into other organs can occur in IPMN, especially the pancreatic type. To our knowledge, only two cases of IPMN of the bile duct with a choledochoduodenal fistula were reported and we have recently experienced a case of IPMN of the bile duct penetrating into two neighboring organs of the stomach and duodenum presenting with abdominal pain and jaundice. Endoscopy showed thick mucin extruding from two openings of the fistulas. Endoscopic suction of thick mucin using direct peroral cholangioscopy with ultra-slim endoscope through choledochoduodenal fistula was very difficult and ineffective because of very thick mucin and next endoscopic suction through the stent after prior insertion of biliary metal stent into choledochogastric fistula also failed. Pathologic specimen obtained from the proximal portion of the choledochogastric fistula near left intrahepatic bile duct through the metal stent showed a low grade adenoma. The patient declined the surgical treatment due to her old age and her abdominal pain with jaundice was improved after percutaneous transhepatic biliary drainage with the irrigation of N-acetylcysteine three times daily for 10 d.
Core tip: An intraductal papillary mucinous neoplasm of the bile duct with combined fistula formation into the stomach and the duodenum initially presented with jaundice and abdominal pain was introduced and after failed attempts of endoscopic suction of thick mucin through the two fistulas to resolve the jaundice, the patient’s symptom was successfully resolved after the irrigations of N-acetylcysteine three times daily via after percutaneous transhepatic biliary drainage tube for 10 d.
- Citation: Hong MY, Yu DW, Hong SG. Intraductal papillary mucinous neoplasm of the bile duct with gastric and duodenal fistulas. World J Gastrointest Endosc 2014; 6(7): 328-333
- URL: https://www.wjgnet.com/1948-5190/full/v6/i7/328.htm
- DOI: https://dx.doi.org/10.4253/wjge.v6.i7.328
