Published online Aug 18, 2012. doi: 10.5312/wjo.v3.i8.131
Revised: December 15, 2011
Accepted: August 7, 2012
Published online: August 18, 2012
AIM: To determine hip joint center (HJC) location on hip arthroplasty population comparing predictive and functional approaches with radiographic measurements.
METHODS: The distance between the HJC and the mid-pelvis was calculated and compared between the three approaches. The localisation error between the predictive and functional approach was compared using the radiographic measurements as the reference. The operated leg was compared to the non-operated leg.
RESULTS: A significant difference was found for the distance between the HJC and the mid-pelvis when comparing the predictive and functional method. The functional method leads to fewer errors. A statistical difference was found for the localization error between the predictive and functional method. The functional method is twice more precise.
CONCLUSION: Although being more individualized, the functional method improves HJC localization and should be used in three-dimensional gait analysis.
- Citation: Bouffard V, Begon M, Champagne A, Farhadnia P, Vendittoli PA, Lavigne M, Prince F. Hip joint center localisation: A biomechanical application to hip arthroplasty population. World J Orthop 2012; 3(8): 131-136
- URL: https://www.wjgnet.com/2218-5836/full/v3/i8/131.htm
- DOI: https://dx.doi.org/10.5312/wjo.v3.i8.131
Hip arthroplasty is a well accepted and successful procedure for patients suffering from degenerative hip joint disease. However, the anatomical reconstruction of the hip is not always easy[1-3] and the insertion of a hip prosthesis may lead to modification of hip geometry[4-6]. Consequently, these changes affect the hip joint dynamics. In gait analysis, accurate location of the hip joint center (HJC) is crucial for the quantification of the musculoskeletal loading at the hip joint and is one of the key point for the study of post-operative rehabilitation[7]. This aspect is even more important in pathologic subjects, where the hip geometry and symmetry have been modified by the surgery and the pathological process. Improper HJC location can affect hip loading, angles, moments and powers calculation acting at the hip joint[4-6].
The determination of joint center location of the lower limb is easier at the ankle and the knee than at the hip joint. For the ankle, the midpoint between the two malleolii gives a good estimate of the joint center of this articulation[8] while knee alignment devices improve significantly the estimation of the knee flexion-axis and the location of the knee joint center[9]. Since the HJC location is further to the skin surface and bony landmarks, no such assumptions can be made to locate the HJC.
Several studies on hip arthroplasty[10-15] have relied on three-dimensional (3D) motion analysis programs (Cortex Motion analysis), Nondestructive Inspection first principle (Optotrak), Workstation (Vicon) to calculate HJC after hip arthroplasty. Since these softwares locate the HJC using predictive methods, a bias can be introduced by HJC mislocation and hence, could affect the calculation of hip joint dynamics. Predictive approaches for locating HJC provide only an estimation of the HJC based on linear regression equations of data coming from markers placed on bony landmarks. For example, some models use the leg length, the width and depth of the pelvis to locate the HJC. All models used in the predictive approach have been determined on few healthy subjects of homogeneous populations. Moreover, hip symmetry of the two legs is often assumed[16]. The accuracy of HJC calculated by this approach differs between studies. According to Bell et al[17] differences of 16 to 65 mm were observed between HJC calculated by the predictive method compared to radiographic measurements while Leardini et al[18] found difference of 8 to 16 mm with a similar study. It seems that the predictive method can be used for able-bodied subject but HJC location estimation can be compromised when applied to hip arthroplasty population, for which symmetry of both legs and pelvis are modified.
In recent years, the functional method, which uses the thigh kinematics relative to the pelvis, in its three degree of freedom, to estimate 3D HJC location, has been proposed[7,18-21] to improve precision of HJC location. Several algorithms exist to model the HJC based on the functional method, and according to Erigh et al[7] the Score algorithm provides the smallest estimation error on the HJC location.
To our knowledge, no study has evaluated the impact of the HJC estimation method on a pathologic population. Moreover, no study has assessed the difference in algorithm performance between the operated and non-operated legs. The purpose of this study is twofold: (1) to compare the precision of 3D location of the HJC obtained by both predictive and functional methods in patients with hip arthroplasty and to compare them with radiographic measurements; and (2) to determine if a difference in HJC location exists between the operated and non-operated leg using the Score algorithm. Our hypotheses are that the functional method will be more accurate to estimate the HJC than the predictive method in hip arthroplasty patients and that the Score algorithm will perform as well as the operated leg than the non-operated leg.
