Published online Aug 26, 2011. doi: 10.4330/wjc.v3.i8.267
Revised: June 16, 2011
Accepted: June 23, 2011
Published online: August 26, 2011
AIM: To describe the characteristics of coronary artery fistulas (CAFs) in adults, including donor vessels and whether termination was cameral or vascular.
METHODS: A PubMed search was performed for articles between 2000 and 2010 to describe the current characteristics of congenital CAFs in adults. A group of 304 adults was collected. Clinical data, presentations, diagnostic modalities, angiographic fistula findings and treatment strategies were gathered and analyzed. With regard to CAF origin, the subjects were tabulated into unilateral, bilateral or multilateral fistulas and compared. The group was stratified into two major subsets according to the mode of termination; coronary-cameral fistulas (CCFs) and coronary-vascular fistulas (CVFs). A comparison was made between the two subsets. Fistula-related major complications [aneurysm formation, infective endocarditis (IE), myocardial infarction (MI), rupture, pericardial effusion (PE) and tamponade] were described. Coronary artery-ventricular multiple micro-fistulas and acquired CAFs were excluded as well as anomalous origin of the coronary arteries from the pulmonary artery (PA).
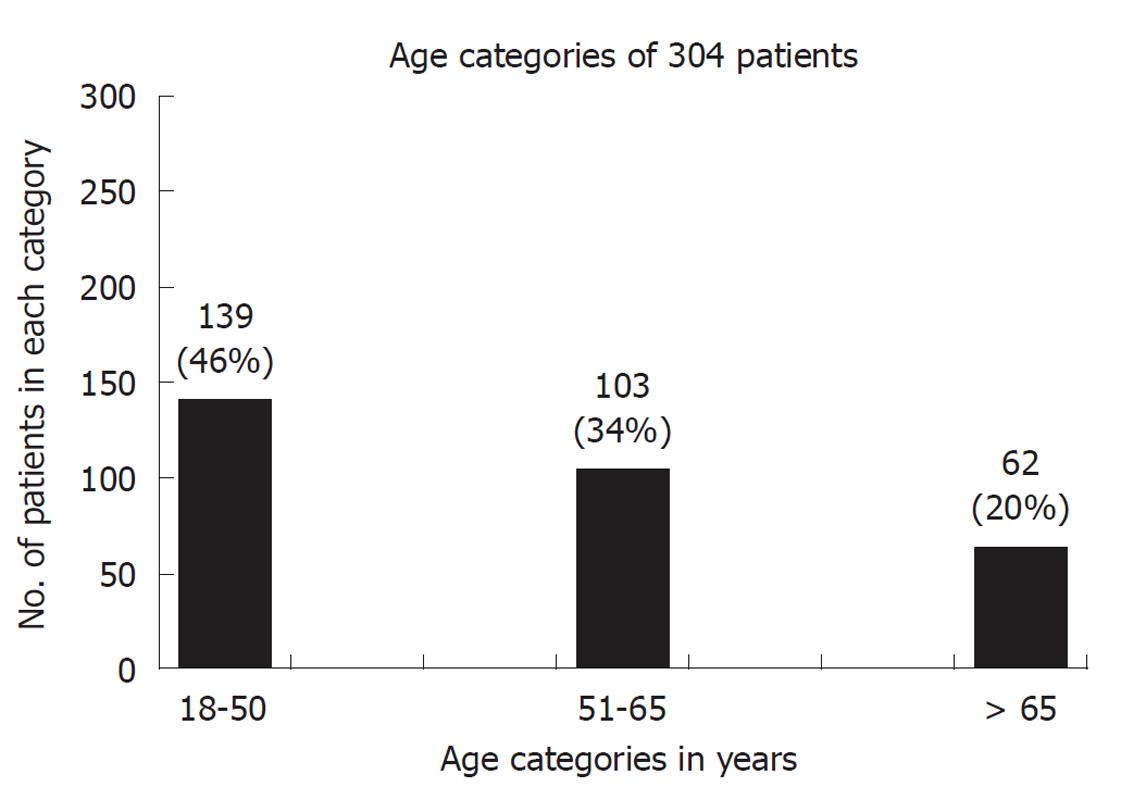
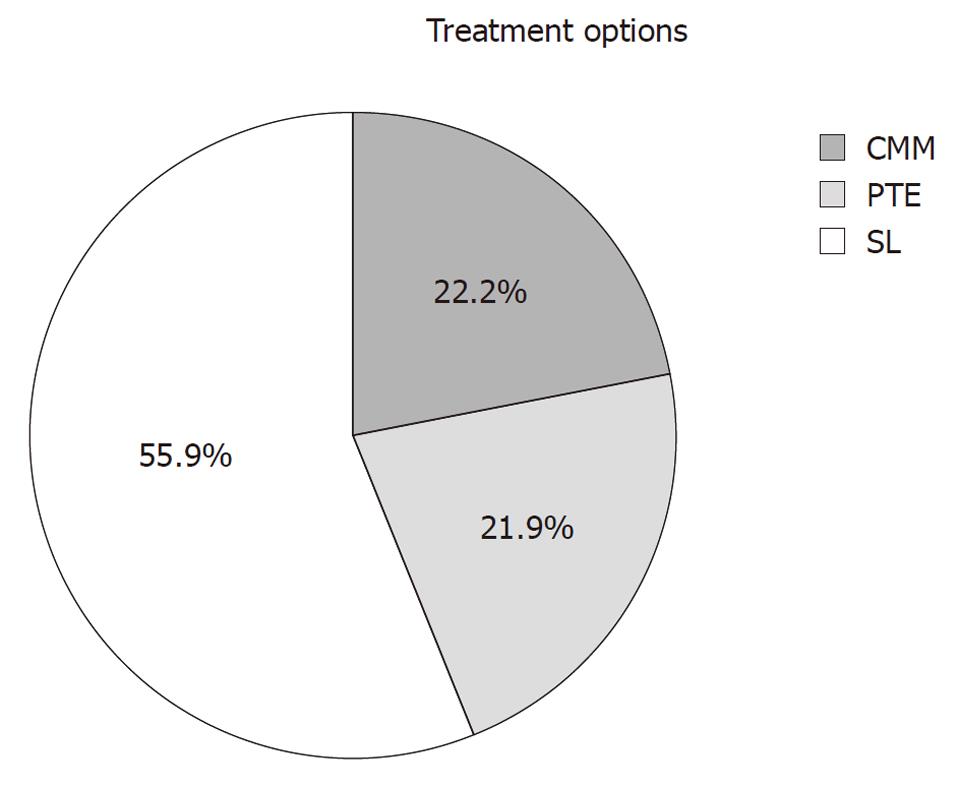
RESULTS: A total of 304 adult subjects (47% male) with congenital CAFs were included. The mean age was 51.4 years (range, 18-86 years), with 20% older than 65 years of age. Dyspnea (31%), chest pain (23%) and angina pectoris (21%) were the prevalent clinical presentations. Continuous cardiac murmur was heard in 82% of the subjects. Of the applied diagnostic modalities, chest X-ray showed an abnormal shadow in 4% of the subjects. The cornerstone in establishing the diagnosis was echocardiography (68%), and conventional contrast coronary angiography (97%). However, multi-slice detector computed tomography was performed in 16%. The unilateral fistula originated from the left in 69% and from the right coronary artery in 31% of the subjects. Most patients (80%) had unilateral fistulas, 18% presented with bilateral fistulas and 2% with multilateral fistulas. Termination into the PA was reported in unilateral (44%), bilateral (73%) and multilateral (75%) fistulas. Fistulas with multiple origins (bilateral and multilateral) terminated more frequently into the PA (29%) than into other sites (10.6%) (P = 0.000). Aneurysmal formation was found in 14% of all subjects. Spontaneous rupture, PE and tamponade were reported in 2% of all subjects. In CCFs, the mean age was 46.2 years whereas in CVFs mean age was 55.6 years (P = 0.003). IE (4%) was exclusively associated with CCFs, while MI (2%) was only found in subjects with CVFs. Surgical ligation was frequently chosen for unilateral (57%), bilateral (51%) and multilateral fistulas (66%), but percutaneous therapeutic embolization (PTE) was increasingly reported (23%, 17% and 17%, respectively).
CONCLUSION: Congenital CAFs are currently detected in elderly patients. Bilateral fistulas are more frequently reported and PTE is more frequently applied as a therapeutic strategy in adults.