Intraductal papillary mucinous neoplasm (IPMN) of the bile duct has been suggested to be the biliary counterpart of IPMN of the pancreas after wide acceptance of the nomenclature by the World Health Organization[1]. It represents a disease spectrum from benign to malignant and affected bile ducts exhibit marked dilatation because of mucin hypersecretion. Jaundice with cholangitis is sometimes complicated by the presence of intraductal tumor with tenacious mucoid impaction[2,3]. The fistula from penetration into other neighboring organs can be caused by high pressure due to mucin-filling of bile ducts and inflammatory stimulation[4]. IPMN of the bile duct with fistula formation into surrounding organs was relatively rare presentation compared with its pancreatic counterpart and to our best knowledge, only two cases of IPMN with the bile duct with one fistula into other organs were reported in the English literature[5,6] and here, we describe the first case of biliary IPMN with two fistulas into the stomach and duodenum.
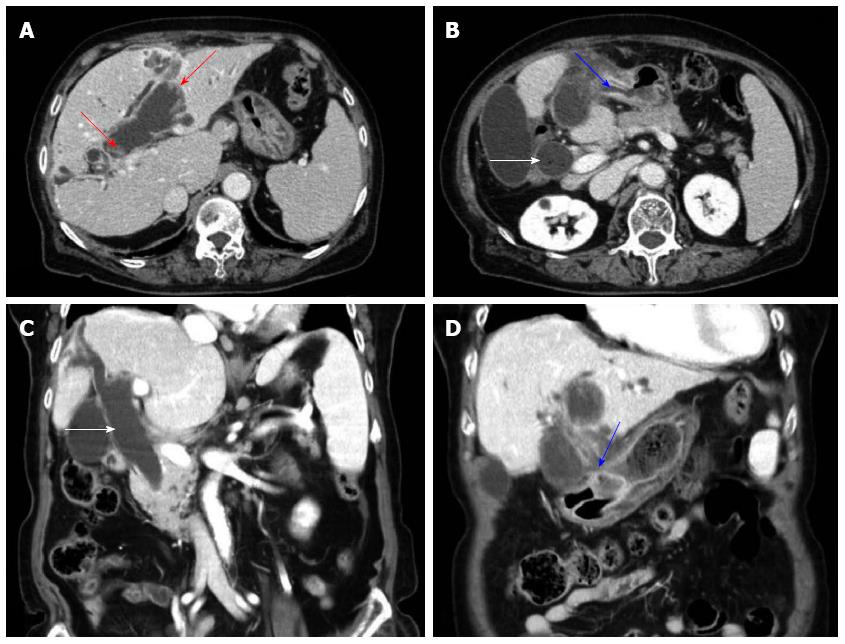
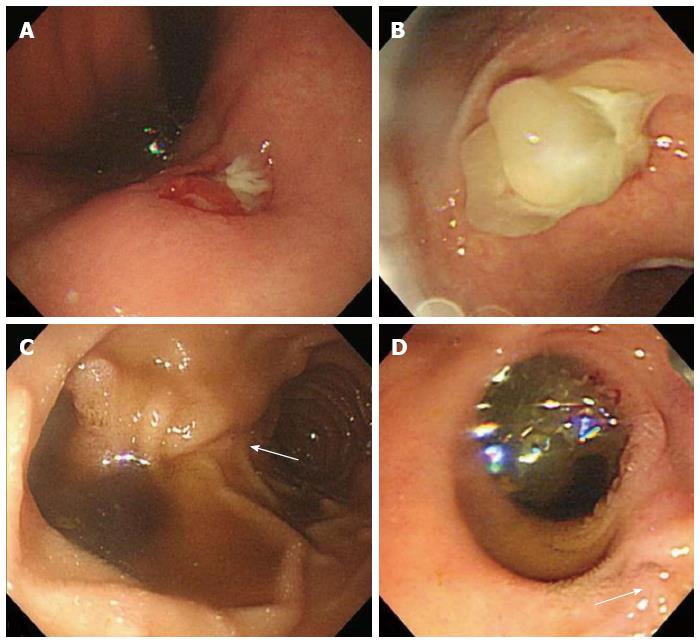
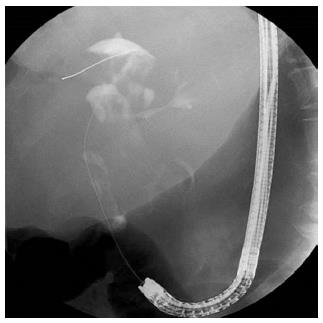
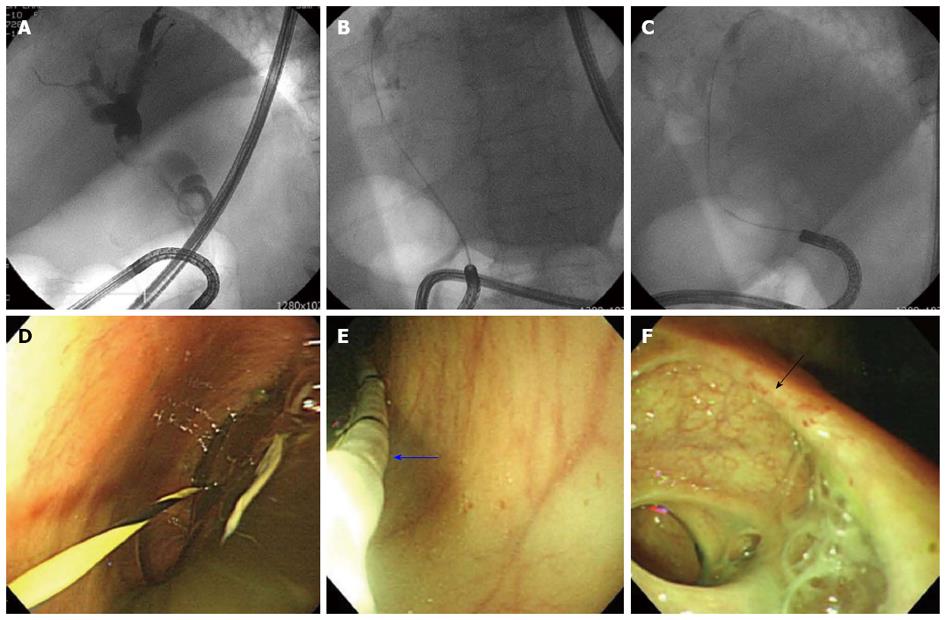
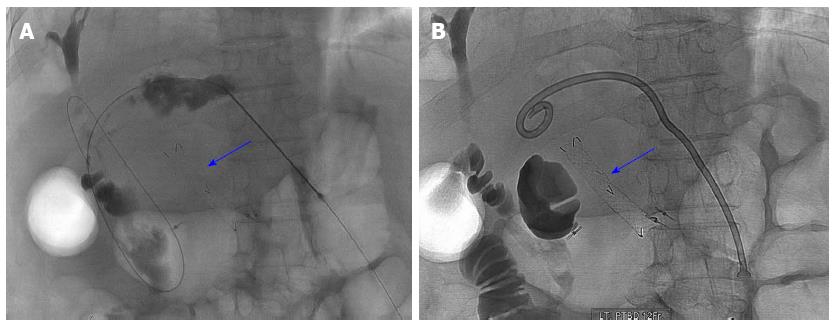
An 87-year-old woman was admitted to our hospital because of acute right upper quadrant abdominal pain. On physical examination, palpable mass and tenderness of upper abdomen was noted. The complete blood count results showed white blood cell count of 3630/mm3, hemoglobin of 7.8 g/dL, and platelet count of 188000/mm3. The blood chemistry analysis showed total protein of 8.6 g/dL, albumin of 3.3 g/dL, total bilirubin of 2.7 mg/dL, aspartate aminotransferase of 29 U/L, alanine aminotransferase of 36 U/L, alkaline phosphatase of 249 IU/L, gamma-glutamyltransferase of 105 U/L, creatinine of 0.9 mg/dL, amylase of 45 U/L, and lipase of 35.6 U/L. Serum tumor markers of serum alpha-fetoprotein, CA19-9 and carcinoembryonic antigen were 1.9 ng/mL, < 2.0 U/mL and 7.5 ng/mL, respectively. Computed tomography (CT) of the abdomen showed markedly dilated common bile duct (CBD) and left intrahepatic duct (IHD) with left IHD penetrating