Patients from the orthopaedic clinic of Maisonneuve-Rosemont Hospital presenting unilateral hip osteoarthritis and no other functional problems of the lower limb were invited to participate in this study. Fourteen patients (age: 58.9 ± 9.3 years, weight: 81.0 ± 15.4 kg, height: 1.69 ± 0.09 m, body mass index: 28.2 ± 3.4 kg/m2) gave their written consent in accordance to the institutional research ethics and scientific committees.
All hip replacements were performed by three experienced surgeons (ML, PAV, AR) using the posterior approach[22]. The biomechanics of the operated hip was restored based on pre-operative template of the normal contra lateral side.
Standardized post-operative anteroposterior radiographs of the pelvis were taken. To ensure a normalized positioning of the pelvis in both frontal and sagittal planes, the legs were positioned at 15° of internal rotation and the coccyx was centered on the pubic symphysis and located proximally to within 20 to 40 mm of the pubis. After being scanned (VIDAR VXR-12, Virginia, USA) radiographs were calibrated and analysed using Imagika software (Clinical Measurement Corporation, New Jersey, USA).
The HJC location was defined as the geometrical center of the femoral head modeled as a sphere. In the frontal plane, the perpendicular distance from the mid-pelvis line (line from the center of sacrum to center of pubic symphysis) and HJC was measured for both legs (Figure 1).
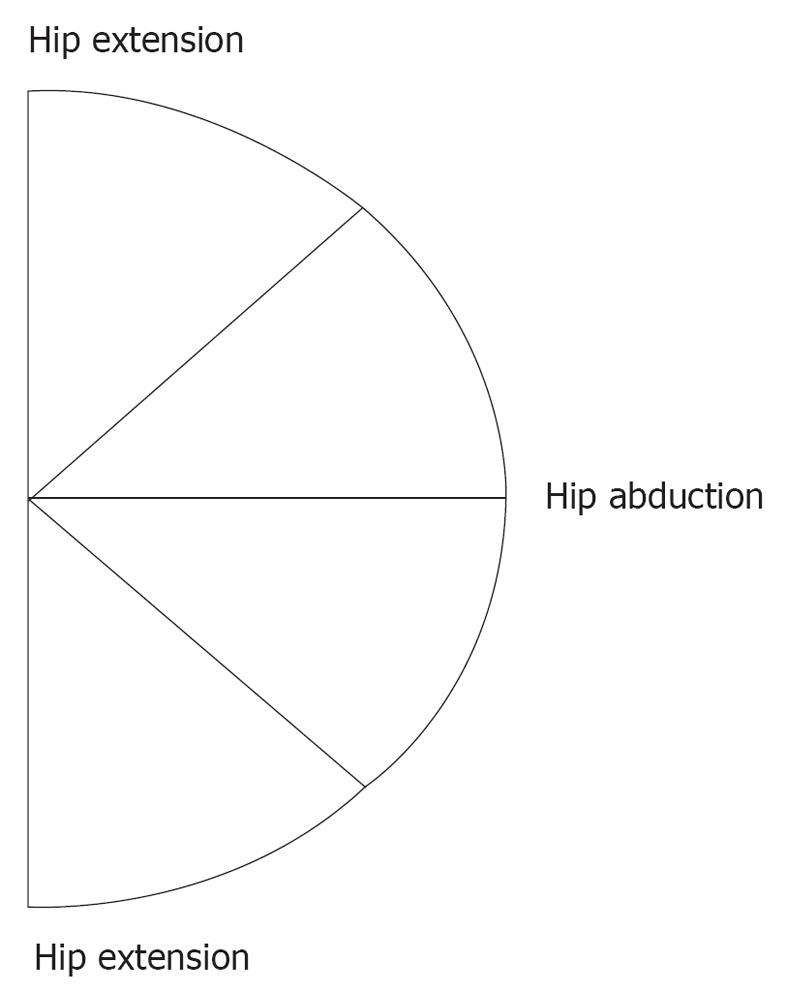
Reflective markers were placed on the left and right antero and postero-superior iliac spines, lateral mid-thigh, medial and lateral knee condyles. Kinematics was recorded at 60 Hz by an 8 cameras Vicon system (Oxford Metrics, Oxford, UK). First, a 5 s static trial, was acquired where the subject received the same instruction as for the radiograph. They were then asked to maintain their trunk in an upright position and to perform three repetitions of the Star Arc movement for both legs. The Star Arc movement, as described in Camomilla et al[23], consists in six movements: starting with a hip flexion, following by three hip abduction a hip extension and finishing by a hip circumduction (Figure 2). All these movements were performed without pain at subject’s selected velocity and amplitude.