- Citation: Said SA. Current characteristics of congenital coronary artery fistulas in adults: A decade of global experience. World J Cardiol 2011; 3(8): 267-277
- URL: https://www.wjgnet.com/1949-8462/full/v3/i8/267.htm
- DOI: https://dx.doi.org/10.4330/wjc.v3.i8.267
Nowadays congenital coronary artery fistulas (CAFs) in adults are frequently non-invasively[1-4], semi-invasively[5-8] and invasively[9] detected because of the rapid advent of various imaging modalities. With these advanced diagnostic techniques many unilateral[10-15], bilateral[16-20] and multilateral[21] fistulas have been diagnosed. Many reports from various parts of the world recording congenital CAFs in adults have been published during the last decade[22-28]. The pertinent diagnosis of congenital CAFs in adults has been published from different regions of the world[29-36]. A review of the world literature resulting in 304 patients between 2000 and 2010 to identify the current characteristics of congenital CAFs in adults is presented, and the important findings are discussed.
PubMed was searched for terms “coronary artery” and “fistulas” combined with “congenital” and “adult”. From the English and non-English medical literature, only relevant publications regarding congenital CAFs in adults were chosen and considered for analysis and evaluation. The search was conducted for the period from 2000 to 2010. Coronary artery-ventricular multiple micro-fistulas and acquired CAFs, as well as cases of anomalous origin of the coronary arteries from the pulmonary artery (PA) were excluded. Papers with a mixed population (pediatric and adult) or with pediatric subjects alone were excluded. Papers and data were carefully examined for completeness. The following criteria for CAFs were stipulated to include homogenous subsets for analysis: origin and number of donor vessels (unilateral, bilateral and multilateral) and mode of termination [coronary-cameral fistula (CCF) vs coronary-vascular fistula (CVF)]. Patients were tabulated according to the origin from the right or left coronary arteries or their branches, or from the right or left sinus of Valsalva and number of the fistulas with regard to their characteristics [from the left main trunk (LMT), left anterior descending (LAD), circumflex coronary artery (Cx), right coronary artery (RCA), left coronary artery (LCA), unilateral, bilateral or multilateral fistulas]. A number of parameters were examined for comparison, such as mean age, gender, clinical presentation, fistula characteristics and complications. The following question was addressed in this review: do different age groups in the adult population with congenital CAFs differ in clinical presentation, fistula characteristics and treatment modalities?
CCFs: The fistula terminates into a cardiac chamber (right atrium (RA)/coronary sinus (CS), right ventricle (RV), left atrium (LA) and left ventricle (LV).
CVFs: The fistula terminates into a thoracic vessel [PA, superior vena cava (SVC), pulmonary veins (PV), bronchial and cardiac veins and right ventricular outflow tract (RVOT)].
These definitions were adopted and modified from Gupta-Malhotra[37].
Data and categorical variables are presented as counts and percentages and continuous variables are expressed as mean. Statistical analysis was performed by using the two-tailed paired Student t-test and Chi-square test. A P value < 0.05 was considered significant. Statistical analyses were performed using SPSS version 18.0 (SPSS Inc., USA).
Characteristics of 304 patients between 2000 and 2010 were collected. Of this group, 47% were male, mean age was 51.4 years (range, 18-86 years). The majority (46%) of patients were aged 18-50 years but a considerable proportion (20%) were older than 65 years (Figure 1). The fistulas were multilateral in 6 (2%) patients, bilateral in 55 (18%) and unilateral in 243 (80%). The origin of the unilateral fistulas was from the LCA in 69% [LMT (7%), LAD (42%), Cx (20%)] and RCA in 31% (Table 1).
| Origin | LMT (n = 17) (7%) | LAD (n = 102) (42%) | Cx (n = 48) (20%) | RCA (n = 76) (31%) |
| Termination | ||||
| PA | 47% | 75% | 23% | 16% |
| RA/CS | 29% | 7% | 52% | 37% |
| RV | 6% | 9% | 4% | 25% |
| SVC | 12% | none | 6% | 5% |
| LV | none | 3% | 4% | 12% |
| Aneurysm | 18% | 7% | 17% | 17% |
| Management | ||||
| SL | 47% | 63% | 52% | 54% |
| CMM | 41% | 13% | 31% | 17% |
| PTE | 12% | 24% | 17% | 29% |
Thirty-five patients (11%) were asymptomatic. In 11 (4%) patients, the clinical presentation was not recorded and 85% of patients were symptomatic. The major presentations were composed of a single symptom in 63% and 37% presented with multiple symptoms. These were, in decreasing order of frequency, dyspnea (31%), chest pain (23%) and angina pectoris (21%). Moreover, palpitation was a commonly reported symptom occurring in 13%, congestive heart failure (CHF) in 8%, infective endocarditis (IE) in 4%, and abnormal shadow on chest X-ray in 4% of patients. Furthermore, fatigue was reported in 6% of patients, atrial fibrillation in 5%, syncope in 4%, pericardial effusion (PE) in 2% and myocardial infarction (MI) in 2%. Ventricular and supra-ventricular tachycardia were very rarely seen.
CHF: Overt CHF was reported in 8% of patients, 70% of whom were female. The mean age was 60.6 years (range, 27-86 years). In these patients, the mean ratio of the left-to-right shunt (Qp:Qs) was 1.8 (range, 1.2-2.7). The mean systolic PA pressure was elevated at 47 mmHg (varying from 25/9 to 61/24 mmHg), compatible with mild pulmonary hypertension. Unilateral fistulas were predominant, being present in 19/23 (83%) of patients, and bilateral in 4/23 (17%). The origin was the LCA in 21/27 (78%) and the RCA in 6/27 (22%) of the fistulas. The therapeutic management of this sub-group was surgical ligation (SL) in 14 patients, percutaneous therapeutic embolization (PTE) in 5 patients and conservative medical management (CMM) in 4 patients.
IE: IE was reported in 11/304 patients (4%), 36% of whom were female. All had CCFs where fistulas arose from right or left coronary arteries having a unilateral[1,38-41] or bilateral[1,42] origin. The termination site was always a cardiac chamber either right- or left-sided: RA[38,41], RV[1], CS[39,40,42,43] or LA[1]. Streptococcus[38,42,44] and Staphylococcus species[40] were isolated from blood cultures. Echocardiography demonstrated aneurysmal dilatation of the donor vessels[43-45], and recipient chamber[42,45], and valvular[44,45] and non-valvular[42,44] vegetation. Furthermore, there was moderate and severe valvular regurgitation with ruptured chordae[1,39]. Non-valvular vegetation was located in the inferior atriocaval junction[38] and CS[40,42,44]. Turbulent flow in the recipient chamber was noted by color Doppler[40,45]. Associated congenital and acquired heart defects (single coronary artery, bicuspid aortic valve and atrio-ventricular valvular heart disease) were also visualized[1,2,41]. All patients were treated surgically, but two were managed conservatively. IE has been reported to occur in the clinical history of patients with CAFs[46].
MI: Both ipsilateral (4 ×) and contralateral (1 ×) to the shunt, infarctions (2%) were reported only in patients with CVFs where the fistulas communicated to the right or left side of the vascular system; PA[9,27,47-49], SVC[10,50], RVOT[12,51] and PV[52]. The mean age was 60.8 years (range, 51-78 years). They were 2 females and 3 males. Significant coronary artery disease was present in 2 patients and 3 were free of atherosclerotic lesions. A unilateral fistula was found in 2 and bilateral fistulas in 3 patients. Of the 3 patients with bilateral fistulas (LAD-RCA), one had inferolateral MI, one developed inferior MI and the third presented with anterior MI. A myocardial perfusion test revealed reversible ischemia in 2 and was negative in one. Medical treatment of the fistula was conducted in 3, PTE in one and SL in one of the patients. PCI was performed in a non-fistula vessel in 2 patients. No infarct-related complications were described.
Cardiac murmur: Cardiac murmur was reported in (47%) of patients. Of those, continuous heart murmur was heard in (82%), systolic murmur in (11%) and diastolic murmur in (7%). No murmur was heard in (53%). Only few patients had two different cardiac murmurs.
Abnormal shadow on chest X-ray: The chest X-ray demonstrated a marked abnormal shadow in 11/304 (4%) patients; unilateral in 8 (5 LCA, 3 RCA) and bilateral in 4 (LAD-RCA). The LCA participated in the formation of the fistula in the majority of fistulas (9/16) with an abnormal shadow on the chest X-ray on either unilateral[53,54] or bilateral fistulas[55-58]. The RCA was involved in fistula formation in 7/16 (44%) patients. Termination occurred into the PA in 9/12 (75%) patients, into the CS in one (8%), into the RA in one (8%) and into the LA in one (8%). All fistulas were associated with an aneurysm. Three-quarters of the patients (9/12) were treated surgically, (8%) PTE was performed in one and 2 (17%) were followed with CMM.