into the antrum of stomach and fistula formation and no definite visible mass in left IHD (Figure 1). Endoscopy showed a round ulcerated lesion and extruding white thick mucin from the opening at the lesser curvature of the antrum during endoscopic suction and another wide opening of the fistula with mucin excretion proximal to the original papillary orifice (Figure 2). Cholangiogram obtained from the duodenal fistula near the papillary orifice showed moderately to severely dilated CBD and proximal left IHD with amorphous, partial intraluminal filling of the contrast in the bile duct (Figure 3). The lesion was strongly suspicious of IPMN of the bile duct with combined choledochogastric and choledochoduodenal fistulas. Four days after admission, serum bilirubin increased up to 5.0 mg/dL. Endoscopic suction to extract mucin to relieve jaundice caused by biliary mucinous obstruction and biopsy from the lesion of left IHD were planned using direct peroral cholangioscopy with ultra-slim endoscope (Olympus), but the removal of mucin by endoscopic suction with standard upper endoscope or ultra-slim endoscope was very difficult and failed because of very thick and high viscous mucin (Figure 4). And then, a partially covered metal stent was inserted through the choledochogastric fistula and endoscopic suction through the stent with ultra-slim endoscope also failed due to very thick mucin (blue arrow, Figure 5). Despite of approaching up to common hepatic duct level with ultra-slim endoscope through the choledochoduodenal fistula, target biopsy was not performed due to physical obstacle of large amount of very thick mucin, but instead, specimens were obtained from the proximal site of the fistula near left IHD through the metal stent in choledochogastric fistula and additional biopsy at the distal site of the choledochogastric fistula near the gastric antrum were done. Serum bilirubin level was increased up to 6.0 mg/dL next day, but the patient refused surgical intervention and continued to complain abdominal pain and jaundice.