A local system of coordinates (SoC) was defined for the pelvis to correspond to the radiographic plane. The pelvic plane of reference was thus defined in the frontal plane as determined by the vertical axis and the antero-superior iliac spines. The vertical axis was chosen as the vector of reference. The SoC of the thigh was calculated using the three markers placed on the mid thigh, medial and lateral knee condyles. The functional HJC was located, for both the operated and non-operated leg using the Score algorithm[7]. Both the functional and predictive methods (calculated by Workstation software, Oxford Metrics, Oxford, UK) of HJC locations were imported in the pelvis SoC in the static trial (Figure 3).
The absolute medio-lateral coordinates of both, the predictive and functional methods were used to calculate the distance between the HJC and the mid-pelvis (HJCD) and were compared to the radiographic measurements[17,18,24]. The HJCD of the operated and non-operated legs were also compared. Furthermore, the HJC location error (HJCLE) was determined (radiographic measurement - predictive and functional method) and was compared between the two methods. The HJCLE of the operated and non-operated legs were also compared. Data were processed with Matlab 7.0 (The MathWorks Inc., MA, USA).
Statistical analyses were performed using SPSS 17.0 (SPSS Inc., Illinois, USA). A two-way analysis of variance (ANOVA) was used to compare the HJCD obtained by the three methods (predictive, functional and radiographics measurements) and to compare the results obtained for the operated and non-operated legs. The HJCLE was analyzed using a two-way ANOVA. The results were then further analysed, if necessary, with Tukey post-hoc tests. All analyses were done with a level of signification set at 0.05.
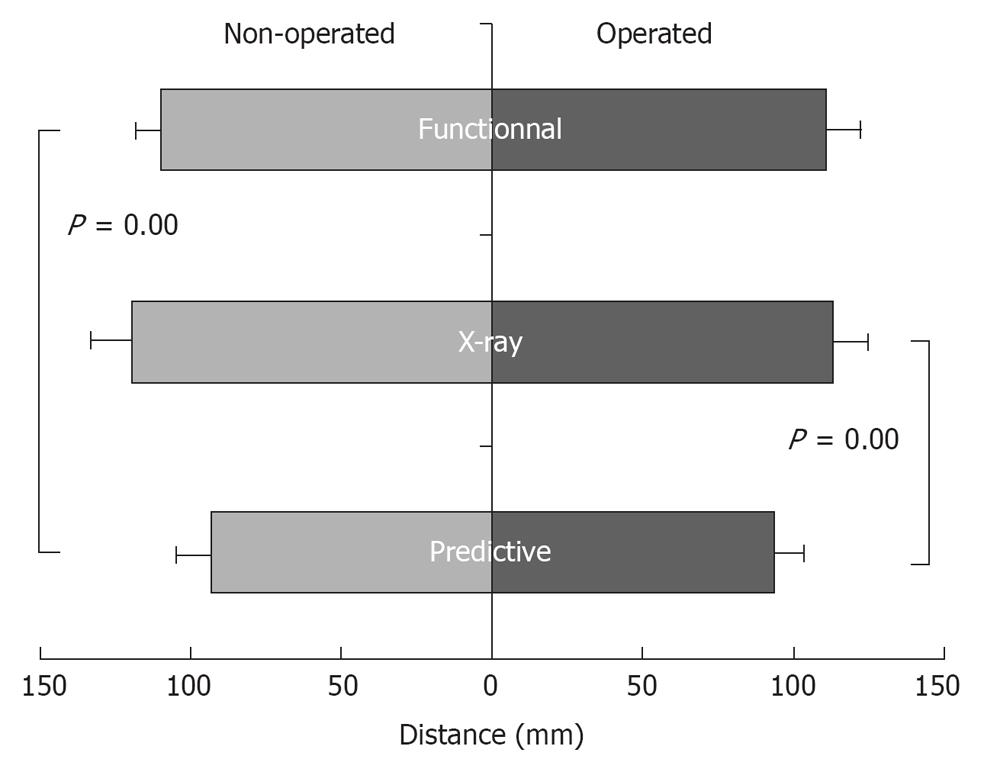
A significant difference was found between the HJCD and the predictive method compared to the functional method (P = 0.01) and the radiographic measurements (P = 0.01). No significant difference was found for the HJCD between the functional method compared to radiographic measurements (P = 0.06). No statistical difference was found for the legs (operated vs non-operated) and no interaction was found (method × leg) (Figure 4).