For the morphological, anatomical visualization, and functional assessment of CAFs, different diagnostic modalities separately or combined were applied to confirm the presence of unilateral[12,13,59-61], bilateral[16,19,30,48,62], or multilateral[6,21,63] CAFs. In the reviewed group, the cornerstone in establishing the diagnosis was conventional coronary angiography (CAG) (97%) and echocardiography (68%). However, multi-slice detector computed tomography (MDCT) is slowly gaining popularity, and was applied in (16%) of reviewed patients. In the current review, associated congenital and acquired heart disease was present in 22% compared with 13% in a previous review in 2006[64].
Doppler echocardiography remains of great diagnostic value in the detection, intra-operative imaging and follow-up of patients with CAFs[2,22]. CAFs could be suspected[7,8] and confirmed[51,65,66] by echocardiography, as well as demonstration of dilatation and aneurysm of the donor vessel[34,36,67-70] and dilatation of the recipient chamber[3,4,71-73]. Thrombotic or vascular masses have been visualized by echocardiography[72]. Abnormal flow by color Doppler imaging provided a direct clue in the diagnosis of fistulous communication[74-79]. Furthermore, turbulent blood flow may be seen in the dilated recipient cardiac chamber[2]. In cases of IE associated with CAFs, valvular[44,45] and non-valvular[42,44] vegetations have been described. Echocardiographic examination showed a variety of associated congenital and acquired heart defects[2,3,51,80]. By means of echocardiography, right-sided pressure could be estimated and the left-to-right shunt (ratio of pulmonary to systemic blood flow) could be calculated[24,47,51,81,82]. Rupture of an aneurysm associated with CAFs causing PE and tamponade was easily illustrated by echocardiography[15,83,84].
Angiographic fistula characteristics related to the origin and number of donor vessels: Unilateral fistulas were found in 80% of subjects (Table 1). An origin from the LMT was reported infrequently in 17 patients in total (7%). The fistulas terminated mostly into the right heart side[10-15,85]. Outflow was mostly into the main PA (47%)[2,61,86], with distribution to the left[80] or right PA branch[87]. Only a few ended in the left heart side[75]. Mild[14,75], moderate[71] to severe[11] pulmonary hypertension was recorded. Dilatation[10,12,14] of the LMT was not frequently observed. In only 3 reports, aneurysmal formation of the LMT was found[13,14,88]. LMT fistulas terminated into PA in 47% and LAD fistulas ended in the PA in 75%[41,65,89-92]. On the other hand, exit to the RA/CS of Cx fistulas was found in 52% and of RCA fistulas was found in 37%. These differences in termination may be related to developmental embryological and anatomical issues. Few LAD fistulas ended in the LV, RV, RA and LA[1,38,93,94]. The clinical presentations of LAD fistulas were usually chest pain[76], angina pectoris[90,95], dyspnea[41,82,92,96-98], fatigue[99], palpitations[1,74], syncope[100], CHF[77,101-103] or IE[1,38]. Cx fistulas terminated into the PA in (23%)[47,104], but the majority ended in the CS in 40%[43,105-109] and the RA in 15%[73,78,110] of cases. The clinical presentations consisted of dyspnea[111,112], palpitations[69,81], syncope[83], angina pectoris[113,114], chest pain[84], fatigue[66,115], CHF[45] and IE[39,40,43]. The termination of RCA fistulas was variable: RA 26%, RV 25%, PA 16%, CS 11%, left LV 12%, LA 3%, SVC 5%, RVOT 1% and PV 1%[33,41,72,70,110,116]. The clinical presentations were angina pectoris[27,35,79], chest pain[9,31,51,117], dyspnea[36,68], palpitations[33] and syncope[118]. In some cases, an abnormal shadow on a chest X-ray brought the subjects to further medical attention[34,119,120]. A comparison between unilateral, bilateral and multilateral fistulas is presented in Table 2. Bilateral fistulas were present in 18% of the total group. The distribution of the origin is summarized in Table 3. The PA pressure was reported frequently to be normal[121-124], but mild[29], moderate[62,125-127] or severe[28] pulmonary hypertension has been reported in this category of fistulas. Fistulas of multilateral origin (i.e. 3 or more fistulas) had a variety of clinical presentations; asymptomatic, chest pain, fatigue, palpitations, dyspnea and syncope[5,6,21,63,128,129]. Termination was mainly into the PA (Table 2).
| Unilateral (n = 243) (80%) | Bilateral (n = 55) (18%) | Multilateral (n = 6) (2%) | |
| Termination | |||
| PA1 | 44% | 73% | 75% |
| CS/RA | 28% | 18% | 10% |
| LA | 2% | 5% | -- |
| LV | 6% | 4% | 15% |
| RV | 13% | 4% | -- |
| Aneurysm | 13% | 16% | 33% |
| Management | |||
| SL | 57% | 51% | 66% |
| CMM | 20% | 32% | 17% |
| PTE | 23% | 17% | 17% |
| Bilateral fistulas | n = 55 |
| LMT-LAD | 3 (5) |
| LMT-RCA | 2 (4) |
| LAD-RSV | 3 (5) |
| LAD-Cx | 1 (2) |
| LCA-RCA | 2 (4) |
| RCA-LAD | 31 (56) |
| RCA-Cx | 8 (15) |
| RSV-Cx | 1 (2) |
| RCA-D | 3 (5) |
| RCA-im | 1 (2) |
Aneurysm: In 43 patients (14%), aneurysmal formation was detected. Aneurysms were associated with unilateral (74%), bilateral (21%) and multilateral fistulas (5%). Overall, exactly the same figure (14%) was found in a mixed pediatric and adult population of 236 patients between 1993 and 2004 reviewed in 2006[64]. Although there were no differences found in the frequency of aneurysm formation, the composition of the 2 studies was completely different. The current review included no pediatric subjects. Aneurysmal formation is infrequently reported in a pediatric population.
Angiographic fistula characteristics related to the mode of termination: A comparison between CCFs and CVFs is shown in Table 4. In CCFs, unilateral fistulas were more prevalent (87%) than in those subjects with CVFs (74%). The fistulas with multiple origins (bilateral and multilateral) were present in 13% and 26% of CCFs and CVFs, respectively. In unilateral CVFs, an origin from the LCA was predominantly involved in fistula formation in 86% of subjects and the RCA in only 14%. In unilateral CCFs, equal distributions of LCA and RCA were found. Comparing the therapeutic strategy between the two reviews of 2010 and 2006[64], we found a specific increase in SL and PTE procedures; from 38% to 56% for SL and from 5% to 22% for PTE, while CMM remained unchanged 21% (2010) vs 24% (2006).