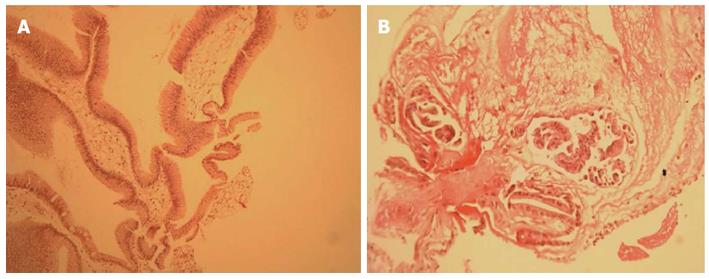
After insertion of percutaneous transhepatic biliary drainage (PTBD) catheter (Figure 5), the irrigations of N-acetylcysteine (300 mg) via the catheter three times a day for 10 d, abdominal pain resolved with decreased serum bilirubin level to 1.0 mg/dL and she was discharged with keeping the PTBD catheter and drainage bag. Pathology showed a low grade dysplasia from the proximal site of the choledochogatric fistula near the left IHD (Figure 6) and non-specific inflammation from the distal site of the fistula near the gastric antrum. She was still alive until recently during the follow-up period of 15 mo.
IPMN of the pancreas was first reported by Ohhashi et al[7] in 1982 and the clinical features are secretion of large amount of mucin by papillary neoplasm, dilatation of the main pancreatic duct or its branch ducts, slow growth with favorable prognosis, and chronic vague abdominal pain. The pathologic feature of the IPMN of the pancreas reveals the presence of a macroscopic intraluminal lesion and visible mucin on the surface of the tumor with solitary or diffuse intraductal growth[8]. IPMN of the bile duct is a variant of the bile duct malignancy and has a similar clinicopathologic features as its pancreatic counterpart because both the bile ducts and the pancreas develop from the ventral endoderm, although IPMN of the bile duct is associated with higher malignancy rate at the time of surgery than its pancreatic counterpart[9,10]. IPMN sometimes represents expansive progression with mucus extrusion and occasionally make a fistula penetrating into other organs. Fistula formation is divided into two types based on the mechanism, invasive penetration by malignant invasion and mechanical penetration by mucin extrusion with duct expansion[7].
In our case, the choledochogastric fistula formation was highly suggestive of mechanical penetration in that the specimen obtained from the distal part of the fistula near the stomach histologically showed non-specific inflammation, while the proximal part near the left IHD showed low grade adenoma.
The consensus guidelines for management of IPMN of the pancreas was well established since 2006, meanwhile, there has no published literature for making the accurate diagnosis and proper management of IPMN of the bile duct[11]. Although the majority of malignant IPMN of the bile duct demonstrates tumors or mural nodule in the bile ducts, in some cases the tumor is not visible in images or even in gross specimens and moderately to severely dilatation of the bile duct with mucobilia is the only finding like our case[2]. The diagnosis of IPMN of the bile duct was based on multimodality assessment of various imaging techniques. Ultrasonography is initial examination of biliary dilatation and stenosis with viscous mucin as fine echogenic findings. CT with magnetic resonance imaging have better delineation of biliary dilatation with tumor location, extent and volume (stage). ERCP is a relatively invasive examination and shows mucobilia as a filling defect of contrast in bile duct and endoscopic ultrasound (EUS) can be used for detecting mural nodule or solid mass with local invasion and cytological analysis obtained by fine needle aspiration[1,3,11]. EUS examination was not performed in our patient because of no visible mass in the CT and ERCP findings.