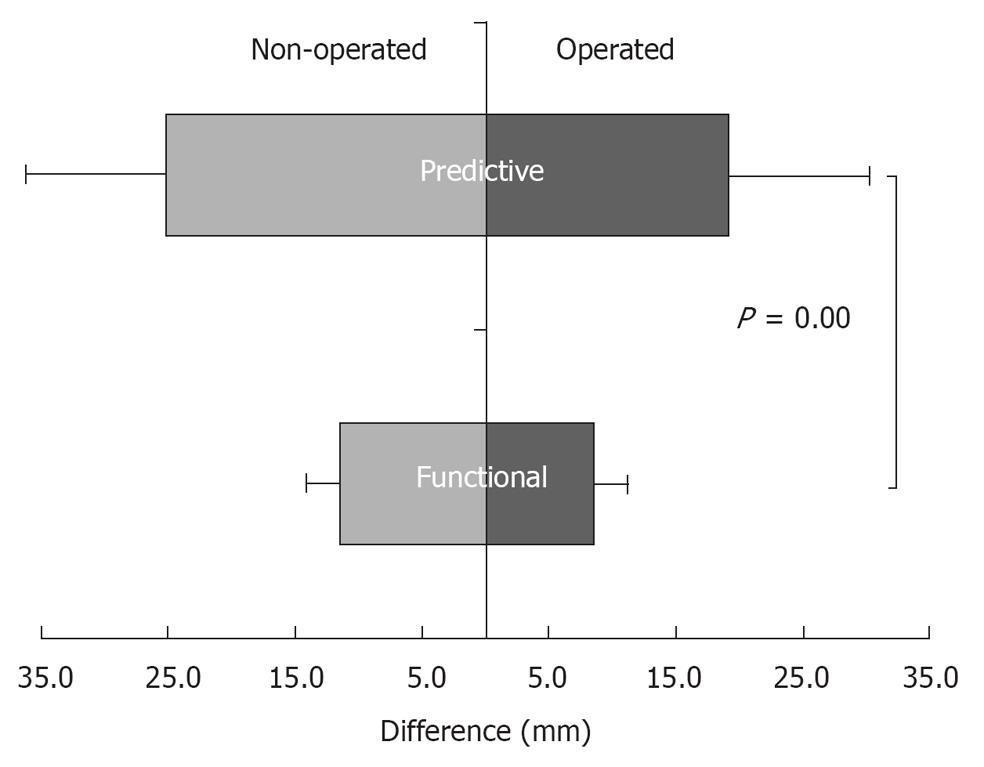
A statistical difference was found for the HJCLE between the predictive and functional method (P = 0.01). No statistical difference was found for the legs (P = 0.07). No interaction was found (Figure 5).
First, this study compared two different approaches, the predictive and functional methods, for estimating the 3D HJC location and compared them with radiographic measurements. Secondly, the HJC location of the operated and non-operated leg was compared in patients with hip arthroplasty.