| CCFs (n = 135) (44%) | CVFs (n = 169) (56%) | P value | |
| Mean age (range, yr) | 46.2 (18-85) | 55.6 (18-86) | 0.000 |
| Female gender | 68 (50.4) | 93 (55) | NS |
| Aneurysm | 24 (18.2) | 19 (11.2) | NS |
| MI | None | 5 (3) | 0.042 |
| IE | 11 (8) | None | 0.000 |
| PE | 4 (2.9) | 4 (1.8) | NS |
| Abnormal chest X-ray | 3 (2) | 8 (5) | NS |
| Origin from LMT and LAD | 33 (24.1) | 94 (55.6) | 0.000 |
| Fistulas having multiple origins (bilateral and multilateral) | 17 (13) | 44 (26) | 0.003 |
Up till now, no data has been available describing a large cohort of adults with congenital CAFs. The purpose of this review was to systematically investigate the current characteristics of this anomaly in adults. Generally, CAFs may have 2 angiographic appearances; a solitary form and coronary artery-ventricular multiple micro-fistula form[130]. In the current review further classification of the solitary CAFs according to their mode of termination was undertaken: CCFs and CVFs. On comparison of the current findings with the review of 2006[64], we found that a continuous heart murmur was heard in significantly more patients (82% vs 32%). Furthermore, CHF was reported in more patients (8% vs 3%). The percentage of asymptomatic presentation remained unchanged (11%) compared with the review of 2006 (9%)[64]. In this study, fatigue was present in 6% and palpitations in 13%, while these were both reported as 7% in 2006. IE was not reported in 2006 but was diagnosed in 4% of the patients in this review. CCFs were associated with the development of IE (P = 0.000). None of the patients with CVFs developed IE. Part of the reason for the occurrence of IE in CCFs is that the extent of turbulent flow may be higher in a dilated cardiac chamber compared with a vascular structure and endothelial damage caused by a continuous fistulous jet may be pointed at the wall of the cardiac chamber. In contrast, MI was associated with CVFs (P = 0.042) and it was not seen in any of the patients with CCFs. CVF patients with MI (60.8 years) were 10 years older than the rest of the group (50.7 years). Borderline significance was reached in CCF patients with IE who were 10 years younger (41.8 years) than those who did not develop IE (51.2 years) (P = 0.068). More investigations are warranted to identify subjects who require antibiotics for prophylaxis of IE. Among the subjects in both IE and MI subsets, nearly one-third were female in contrast to the CHF subset where the majority (two-thirds) were female. The lowest mean age was found in the IE subset (41.8 years) and the highest in the CHF subset (60.6 years) (Table 5), implying that subjects with IE are diagnosed earlier and female subjects with congenital CAFs are prone to develop CHF at an older age. Patients with unilateral fistulas and an origin from the RCA, had the lowest mean age (44.9 years) and patients with bilateral and multilateral fistulas were older (57.4 and 58 years, respectively). This may indicate that fistulas from the RCA may become symptomatic earlier and are detected at a relatively young age, while diagnosis may be delayed, for obscure reasons, in fistulas with multiple origins. The behavior of the fistulas in CCFs and CVFs is quite variable, as we found that the frequency of fistulas presenting with multiple origins (bilateral and multilateral) in CVFs (26%) was twice that in CCFs (13%) (P = 0.003), and the termination of bilateral or multilateral fistulas into the PA (29%) was significantly higher than into other outflow sites (10.6%) (P = 0.000). Not only unilateral CAFs may be suspected and diagnosed by echocardiography[2,46,48,67,128] and their presence confirmed by CAG or MDCT[48,131], but also distinctive echocardiographic findings may suggest the presence of bilateral CAFs[48,132]. In the series of Vitarelli et al[2], transthoracic echocardiography was suggestive for the presence of CAFs in 33% of cases and trans-esophageal echocardiography (TOE) confirmed the diagnosis in all patients. In the previously published 2006 review[64], CAG was performed in 83%, while this review found an increase to 97% of subjects. The selective nature of CAG visualizes mainly a single origin of CAFs from a unique coronary artery during its super selective engagement, while MDCT, owing to its non-selective nature is easily able to demonstrate multiple origins of bilateral or multilateral fistulas originating from the coronary arteries or possessing a separate origin directly from the ascending thoracic aorta. Currently, the cornerstone in diagnosis remains echocardiography (68%) and CAG (97%), however MDCT (16%)[48,131], is gaining ground and has proved to be more useful in detecting multilateral fistulas, especially fistulas with multiple origins from the ascending aorta[5,6]. Non-invasive MDCT or TOE should be included alongside CAG in the workup of this category of patient to detect CAFs with suspected or unrecognized multiple origins. The usefulness and advantages of MDCT for the visualization of CAFs are well known. Recognition of CAFs by MDCT has become increasingly popular in adults with congenital CAFs[93].
| Age (yr), mean (range) | Female gender (%) | |
| Origin of fistulas | ||
| Unilateral | ||
| LMT | 50.4 (21-74) | 47 |
| LAD | 55.6 (18-86) | 51 |
| Cx | 51.4 (21-82) | 52 |
| RCA | 44.9 (18-78) | 53 |
| Bilateral | 57.4 (24-83) | 60 |
| Multilateral | 58.0 (38-79) | 67 |
| Clinical presentation | ||
| CHF | 60.6 (27-86) | 70 |
| IE | 41.8 (22-65) | 36 |
| MI | 58.0 (44-78) | 33 |
It was reported in 2006 that the origin of the fistulas was from the LCA in 58% and from the RCA in 42% of patients[64]. In the current review, the overall figures were 69% and 31%, respectively. In 2006, the fistulas were unilateral, bilateral and multilateral in 93%, 6% and 1%, respectively. Currently, the majority, as expected, were unilateral fistulas (80%), followed by bilateral fistulas (18%) and finally multilateral fistulas (2%). Among the unilateral fistulas, the LAD was predominantly the origin (42%) of the fistulas, followed by the RCA (31%), the Cx (20%) and finally the LMT (7%). In this study, it was possible to identify 2 distinct subtypes of clinically relevant fistulas with specific termination sites; the CCFs and the CVFs. In this study, the proportion of fistulas with multiple origins (20%) was significantly increased compared with a few years earlier (7%)[64]. There appears to be distinct differences in terms of mean age, gender and complications between CCFs and CVFs. The difference in mean age between CCF (46.2 years) and CVF (55.6 years) subjects was statistically significant (P = 0.000). The difference in gender was insignificant. No significant difference was found between aneurysmal formation, rupture and PE in CCFs and CVFs. The origin from the LMT and LAD of CCF fistulas was significantly less frequent (24.1%) than of CVFs (55.6%) (P = 0.000) (Table 4).
During the last decade, advances in diagnostic and therapeutic techniques and devices as well as the fruitful collaboration between interventional cardiologists and radiologists[31] have encouraged clinicians to apply sophisticated diagnostic methods and advanced treatment modalities for complex CAFs. Despite the increasing reported numbers of bilateral fistulas, PTE was performed in 22% of subjects. The broad availability of modern occluding materials and devices[133], the rapid gain in experience[134], the collaboration between interventional radiologists and cardiologists[31,134], and the increased number of diagnosed patients as witnessed by the increased proportion of bilateral fistulas, have led to increased rates of SL and PTE procedures (Figure 2). In 2006, SL was performed in 38% of patients, currently reported as increased up to 56%, while PTE was undertaken in only 5%, but is now significantly increased up to 22%, while CMM remains unchanged at 24% vs 21%. The statistical analysis produced significant figures with the application of the univariate method, but this was completely abolished when the multivariate test was performed with correction for age and gender. Age was the confounder and driving force for these differences. Regarding these latter findings and in view of the lack of available data concerning a large cohort of adult patients with congenital CAFs, a national registry and international cooperation should be launched. The conduction of a coordinated and well orchestrated study to build a database according to a prospective well-defined protocol seems to be necessary in the future.
The main findings of this review are summarized as follows: (1) 20% of adults with congenital CAFs are elderly; (2) 63% of patients presented with a single symptom; (3) severe complications such as IE and MI are relatively uncommon and occurred more commonly in males (IE 64% and MI 67%), but presentation with CHF occurred more frequently in females (70%) and had a higher (60.6 years) mean age; (4) CCFs may predispose to the development of IE, which was exclusively reported in patients with CCFs either having a unilateral or a bilateral origin; (5) regardless of the origin from the left or right coronary arteries, either in a unilateral or bilateral fashion, MI was infrequently recorded but selectively occurred in patients with CVFs (P = 0.042); (6) echocardiography and CAG remain the mainstay to suspect and detect CAFs in symptomatic and asymptomatic adult subjects; MDCT is rapidly gaining ground in the diagnostic armamentarium; (7) currently, LCA is the origin of unilateral fistulas in two-thirds of subjects; subjects with unilateral fistulas originating from the RCA are relatively younger age (44.9 years) and may be diagnosed earlier compared with the LCA (54.4 years) and multilateral fistulas (58 years); moreover, fistulas with multiple origins are more readily reported (20%); and (8) in the last decade, SL (56%) and PTE (22%) have tremendously increased as a treatment option of congenital CAFs in adults.
There are some recognized limitations of this review. One is that many publications of the last decade were not included in this work due to incompleteness and lack of specific data needed for the current review. Therefore there may be a problem of limited sample size. The important question of whether there is a need for IE antibiotic prophylaxis in all subtypes of CAFs, or should it be reserved for CCFs is difficult to answer from the present data. Further investigations are warranted. A further shortcoming is the fact that the numbers in the subgroups are small. The need for a prospective national and international registry is of pivotal importance.
The authors appreciate the great assistance of the librarians Mrs. Geerdink A and Mr. Maas D of hospital Group Twente. Mr. Nijhuis RLG, MD, PhD and Mrs. Luiken-McLaren C are greatly appreciated for their intellectual support during the preparation of the manuscript.
Coronary artery fistulas (CAFs) are a rare congenital anomaly of termination of the coronary arterial tree. The incidence of CAFs is low but is currently increasingly detected with the broad application of echocardiography, conventional coronary angiography (CAG), and the use of sophisticated multi-slice detector computed tomography (MDCT).
These anomalies may be associated with longevity extending into the septuagenarian and octogenarian stage of life. For detection of CAFs, invasive and non-invasive modalities are readily available. The anatomical delineation of the course of the fistula and assessment of functional properties are of pivotal significance in the determination of the therapeutic strategy. In the current review, data is presented of adult patients with congenital CAFs. The correct diagnosis necessitates a multi-diagnostic approach. Initiation of a prospective national/international database to collect all relevant data is of distinctive value to properly evaluate this rare congenital anomaly.
Recent reports have highlighted and emphasized the importance of appropriate delineation of the angiographic and anatomic course of the fistulous pathway in patients with congenital CAFs.
Despite the wide availability of MDCT, echocardiography and conventional CAG with its limited 2-dimensional character is still a very important diagnostic tool in establishing the diagnoses of CAFs. In some patients, MDCT may be a complementary or supplemental non-invasive diagnostic modality to echocardiography and conventional CAG. With further sophistication and its 3-dimensional properties it may, in the future, even replace conventional CAG in the detection of congenital CAFs.