The insertion of multiple uncovered metal stents has been shown to be feasible in the patients of IPMN of the pancreas with biliary obstruction by mucoid impaction[12], but the insertion of multiple metal stents alongside each other to facilitate biliary drainage could not apply to the patient of severely dilated bile duct with thick mucoid impaction and no specific stenosis like our case.
The mucolysis of antioxidant N-acetylcysteine (NAC) was widely used in the management of the symptom of the chronic obstructive pulmonary disease and other respiratory conditions such as idiopathic pulmonary fibrosis[13,14] and the usefulness of the dissolution of the renal stone by the irrigation with NAC via percutaneous nephrostomy was reported[15]. A case of the effectiveness of infusion of NAC through nasobiliary catheter for advanced biliary IPMN was recently reported[16]. In our case, the bilirubin level and her abdominal pain was improved by the intermittent infusions of NAC (300 mg) three times a day for 10 d through the PTBD catheter. Choledoscopy via PTBD after resolution of abdominal pain and jaundice with multiple irrigations of NAC was intended for further detailed examination of IHD, but she denied and only request symptom relief.
In summary, IPMN of bile duct with combined two fistulas into the stomach and the duodenum presented with abdominal pain and ongoing jaundice due to thick mucoid impaction in the bile duct was successfully treated with the irrigation with NAC for 10 d.
The patient presented with abdominal pain and jaundice.
Intraductal papillary mucinous neoplasm (IPMN) of the bile duct with combined fistulas of the stomach and the duodenum.
Mucin-producing cholangiocarcinoma or biliary papilloma(tosis) or papillary cholangiocarcinoma were considered because of mucin hypersecretion and moderately to severely dilation of the bile duct on imaging studies.
Acute cholangitis accompanied with IPMN of the bile duct was based on fact that initial serum total bilirubin level was 2.7 mg/dL and reached up to 6 mg/dL six days after admission.
IPMN of the bile duct with combined fistulas of the stomach and the duodenum was based on multimodality imaging and endoscopic finding.
Histologic finding of the specimen obtained from left intrahepatic bile duct through the inserted metal stent in choledochogastric fistula showed IMPN of the bile duct with low grade dysplasia.
The patient’s abdominal pain with jaundice was settled after the multiple irrigations of N-acetylcysteine (NAC) through percutaneous transhepatic biliary drainage (PTBD) catheter for 10 d.
Two case reports of IPMN of the bile duct accompanied with choledochoduodenal fistula published in English were shown in references 5, 6.
Clinicians should consider that multiple irrigations of NAC via PTBD tube is an alternative therapeutic option for IPMN of the bile duct with thick mucoid impaction accompained with cholangitis after failed endoscopic suction of mucin.
The authors presented a rare, interesting case of IPMB with combined fistula formation into the stomach and the duodenum. This case is very interesting.
P- Reviewers: Ogura T, Moon JH S- Editor: Song XX L- Editor: A E- Editor: Zhang DN
| 1. | Takanami K, Yamada T, Tsuda M, Takase K, Ishida K, Nakamura Y, Kanno A, Shimosegawa T, Unno M, Takahashi S. Intraductal papillary mucininous neoplasm of the bile ducts: multimodality assessment with pathologic correlation. Abdom Imaging. 2011;36:447-456. [Cited in This Article: ] |