In the present study, the absence of a statistical difference between the radiographic measurements and the HJC location calculated by the functional method found, supports the idea of the feasibility of determining HJC location with a smaller error in the frontal plane than predictive method in pathological subjects[21]. Previous studies have suggested that the use of the functional approach to determine the HJC location was not appropriate when hip motion is restricted by a pathologic process[24,25]. However Piazza et al[21] demonstrated that even with restricted range of motion, the accuracy of the 3D HJC location is not reduced. Nevertheless, these results were obtained from healthy subjects where data were modified to simulate a pathologic population. In our study, the comparison of HJC locations was performed in hip arthroplasty patients, in whom symmetry of both limbs could not be assumed and hip range of motion was reduced because of the pathologic process around the hip joint. According to our results, the functional approach can easily be integrated in gait analysis and would improve the calculation accuracy in hip joint loading, angles, moments and powers. Moreover, the absence of a statistical difference between the operated and non-operated leg demonstrates that the Score method performs adequately with pathological subjects which consolidate the clinical utilisation of this algorithm.
The statistical difference found for the HJCLE between the predictive and functional methods shows the limit of the predictive method[16,17,26]. In fact, the predictive method is twice less accurate than the functional method when comparing to radiographic measurements. In order to restore hip biomechanics, the surgeon performs pre-operative template during which the contra-lateral normal leg serves as the reference for restoring the normal hip joint anatomy. Despites pre-operative template, hip parameters such as femoral offset, vertical and horizontal centers of rotation and leg length are not always normalized[1-3]. Moreover, anthropometric tables and linear regressions, used in the predictive method, do not take into consideration the new hip geometry and pathological process and therefore cannot correctly estimate the 3D HJC location. Previous studies have shown that errors in HJC location of 20 mm in the frontal plane can lead to underestimation of adduction moment arm of 20%, force of 26% and moments of 40%. This demonstrates the sensitivity of HJC location on gait analysis[27]. No statistical difference was found in HJCLE between the operated and non-operated legs when using the predictive and functional methods. However, it is likely that a larger sample size would lead to significant statistical difference. These results could promote the operated leg with a difference error closer to the radiographic measurements independently of the method used. This might be explained by the assumption that on the operated side, the hip is a ball and socket joint while on the non-operated side the hip might suffer from Osteoarthritis (OA) which affects its geometry. Moreover previous studies[28,29] have reported leg length discrepancy after hip arthroplasty which may compromise the estimation of the 3D HJC location. In both cases, it provides better conditions for HJC calculation of the operated leg.
Some limitations are associated with this study. Firstly, even if the used of three markers, placed in order to define pelvis orientation, is enough to determine the location of the HJC[26], the used of more than three markers could provide redundant information in pelvis and thigh kinematics and consequently reduce soft tissue artefact. Secondly, since radiographic measurements are always taken pre and post- surgery, they could be more useful to improve HJC location. The comparison between radiographic measurements and 3D HJC location from motion analysis software would be facilitate if superior iliac spine were always visible or if two bi-planar normalized radiographic measurements or other 3D medical imaging were available. This would help in locating the HJC in space and it would be easier to corroborate with HJC location given by 3D analysis software. Thirdly, because of the inability of some patients, hip movements were done in a restricted range of motion.
In conclusion, this study showed a HJCD similar to the radiographic measurements and a smaller HJCLE for the functional approach. Furthermore, according to the HJCD and HJCLE no difference was found between the operated and non-operated leg. Patients undergoing hip arthroplasty are a challenging population for the determination of 3D HJC location because their hip geometry and symmetry has been modified by the surgical intervention and the pathological process. In such conditions, the functional method is more accurate than the predictive method in the frontal plane when compared to radiographic measurements. Although being more individualized, the functional method improves 3D HJC localisation and should be used in 3D gait analysis.
We would like also to thank Dr. Payam Farhadnia for the radiographic analyses.
Hip arthroplasty is a well accepted and successful procedure for patients suffering from degenerative hip joint disease. However, the anatomical reconstruction of the hip is not always easy and the insertion of a hip prosthesis may lead to modification of hip geometry. Consequently, these changes affect the hip joint dynamics. In gait analysis, accurate location of the hip joint center (HJC) is crucial for the quantification of the musculoskeletal loading at the hip joint and is one of the key point for the study of post-operative rehabilitation. This aspect is even more important in pathologic subjects, where the hip geometry and symmetry have been modified by the surgery and the pathological process. Improper HJC location can affect hip loading, angles, moments and powers calculation acting at the hip joint.