CAFs: CAFs are considered when an abnormal communication exists between one or more coronary arteries and a cardiac chamber or an intrathoracic vascular structure. According to their mode of termination, CAFs may be classified into coronary-cameral or coronary-vascular fistulas.
This article is a very comprehensive review about the characteristics of congenital coronary artery fistulas in adults. However, it should be noted that coronary artery fistula is not infrequently observed, and most of them are not published. Therefore, unusual and complicated cases were more frequently reported than it really was. So, the review of published literature may result in the selection bias and this should be pointed out in the study limitation. Otherwise, this paper is well organized and well written about this issue.
Peer reviewers: Seung-Woon Rha, MD, PhD, FACC, FAHA, FESC, FSCAI, FAPSIC, Cardiovascular Center, Korea University Guro Hospital, 80, Guro-dong, Guro-gu, Seoul 152-703, South Korea; Pil-Ki Min, MD, PhD, Cardiology Division, Heart Center, Gangnam Severance Hospital, Yonsei University College of Medicine, 712 Eonjuro, Gangnam-gu, Seoul 135-720, South Korea
S- Editor Cheng JX L- Editor Cant MR E- Editor Zheng XM
| 1. | Hong GJ, Lin CY, Lee CY, Loh SH, Yang HS, Liu KY, Tsai YT, Tsai CS. Congenital coronary artery fistulas: clinical considerations and surgical treatment. ANZ J Surg. 2004;74:350-355. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 30] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Vitarelli A, De Curtis G, Conde Y, Colantonio M, Di Benedetto G, Pecce P, De Nardo L, Squillaci E. Assessment of congenital coronary artery fistulas by transesophageal color Doppler echocardiography. Am J Med. 2002;113:127-133. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 76] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Parga JR, Ikari NM, Bustamante LN, Rochitte CE, de Avila LF, Oliveira SA. Case report: MRI evaluation of congenital coronary artery fistulae. Br J Radiol. 2004;77:508-511. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Duerinckx AJ, Shaaban A, Lewis A, Perloff J, Laks H. 3D MR imaging of coronary arteriovenous fistulas. Eur Radiol. 2000;10:1459-1463. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Dimitrakakis G, Von Oppell U, Luckraz H, Groves P. Surgical repair of triple coronary-pulmonary artery fistulae with associated atrial septal defect and aortic valve regurgitation. Interact Cardiovasc Thorac Surg. 2008;7:933-934. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Hatakeyama Y, Doi T, Shirasawa K, Sasaki Y, Inenaga K, Takeda S, Takeoka R, Hwang MW, Nomura Y, Park CH. Four coronary to pulmonary artery fistulas originating from the left main trunk and each of three coronary arteries (LAD, LCX and RCA) detected by the combination of coronary angiography and multislice computed tomography. Int J Cardiol. 2007;121:227-228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Oncel D, Oncel G. Right coronary artery to left ventricle fistula--effective diagnosis with 64-MDCT. Int J Cardiovasc Imaging. 2007;23:287-291. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Kimura M, Shiraishi J, Ito D, Ariyoshi M, Matsui A, Arihara M, Irie H, Hyogo M, Shima T, Kohno Y. Usefulness and Limitation of Transthoracic Echocardiography in the Diagnosis of Large Coronary Artery Fistula. Echocardiography. 2010;Epub ahead of print. [PubMed] [Cited in This Article: ] |
| 9. | Serçelik A, Mavi A, Ayalp R, Pestamalci T, Gümüsburun E, Batiraliev T. Congenital coronary artery fistulas in Turkish patients undergoing diagnostic cardiac angiography. Int J Clin Pract. 2003;57:280-283. [PubMed] [Cited in This Article: ] |
| 10. | Sáez de Ibarra JI, Fernández-Tarrío R, Francisco Forteza J, Bonnín O. Giant coronary artery fistula between the left main coronary artery and the superior vena cava complicated by coronary artery dissection. Rev Esp Cardiol. 2010;63:743-744. [PubMed] [Cited in This Article: ] |
| 11. | Dahiya R, Copeland J, Butman SM. Myocardial ischemia and congestive heart failure from a left main to coronary sinus fistula. Cardiol Rev. 2004;12:59-62. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Egea-Serrano P, Fernández RG, Menchero AG, Jaldón MS. Coronary artery fistula documented by invasive and non-invasive image techniques. Eur Heart J. 2009;30:939. [PubMed] [Cited in This Article: ] |
| 13. | Vijayvergiya R, Singh TP, Grover A. Large left coronary artery to coronary sinus fistula. Int J Cardiol. 2006;108:132-134. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Rangasetty UC, Ahmad M. Giant coronary artery fistula with aneurysm and multiple openings: a two-dimensional echocardiographic evaluation. Echocardiography. 2006;23:611-613. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Gamma R, Seiler J, Moschovitis G, Mohacsi P, Berdat P, Zenklusen RZ, Tüller D, Walpoth N. Giant coronary artery fistula complicated by cardiac tamponade. Int J Cardiol. 2006;107:413-414. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Tomasian A, Lell M, Currier J, Rahman J, Krishnam MS. Coronary artery to pulmonary artery fistulae with multiple aneurysms: radiological features on dual-source 64-slice CT angiography. Br J Radiol. 2008;81:e218-e220. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | De Santis A, Cifarelli A, Violini R. Transcatheter closure of coronary artery fistula using the new Amplatzer vascular plug and a telescoping catheter technique. J Cardiovasc Med (Hagerstown). 2010;11:605-609. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Vaidyanathan KR, Theodore SA, Sankar MN, Cherian KM. Coronary artery to pulmonary artery fistula with dual origin--embryological, clinical and surgical significance. Eur J Cardiothorac Surg. 2007;31:318-319. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Noda Y, Matsutera R, Yasuoka Y, Abe H, Adachi H, Hattori S, Araki R, Imanaka T, Kosugi M, Sasaki T. Noninvasive demonstration of dual coronary artery fistulas to main pulmonary artery with 64-slice multidetector-computed tomography: a case report. Cardiol Res Pract. 2010;. [PubMed] [Cited in This Article: ] |
| 20. | Sangiorgi G, Castelvecchio S, Inglese L. Successful double percutaneous alcohol and coil embolization of bilateral coronary-to-pulmonary artery fistulas. J Interven Cardiol. 2000;13:209-213 doi: 10.1111/j.1540-8183.2000.tb00292.x. [Cited in This Article: ] |
| 21. | Vermeulen T, Haine S, Paelinck BP, Rodrigus IE, Vrints CJ, Conraads VM. Coronary artery-pulmonary artery fistula in a heart-transplanted patient. Eur J Echocardiogr. 2010;11:80-81. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Hol PK, Geiran O, Andersen K, Vatne K, Offstad J, Svennevig JL, Fosse E. Improvement of coronary artery fistula surgery by intraoperative imaging. Ann Thorac Surg. 2004;78:2193-2195. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Cebi N, Schulze-Waltrup N, Frömke J, Scheffold T, Heuer H. Congenital coronary artery fistulas in adults: concomitant pathologies and treatment. Int J Cardiovasc Imaging. 2008;24:349-355. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Hendry C, Mahadevan V, Fath-Ordoubadi F. Successful percutaneous closure of coronary artery fistula with angiographic follow-up at 6 months. Catheter Cardiovasc Interv. 2009;73:581-583. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Feuchtner G, Junker D, Bonatti J, Friedrich G. Right coronary artery fistula into left ventricle: dynamic compression shown by multislice computed tomography. Eur J Cardiothorac Surg. 2007;32:933. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Kabbani Z, Garcia-Nielsen L, Lozano ML, Febles T, Febles-Bethencourt L, Castro A. Coil embolization of coronary artery fistulas. A single-centre experience. Cardiovasc Revasc Med. 2008;9:14-17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 27. | Cherif A, Farhati A, Fajraoui M, Boussaada R, Hmam M, Ezzar T, Mourali S, Mechmeche R. [Coronary-pulmonary arterial fistula in the adult: report of 6 cases and review of the literature]. Tunis Med. 2003;81:595-599. [PubMed] [Cited in This Article: ] |
| 28. | Filho JR, Carneiro da Silva OA, Vilarinho DO, Guilherme FG, Ferreira JC, de Souza AM. Pulmonary hypertension secondary to coronary-to-pulmonary artery fistula. Arq Bras Cardiol. 2008;91:e11-e13. [Cited in This Article: ] |