| 2. | Lim JH, Jang KT, Choi D. Biliary intraductal papillary-mucinous neoplasm manifesting only as dilatation of the hepatic lobar or segmental bile ducts: imaging features in six patients. AJR Am J Roentgenol. 2008;191:778-782. [Cited in This Article: ] |
| 3. | Yeh TS, Tseng JH, Chiu CT, Liu NJ, Chen TC, Jan YY, Chen MF. Cholangiographic spectrum of intraductal papillary mucinous neoplasm of the bile ducts. Ann Surg. 2006;244:248-253. [Cited in This Article: ] |
| 4. | Yamada Y, Mori H, Hijiya N, Matsumoto S, Takaji R, Ohta M, Kitano S, Moriyama M. Intraductal papillary mucinous neoplasms of the pancreas complicated with intraductal hemorrhage, perforation, and fistula formation: CT and MR imaging findings with pathologic correlation. Abdom Imaging. 2012;37:100-109. [Cited in This Article: ] |
| 5. | Barresi L, Tarantino I, Granata A, Curcio G, Gentile R, Liotta R, Marrone G, Traina M. Biliary intraductal papillary mucinous neoplasm visualized intralesionally through a fistula with the duodenal bulb. Endoscopy. 2012;44 Suppl 2 UCTN:E84-E85. [Cited in This Article: ] |
| 6. | Kim HT, Kim SI, Kwon OW, Lee HL, Jun DW, Lee OY, Choi HS. Intraductal Papillary Mucinous Neoplasm of the Bile Ducts Accompanied by a Choledochoduodenal Fistula. Korean J Med. 2011;81:93-97. [Cited in This Article: ] |
| 7. | Kobayashi G, Fujita N, Noda Y, Ito K, Horaguchi J, Obana T, Koshida S, Kanno Y, Yamashita Y, Kato Y. Intraductal papillary mucinous neoplasms of the pancreas showing fistula formation into other organs. J Gastroenterol. 2010;45:1080-1089. [Cited in This Article: ] |
| 8. | Barton JG, Barrett DA, Maricevich MA, Schnelldorfer T, Wood CM, Smyrk TC, Baron TH, Sarr MG, Donohue JH, Farnell MB. Intraductal papillary mucinous neoplasm of the biliary tract: a real disease? HPB (Oxford). 2009;11:684-691. [Cited in This Article: ] |
| 9. | Kloek JJ, van der Gaag NA, Erdogan D, Rauws EA, Busch OR, Gouma DJ, ten Kate FJ, van Gulik TM. A comparative study of intraductal papillary neoplasia of the biliary tract and pancreas. Hum Pathol. 2011;42:824-832. [Cited in This Article: ] |
| 10. | Rocha FG, Lee H, Katabi N, DeMatteo RP, Fong Y, D’Angelica MI, Allen PJ, Klimstra DS, Jarnagin WR. Intraductal papillary neoplasm of the bile duct: a biliary equivalent to intraductal papillary mucinous neoplasm of the pancreas? Hepatology. 2012;56:1352-1360. [Cited in This Article: ] |
| 11. | Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, Kimura W, Levy P, Pitman MB, Schmidt CM. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183-197. [Cited in This Article: ] |
| 12. | Seynaeve L, Van Steenbergen W. Treatment, by insertion of multiple uncovered metallic stents, of intraductal papillary mucinous neoplasm of the pancreas with biliary obstruction by mucus impaction. Pancreatology. 2007;7:540-543. [Cited in This Article: ] |
| 13. | Demedts M, Behr J, Buhl R, Costabel U, Dekhuijzen R, Jansen HM, MacNee W, Thomeer M, Wallaert B, Laurent F. High-dose acetylcysteine in idiopathic pulmonary fibrosis. N Engl J Med. 2005;353:2229-2242. [Cited in This Article: ] |
| 14. | Sadowska AM. N-Acetylcysteine mucolysis in the management of chronic obstructive pulmonary disease. Ther Adv Respir Dis. 2012;6:127-135. [Cited in This Article: ] |
| 15. | Egghart G, Marquardt HD, Kastert HB, Feizelmeier F. Percutaneous nephrostomy and irrigation lithochemolysis. A new concept for the treatment of cystine stones. Int Urol Nephrol. 1983;15:131-136. [Cited in This Article: ] |
| 16. | Hu LH, Liu MH, Liao Z, Zou WB, Ye B, Wang L, Li ZS. Continuous infusion of N-acetylcysteine by nasobiliary for advanced intraductal papillary mucinous neoplasm of bile ducts (with video). Am J Gastroenterol. 2012;107:1929-1930. [Cited in This Article: ] |