To knowledge, no study has evaluated the impact of the HJC estimation method on a pathologic population. Moreover, no study has assessed the difference in algorithm performance between the operated and non-operated legs. The purpose of this study is twofold: (1) to compare the precision of 3D location of the HJC obtained by both predictive and functional methods in patients with hip arthroplasty and to compare them with radiographic measurements; and (2) to determine if a difference in HJC location exists between the operated and non-operated leg using the Score algorithm.
The distance between the HJC and the mid-pelvis was calculated and compared between the three approaches. The localisation error between the predictive and functional approach was compared using the radiographic measurements as the reference. The operated leg was compared to the non-operated leg.
A significant difference was found for the distance between the HJC and the mid-pelvis when comparing the predictive and functional method. The functional method leads to fewer errors. A statistical difference was found for the localization error between the predictive and functional method. The functional method is twice more precise. The authors concluded that although being more individualized, the functional method improves HJC localization and should be used in three-dimensional gait analysis.
This is a nice study showing that functional 3D method is accurate in predicting HJC. The methods are valid and it is well written
Peer reviewer: George C Babis, MD, Associate Professor, 1st Orthopaedic Department, University of Athens Medical School, Attikon University Hospital, Rimini 1, Chaidari 12462, Greece
S- Editor Huang XZ L- Editor A E- Editor Zheng XM
| 1. | Johnston RC, Brand RA, Crowninshield RD. Reconstruction of the hip. A mathematical approach to determine optimum geometric relationships. J Bone Joint Surg Am. 1979;61:639-652. [PubMed] [Cited in This Article: ] |
| 2. | Bourne RB, Rorabeck CH. Soft tissue balancing: the hip. J Arthroplasty. 2002;17:17-22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 136] [Cited by in F6Publishing: 149] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 3. | Sakai T, Sugano N, Ohzono K, Nishii T, Haraguchi K, Yoshikawa H. Femoral anteversion, femoral offset, and abductor lever arm after total hip arthroplasty using a modular femoral neck system. J Orthop Sci. 2002;7:62-67. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 50] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Heller MO, Bergmann G, Deuretzbacher G, Claes L, Haas NP, Duda GN. Influence of femoral anteversion on proximal femoral loading: measurement and simulation in four patients. Clin Biomech (Bristol, Avon). 2001;16:644-649. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 75] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Lenaerts G, De Groote F, Demeulenaere B, Mulier M, Van der Perre G, Spaepen A, Jonkers I. Subject-specific hip geometry affects predicted hip joint contact forces during gait. J Biomech. 2008;41:1243-1252. [PubMed] [Cited in This Article: ] |
| 6. | Delp SL, Wixson RL, Komattu AV, Kocmond JH. How superior placement of the joint center in hip arthroplasty affects the abductor muscles. Clin Orthop Relat Res. 1996;137-146. [PubMed] [Cited in This Article: ] |
| 7. | Ehrig RM, Taylor WR, Duda GN, Heller MO. A survey of formal methods for determining the centre of rotation of ball joints. J Biomech. 2006;39:2798-2809. [PubMed] [Cited in This Article: ] |
| 8. | Asla RJD, Deland JT. Anatomy and biomechanics of the foot and ankle. Foot and ankle. Philadelphia, PA: Lippincott Williams and Wilkins 2004; 1-23. [Cited in This Article: ] |
| 9. | Davis RB, DeLuca PA. Clinical gait analysis: current methods and future directions. Current applications and future directions. Piscataway, NJ: IEEE Press 1996; 17-42. [Cited in This Article: ] |
| 10. | Nantel J, Termoz N, Vendittoli PA, Lavigne M, Prince F. Gait patterns after total hip arthroplasty and surface replacement arthroplasty. Arch Phys Med Rehabil. 2009;90:463-469. [PubMed] [Cited in This Article: ] |
| 11. | Sliwinski MM, Sisto SA, Batavia M, Chen B, Forrest GF. Dynamic stability during walking following unilateral total hip arthroplasty. Gait Posture. 2004;19:141-147. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Lenaerts G, Bartels W, Gelaude F, Mulier M, Spaepen A, Van der Perre G, Jonkers I. Subject-specific hip geometry and hip joint centre location affects calculated contact forces at the hip during gait. J Biomech. 2009;42:1246-1251. [PubMed] [Cited in This Article: ] |