| 29. | Portela A, Vale BP, Bastos R, Sousa JF, Costa I, Paiva J. [Large coronary-pulmonary artery fistulae: percutaneous embolization with microcoils and disposable balloons]. Arq Bras Cardiol. 2005;84:270-272. [PubMed] [Cited in This Article: ] |
| 30. | Dourado LO, Góis AF, Hueb W, César LA. Large bilateral coronary artery fistula: the choice of clinical treatment. Arq Bras Cardiol. 2009;93:e48-e49. [PubMed] [Cited in This Article: ] |
| 31. | Syed MI, Kalweit WH, Shaikh A. Microcoil embolization for treatment of a right coronary arteriovenous fistula. J Interv Cardiol. 2003;16:347-350. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 32. | Abdelmoneim SS, Mookadam F, Moustafa S, Zehr KJ, Mookadam M, Maalouf JF, Holmes DR. Coronary artery fistula: single-center experience spanning 17 years. J Interv Cardiol. 2007;20:265-274. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 33. | Collins N, Mehta R, Benson L, Horlick E. Percutaneous coronary artery fistula closure in adults: technical and procedural aspects. Catheter Cardiovasc Interv. 2007;69:872-880. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 34. | Sawai T, Miyazaki S, Nakahira J, Ito M, Oka M, Tanaka M, Imanaka H, Minami T. Intraoperative transesophageal echocardiography enables characterization of coronary artery fistula in coexistence with multiple giant coronary artery aneurysms. Anesth Analg. 2008;106:1104-1106. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 35. | Arafah MR. Closure of coronary artery fistula using covered stent. J Saudi Heart Ass. 2005;17:185-189. [Cited in This Article: ] |
| 36. | Zoghbi E, Seif F, Obeid M, Abou Nader G, Sawaya J. A young female with an unusual cause of dyspnea. Int J Cardiol. 2007;122:e21-e22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 37. | Gupta M. Coronary artery fistula. Available from: http://emedicine.medscape.com/article/895749-overview. [Cited in This Article: ] |
| 38. | Agostini M, Ribichini F, Portolan M, Ugliengo G, Iacovoni A, Grossi C. Giant coronary artery fistula connecting the left coronary sinus with the superior atriocaval junction. Ital Heart J. 2004;5:483-485. [PubMed] [Cited in This Article: ] |
| 39. | Hajj-Chahine J, Haddad F, El-Rassi I, Jebara V. Surgical management of a circumflex aneurysm with fistula to the coronary sinus. Eur J Cardiothorac Surg. 2009;35:1086-1088. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 40. | Kasravi B, Reid CL, Allen BJ. Coronary artery fistula presenting as bacterial endocarditis. J Am Soc Echocardiogr. 2004;17:1315-1316. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 41. | Demirkilic U, Ozal E, Bingol H, Cingoz F, Gunay C, Doganci S, Kuralay E, Tatar H. Surgical treatment of coronary artery fistulas: 15 years' experience. Asian Cardiovasc Thorac Ann. 2004;12:133-138. [PubMed] [Cited in This Article: ] |
| 42. | Gill DS, Yong QW, Wong TW, Tan LK, Ng KS. Vegetation and bilateral congenital coronary artery fistulas. J Am Soc Echocardiogr. 2005;18:492-493. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 43. | Chamberlain MH, Henry R, Brann S, Angelini GD. Surgical management of a gigantic circumflex coronary artery aneurysm with fistulous connection to the coronary sinus. Eur J Cardiothorac Surg. 2001;20:1255-1257. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 44. | Umezu K, Hanayama N, Toyama A, Hobo K, Takazawa A. Successful repair for a giant coronary artery aneurysm with coronary arteriovenous fistula complicated by both right- and left-sided infective endocarditis. Gen Thorac Cardiovasc Surg. 2009;57:544-546. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 45. | Aoyagi S, Fukunaga S, Ishihara K, Egawa N, Hosokawa Y, Nakamura E. Coronary artery fistula from the left circumflex to the coronary sinus. Int Heart J. 2006;47:147-152. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 46. | Tirilomis T, Aleksic I, Busch T, Zenker D, Ruschewski W, Dalichau H. Congenital coronary artery fistulas in adults: surgical treatment and outcome. Int J Cardiol. 2005;98:57-59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 54] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 47. | Onorati F, Mastroroberto P, Bilotta M, Cristodoro L, Esposito A, Pezzo F, Renzulli A. Surgical treatment of coronary-to-pulmonary fistula: how and when? Heart Vessels. 2006;21:321-324. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 48. | Chan MS, Chan IY, Fung KH, Lee G, Tsui KL, Leung TC. Demonstration of complex coronary-pulmonary artery fistula by MDCT and correlation with coronary angiography. AJR Am J Roentgenol. 2005;184:S28-S32. [PubMed] [Cited in This Article: ] |
| 49. | Müller D, Wimmer-Greinecker G, Fichtelscherer S, Moritz A. Symptomatic coronary artery-Pulmonary artery fistulae. Int J Thorac Cardiovasc Surg. 2004;20:192-193 doi: 10.1007/s12055-004-0085-9. [Cited in This Article: ] |
| 50. | Ashmeik K, Amin J, Pai RG. Echocardiographic characterization of a rare type of coronary artery fistula draining into superior vena cava. J Am Soc Echocardiogr. 2000;13:407-411. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 51. | Abdelmoneim SS, Mookadam F, Moustafa SE, Holmes DR. Coronary artery fistula with anomalous coronary artery origin: a case report. J Am Soc Echocardiogr. 2007;20:333.e1-333.e4. [PubMed] [Cited in This Article: ] |
| 52. | Doganay S, Bozkurt M, Kantarci M, Erkut B. Coronary artery-pulmonary vein fistula diagnosed by multidetector computed tomography. J Cardiovasc Med (Hagerstown). 2009;10:428-430. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 53. | Ozaki N, Wakita N, Inoue K, Yamada A. Surgical repair of coronary artery to pulmonary artery fistula with aneurysms. Eur J Cardiothorac Surg. 2009;35:1089-1090. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 54. | Nakamura K, Shiratori K, Hashimoto K. Giant saccular aneurysm of coronary arteriovenous fistula to the main pulmonary artery: intraoperative assessment by using fluorescent imaging. Ann Thorac Cardiovasc Surg. 2010;16:354-357. [PubMed] [Cited in This Article: ] |
| 55. | Ito M, Kodama M, Saeki M, Fukunaga H, Goto T, Inoue H, Kasuya S, Aizawa Y. Rupture of a giant saccular aneurysm of coronary arteriovenous fistulas. Jpn Heart J. 2000;41:659-664. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 56. | Izumi K, Hisata Y, Hazam S. Surgical repair for a coronary-pulmonary artery fistula with a saccular aneurysm of the coronary artery. Ann Thorac Cardiovasc Surg. 2009;15:194-197. [PubMed] [Cited in This Article: ] |
| 57. | Nagaya K, Nagamine S, Osaka K, Kakihata H. A case of coronary-pulmonary artery fistula with a giant aneurysm. Jpn J Cardiovasc Surg. 2006;35:81-84. [Cited in This Article: ] |
| 58. | Fujimoto N, Onishi K, Tanabe M, Koji T, Omichi C, Kato S, Kawasaki A, Nakano T, Ito M. Two cases of giant aneurysm in coronary-pulmonary artery fistula associated with atherosclerotic change. Int J Cardiol. 2004;97:577-578. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 59. | Bouchez S, Coddens J, Vanermen H, Mustafa G, Shernan S. Case 3--2001: multiplane transesophageal echocardiography in minimally invasive surgery for coronary artery fistula. J Cardiothorac Vasc Anesth. 2001;15:114-117. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 60. | Kinoshita O, Ogiwara F, Hanaoka T, Tomita T, Yokozeki O, Kai R, Uchikawa S, Kogashi K, Tsutsui H, Imamura H. Large saccular aneurysm in a coronary arterial fistula--a case report. Angiology. 2005;56:233-235. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 61. | Okwuosa TM, Gundeck EL, Ward RP. Coronary to pulmonary artery fistula--diagnosis by transesophageal echocardiography. Echocardiography. 2006;23:62-64. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 62. | Brown MA, Balzer D, Lasala J. Multiple coronary artery fistulae treated with a single Amplatzer vascular plug: check the back door when the front is locked. Catheter Cardiovasc Interv. 2009;73:390-394. [PubMed] [Cited in This Article: ] |
| 63. | Sugihara M, Yamamoto H, Matsushita H, Tadehara F, Gomyo Y, Mochizuki T, Marui A. Multiple coronary artery fistulas with a huge right coronary artery showing exacerbation during 16 years of follow-up. Circ J. 2004;68:85-87. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 64. | Said SA, Lam J, van der Werf T. Solitary coronary artery fistulas: a congenital anomaly in children and adults. A contemporary review. Congenit Heart Dis. 2006;1:63-76. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 65. | Gandy KL, Rebeiz AG, Wang A, Jaggers JJ. Left main coronary artery-to-pulmonary artery fistula with severe aneurysmal dilatation. Ann Thorac Surg. 2004;77:1081-1083. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 66. | Darwazah AK, Hussein IH, Hawari MH. Congenital circumflex coronary arteriovenous fistula with aneurysmal termination in the pulmonary artery. Tex Heart Inst J. 2005;32:56-59; discussion 58-59. [PubMed] [Cited in This Article: ] |