| 13. | Madsen MS, Ritter MA, Morris HH, Meding JB, Berend ME, Faris PM, Vardaxis VG. The effect of total hip arthroplasty surgical approach on gait. J Orthop Res. 2004;22:44-50. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 146] [Cited by in F6Publishing: 144] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 14. | Perron M, Malouin F, Moffet H, McFadyen BJ. Three-dimensional gait analysis in women with a total hip arthroplasty. Clin Biomech (Bristol, Avon). 2000;15:504-515. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 172] [Cited by in F6Publishing: 161] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 15. | Mont MA, Seyler TM, Ragland PS, Starr R, Erhart J, Bhave A. Gait analysis of patients with resurfacing hip arthroplasty compared with hip osteoarthritis and standard total hip arthroplasty. J Arthroplasty. 2007;22:100-108. [PubMed] [Cited in This Article: ] |
| 16. | Frigo C, Rabuffetti M. Multifactorial estimation of hip and knee joint centres for clinical application of gait analysis. Gait Posture. 1998;8:91-102. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 38] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Bell AL, Pedersen DR, Brand RA. A comparison of the accuracy of several hip center location prediction methods. J Biomech. 1990;23:617-621. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 591] [Cited by in F6Publishing: 532] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 18. | Leardini A, Cappozzo A, Catani F, Toksvig-Larsen S, Petitto A, Sforza V, Cassanelli G, Giannini S. Validation of a functional method for the estimation of hip joint centre location. J Biomech. 1999;32:99-103. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 308] [Cited by in F6Publishing: 254] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 19. | Ehrig RM, Taylor WR, Duda GN, Heller MO. A survey of formal methods for determining functional joint axes. J Biomech. 2007;40:2150-2157. [PubMed] [Cited in This Article: ] |
| 20. | Piazza SJ, Okita N, Cavanagh PR. Accuracy of the functional method of hip joint center location: effects of limited motion and varied implementation. J Biomech. 2001;34:967-973. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 142] [Cited by in F6Publishing: 117] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 21. | Piazza SJ, Erdemir A, Okita N, Cavanagh PR. Assessment of the functional method of hip joint center location subject to reduced range of hip motion. J Biomech. 2004;37:349-356. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 130] [Cited by in F6Publishing: 107] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 22. | Hoppenfeld S, deBoer P. Surgical exposure in orthopaedics: The anatomic approach. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2003; . [Cited in This Article: ] |
| 23. | Camomilla V, Cereatti A, Vannozzi G, Cappozzo A. An optimized protocol for hip joint centre determination using the functional method. J Biomech. 2006;39:1096-1106. [PubMed] [Cited in This Article: ] |
| 24. | Kirkwood RN, Culham EG, Costigan P. Radiographic and non-invasive determination of the hip joint center location: effect on hip joint moments. Clin Biomech (Bristol, Avon). 1999;14:227-235. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 67] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 25. | Seidel GK, Marchinda DM, Dijkers M, Soutas-Little RW. Hip joint center location from palpable bony landmarks--a cadaver study. J Biomech. 1995;28:995-998. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 148] [Cited by in F6Publishing: 120] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 26. | Hicks JL, Richards JG. Clinical applicability of using spherical fitting to find hip joint centers. Gait Posture. 2005;22:138-145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 62] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 27. | Delp SL, Maloney W. Effects of hip center location on the moment-generating capacity of the muscles. J Biomech. 1993;26:485-499. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 123] [Cited by in F6Publishing: 109] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 28. | Williams O, Fitzpatrick R, Hajat S, Reeves BC, Stimpson A, Morris RW, Murray DW, Rigge M, Gregg PJ. Mortality, morbidity, and 1-year outcomes of primary elective total hip arthroplasty. J Arthroplasty. 2002;17:165-171. [PubMed] [Cited in This Article: ] |
| 29. | Williamson JA, Reckling FW. Limb length discrepancy and related problems following total hip joint replacement. Clin Orthop Relat Res. 1978;135-138. [PubMed] [Cited in This Article: ] |