| 67. | Chee TS, Tan PJ, Koh SK, Jayaram L. Coronary artery fistula diagnosed by transthoracic Doppler echocardiography. Singapore Med J. 2007;48:e262-e264. [PubMed] [Cited in This Article: ] |
| 68. | Ascoop AK, Budts W. Percutaneous closure of a congenital coronary artery fistula complicated by an acute myocardial infarction. Acta Cardiol. 2004;59:67-69. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 69. | Mohanty SK, Ramanathan KR, Banakal S, Muralidhar K, Kumar P. An interesting case of coronary cameral fistula. Ann Card Anaesth. 2005;8:152-154. [PubMed] [Cited in This Article: ] |
| 70. | Li D, Wu Q, Sun L, Song Y, Wang W, Pan S, Luo G, Liu Y, Qi Z, Tao T. Surgical treatment of giant coronary artery aneurysm. J Thorac Cardiovasc Surg. 2005;130:817-821. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 131] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 71. | Makaryus AN, Kort S, Rosman D, Vatsia S, Mangion JR. Successful surgical repair of a giant left main coronary artery aneurysm with arteriovenous fistula draining into a persistent left superior vena cava and coronary sinus: role of intraoperative transesophageal echocardiography. J Am Soc Echocardiogr. 2003;16:1322-1325. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 72. | El Watidy AM, Ismail HH, Calafiore AM. Surgical management of right coronary artery-coronary sinus fistula causing severe mitral and tricuspid regurgitation. Interact Cardiovasc Thorac Surg. 2010;10:110-112. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 73. | Maleszka A, Kleikamp G, Minami K, Peterschröder A, Körfer R. Giant coronary arteriovenous fistula. A case report and review of the literature. Z Kardiol. 2005;94:38-43. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 74. | Yang Y, Bartel T, Caspari G, Eggebrecht H, Baumgart D, Erbel R. Echocardiographic detection of coronary artery fistula into the pulmonary artery. Eur J Echocardiogr. 2001;2:292-294. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 75. | Tousoulis D, Brilli S, Aggelli K, Tentolouris C, Stefanadis C, Toutouzas K, Frogoudaki A, Toutouzas P. Left main coronary artery to left atrial fistula causing mild pulmonary hypertension. Circulation. 2001;103:2028-2029. [PubMed] [Cited in This Article: ] |
| 76. | Sato F, Koishizawa T. Stress/Rest (99m)Tc-MIBI SPECT and 123I-BMIPP scintigraphy for indication of surgery with coronary artery to pulmonary artery fistula. Int Heart J. 2005;46:355-361. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 77. | Qawoq H, Krecki R, Lipiec P, Krzemińska-Pakuła M, Kasprzak JD. A coronary fistula diagnosed in the eighth decade of life: The utility of non-invasive methods in the selection of treatment approach. Cardiol J. 2010;17:299-302. [PubMed] [Cited in This Article: ] |
| 78. | Okamoto M, Makita Y, Fujii Y, Kajihara K, Yamasaki S, Iwamoto A, Hashimoto M, Sueda T. Successful coil embolization with assistance of coronary stenting in an adult patient with a huge coronary arterial-right atrial fistula. Intern Med. 2006;45:865-870. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 79. | Goswami NJ, Zabalgoitia M. Localization of a coronary artery fistula using contrast transesophageal echocardiography. J Am Soc Echocardiogr. 2002;15:839-840. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 80. | Lu CW, Lin TY, Wang MJ. Large coronary arteriovenous fistula to the main pulmonary artery. Anesth Analg. 2006;103:41-42. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 81. | Sağlam H, Koçoğullari CU, Kaya E, Emmiler M. Congenital coronary artery fistula as a cause of angina pectoris. Turk Kardiyol Dern Ars. 2008;36:552-554. [PubMed] [Cited in This Article: ] |
| 82. | Versaci F, Del Giudice C, Sperandio M, Simonetti G, Chiariello L. A case of coronary artery fistula visualized by 64-slice multidetector CT. Nat Clin Pract Cardiovasc Med. 2009;6:57-60. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 83. | Misumi T, Nishikawa K, Yasudo M, Suzuki T, Kumamaru H. Rupture of an aneurysm of a coronary arteriovenous fistula. Ann Thorac Surg. 2001;71:2026-2027. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 84. | Choh S, Orime Y, Tsukamoto S, Shiono M, Negishi N. Successful surgical treatment of rupture of coronary arteriovenous fistula with unconsciousness after chest and back pain. Ann Thorac Cardiovasc Surg. 2005;11:190-193. [PubMed] [Cited in This Article: ] |
| 85. | Nekkanti R, Nanda NC, Angsingkar KG, Mukhtar O. Transesophageal three-dimensional echocardiographic assessment of left main coronary artery fistula. Echocardiography. 2001;18:305-308. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 86. | Ekonomou CK, Papadopoulos DP, Dalianis NV, Stratigis NG, Benos J, Votteas VE. Coronary fistula from left main stem to main pulmonary artery. J Invasive Cardiol. 2003;15:600-601. [PubMed] [Cited in This Article: ] |
| 87. | Khurana R, Mittal T, Qasim A, Malik I, Qureshi SA, Bogers AJ. Coronary steal with unstable angina secondary to a coronary artery fistula. EuroIntervention. 2009;4:542-548. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 88. | Maeda S, Nishizaki M, Hashiyama N, Mo M, Isobe M. Giant aneurysm in coronary artery fistula. J Am Coll Cardiol. 2009;54:e119. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 89. | Gelsomino S, Rubattu G, Terrosu PF, Cossu L, Orrù F, Barboso G. Successful repair of a coronary artery to pulmonary artery fistula with saccular artery aneurysm and critical stenosis of the left anterior descending coronary artery. Ital Heart J. 2003;4:350-353. [PubMed] [Cited in This Article: ] |
| 90. | Toledo IC, Braile V, Leal JC, Braile DM. [Fistula between anterior intraventricular coronary artery and the pulmonary artery trunk: five operated patients]. Rev Bras Cir Cardiovasc. 2007;22:241-244. [PubMed] [Cited in This Article: ] |
| 91. | Inoue H, Ueno M, Yamamoto H, Matsumoto K, Tao K, Sakata R. Surgical treatment of coronary artery aneurysm with coronary artery fistula. Ann Thorac Cardiovasc Surg. 2009;15:198-202. [PubMed] [Cited in This Article: ] |
| 92. | Kamiya H, Yasuda T, Nagamine H, Sakakibara N, Nishida S, Kawasuji M, Watanabe G. Surgical treatment of congenital coronary artery fistulas: 27 years' experience and a review of the literature. J Card Surg. 2002;17:173-177. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 108] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 93. | Kacmaz F, Ozbulbul NI, Alyan O, Maden O, Demir AD, Balbay Y, Erbay AR, Atak R, Senen K, Olcer T. Imaging of coronary artery anomalies: the role of multidetector computed tomography. Coron Artery Dis. 2008;19:203-209. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 94. | de Doelder MS, Hillers JA. Combination of imaging modalities in a coronary artery fistula. Neth Heart J. 2008;16:313-314. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 95. | Papadopoulos DP, Bourantas CV, Ekonomou CK, Votteas V. Coexistence of atherosclerosis and fistula as a cause of angina pectoris: a case report. Cases J. 2010;3:70. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 96. | Said SA, Schroeder-Tanka JM, Mulder BJ. Female gender and the risk of rupture of congenital aneurysmal fistula in adults. Congenit Heart Dis. 2008;3:63-68. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 97. | Shimamura Y, Yamaki F, Yamamoto H, Kouda T, Tsukagoshi M. Aneurysm in the pulmonary trunk associated with atrial septal defect, a left coronary artery fistula to the pulmonary trunk, and valvular pulmonary stenosis. Jpn J Thorac Cardiovasc Surg. 2000;48:329-333. [PubMed] [Cited in This Article: ] |
| 98. | Klein LW. A new hypothesis of the developmental origin of congenital left anterior descending coronary artery to pulmonary artery fistulas. Catheter Cardiovasc Interv. 2008;71:568-571. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 99. | Zamani J, Tavasoli M, Mahmmoudi Y. Transcatheter coil embolization of coronary artery fistula. Iran Cardiovasc Res J. 2010;4:44-46. [Cited in This Article: ] |
| 100. | Murata N, Yamamoto N. A case of ruptured coronary artery aneurysm associated with coronary artery fistulas. Jpn J Cardiovasc Surg. 2001;30:305-307. [Cited in This Article: ] |
| 101. | Rhee GH, Choi JK, Kuh JH, Rhee YK, Chae JK, Kim WH, Ko JK. Congenital coronary arteriovenous fistula combined with ASD. Korean Circ J. 2000;30:767-771. [Cited in This Article: ] |
| 102. | Behera SK, Danon S, Levi DS, Moore JW. Transcatheter closure of coronary artery fistulae using the Amplatzer Duct Occluder. Catheter Cardiovasc Interv. 2006;68:242-248. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 49] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 103. | Mullasari AS, Umesan CV, Kumar KJ. Transcatheter closure of coronary artery to pulmonary artery fistula using covered stents. Heart. 2002;87:60. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 104. | Kilic H, Akdemir R, Bicer A, Dogan M. Transcatheter closure of congenital coronary arterial fistulas in adults. Coron Artery Dis. 2008;19:43-45. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 105. | Ahmed J, Edelstein Y, Rose M, Lichstein E, Connolly MW. Coronary arteriovenous fistula with papillary muscle rupture. South Med J. 2000;93:627-628. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 106. | Rajs J, Brodin LA, Hertzfeld I, Larsen FF. Death related to coronary artery fistula after rupture of an aneurysm to the coronary sinus. Am J Forensic Med Pathol. 2001;22:58-61. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 107. | Nakahira A, Sasaki Y, Hirai H, Fukui T, Motoki M, Takahashi Y, Oe H, Kataoka T, Suehiro S. Rupture of aneurysmal circumflex coronary artery into the left atrium after ligation of its arteriovenous fistula. Circ J. 2007;71:1996-1998. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 108. | Dogan A, Ozaydin M, Altinbas A, Gedikli O. A giant aneurysm of the circumflex coronary artery with fistulous connection to the coronary sinus: a case report. Int J Cardiovasc Imaging. 2003;19:5-8. [PubMed] [Cited in This Article: ] |
| 109. | Kearney LG, Chan R, Srivastava PM. Multimodality imaging of circumflex artery fistula to coronary sinus with persistent left-sided superior vena cava. Eur Heart J. 2007;28:2652. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 110. | Komatsu S, Sato Y, Ichikawa M, Kunimasa T, Ito S, Takagi T, Lee T, Matsumoto N, Takayama T, Ichikawa M. Anomalous coronary arteries in adults detected by multislice computed tomography: presentation of cases from multicenter registry and review of the literature. Heart Vessels. 2008;23:26-34. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 111. | Burns KE, Ferguson KA, Spouge A, Brown JE. Massive congenital coronary arteriovenous malformation presenting with exertional dyspnea and desaturation in an adult: a case report and review of the literature. Can J Cardiol. 2001;17:85-89. [PubMed] [Cited in This Article: ] |
| 112. | Gufler H, Voigtlander T, Nowak B, Magedanz A, Schmermund A. Left circumflex coronary artery fistula to the superior vena cava: assessment of the exact anatomy by multidetector CT. Clin Res Cardiol. 2008;97:272-276. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 113. | Díaz de la Llera LS, Fournier Andray JA, Gómez Moreno S, Mayol Deya A, González García A, Pérez Fernández-Cortacero JA. [Percutaneous occlusion with coils of coronary artery fistulas in adults]. Rev Esp Cardiol. 2005;58:93-96. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 114. | Pate GE, Webb JG, Carere RG. An unusual complication of coil embolization of a large coronary-pulmonary fistula. J Invasive Cardiol. 2003;15:717-718. [PubMed] [Cited in This Article: ] |
| 115. | Said SA, van der Sluis A, Koster K, Sie H, Shahin GM. Congenital circumflex artery-coronary sinus fistula in an adult female associated with severe mitral regurgitation and myelodysplasy--case report and review of the literature. Congenit Heart Dis. 2010;5:599-606. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 116. | Zhu XY, Zhang DZ, Han XM, Cui CS, Sheng XT, Wang QG, Cha YM, Abhiram P, Rihal CS. Transcatheter closure of congenital coronary artery fistulae: immediate and long-term follow-up results. Clin Cardiol. 2009;32:506-512. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 117. | Weymann A, Lembcke A, Konertz WF. Right coronary artery to superior vena cava fistula: imaging with cardiac catheterization, 320-detector row computed tomography, magnetic resonance imaging, and transoesophageal echocardiography. Eur Heart J. 2009;30:2146. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 118. | Meerkin D, Balkin J, Klutstein M. Rapid transcatheter occlusion of a coronary cameral fistula using a three-lobed vascular occlusion plug. J Invasive Cardiol. 2009;21:E151-E153. [PubMed] [Cited in This Article: ] |
| 119. | Chen YF, Chien TM, Lee CS. Coronary aneurysm with double right coronary artery and fistula. J Thorac Cardiovasc Surg. 2011;141:585. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 120. | Mawatari T, Koshino T, Morishita K, Komatsu K, Abe T. Successful surgical treatment of giant coronary artery aneurysm with fistula. Ann Thorac Surg. 2000;70:1394-1397. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 41] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 121. | Phillips MB, Oken KR. Embryology in the elderly: Bilateral coronary artery fistulae. Southern Med J. 2005;98:S45 doi: 10.1097/00007611-200510001-00121. [Cited in This Article: ] |
| 122. | Androulakis A, Chrysohoou C, Barbetseas J, Brili S, Kakavas A, Maragiannis D, Kallikazaros I, Stefanadis C. Arteriovenous connection between the aorta and the coronary sinus through a giant fistulous right coronary artery. Hellenic J Cardiol. 2008;49:48-51. [PubMed] [Cited in This Article: ] |
| 123. | Huang HC, Liu CY, Lu TM, Hsu CP. Applying preoperative multidetector computed tomography to bilateral coronary artery fistulas. J Chin Med Assoc. 2010;73:431-434. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 124. | Osawa H, Sakurada T, Sasaki J, Araki E. Successful surgical repair of a bilateral coronary-to-pulmonary artery fistula. Ann Thorac Cardiovasc Surg. 2009;15:50-52. [PubMed] [Cited in This Article: ] |
| 125. | Zhou T, Shen XQ, Fang ZF, Zhou SH, Qi SS, Lü XL. Transcatheter closure of a giant coronary artery fistula with patent duct occluder. Chin Med J (Engl). 2006;119:779-781. [PubMed] [Cited in This Article: ] |
| 126. | Sun S, Li JY, Hu PY, Wu SJ. Starfish-assisted off-pump obliteration of massive coronary arteriovenous fistulae. Tex Heart Inst J. 2005;32:595-597. [PubMed] [Cited in This Article: ] |
| 127. | Wu YJ, Chan YC, Hung CL, Hou CJY. Congestive heart failure in a patient with giant aneurysm-like right coronary AV fistula. Acta Cardiol Sin. 2004;20:105-109. [Cited in This Article: ] |
| 128. | Li RG, Fang WY, Shi HY, Qu XK, Chen H, Qiu XB, Xu YJ, Dong JL, Guan SF, Jiang B. Transcatheter coil embolization of multiple coronary artery-to-left ventricle fistulas: report of a rare case. Chin Med J (Engl). 2008;121:1342-1344. [PubMed] [Cited in This Article: ] |
| 129. | Fujii H, Tsutsumi Y, Ohashi H, Kawai T, Iino K, Onaka M. Surgical treatment of multiple coronary artery fistulas with an associated small saccular aneurysm--a case report. J Card Surg. 2006;21:493-495. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 130. | Said SA. Congenital solitary coronary artery fistulas characterized by their drainage sites. World J Cardiol. 2010;2:6-12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 131. | Tan KT, Chamberlain-Webber R, McGann G. Characterisation of coronary artery fistula by multi-slice computed tomography. Int J Cardiol. 2006;111:311-312. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 132. | Gach O, Davin L, Legrand V. Non-invasive imaging of a giant right coronary artery due to a coronary fistula. Acta Cardiol. 2006;61:569-571. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 133. | Sim JY, Alejos JC, Moore JW. Techniques and applications of transcatheter embolization procedures in pediatric cardiology. J Interv Cardiol. 2003;16:425-448. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 134. | Said SAM, Nijhuis RLG, op den Akker JW, Kimman GP, Van Houwelingen KG, Gerrits D, Huisman AB, Slart RHJA, Nicastia DM, Koomen EM. Diagnostic and therapeutic approach of congenital solitary coronary artery fistulas in adults: Dutch case series and review of literature. Neth Heart J. 2011;19:183-191 doi: 10.1007/s12471-011-0088-2. [Cited in This Article: ] |