Published online Oct 18, 2016. doi: 10.5312/wjo.v7.i10.664
Peer-review started: February 16, 2016
First decision: March 24, 2016
Revised: June 20, 2016
Accepted: August 11, 2016
Article in press: August 15, 2016
Published online: October 18, 2016
To evaluate the effect of body mass index (BMI) on short-term functional outcome and complications in primary total knee arthroplasty.
All patients undergoing primary total knee arthroplasty at a single institution between 2007 and 2013 were identified from a prospective arthroplasty database. 2180 patients were included in the study. Age, gender, BMI, pre- and post-operative functional scores [Western Ontario and McMaster University Arthritis Index (WOMAC) and SF-36], complications and revision rate were recorded. Patients were grouped according to the WHO BMI classification. The functional outcome of the normal weight cohort (BMI < 25) was compared to the overweight and obese (BMI ≥ 25) cohort. A separate sub-group analysis was performed comparing all five WHO BMI groups; Normal weight, overweight, class 1 obese, class 2 obese and class 3 obese.
With a mean age of 67.89 (28-92), 2180 primary total knee replacements were included. 64.36% (1403) were female. The mean BMI was 31.86 (18-52). Ninty-three percent of patients were either overweight or obese. Mean follow-up 19.33 mo (6-60 mo). There was no significant difference in pre or post-operative WOMAC score in the normal weight (BMI < 25) cohort compared to patients with a BMI ≥ 25 (P > 0.05). Sub-group analysis revealed significantly worse WOMAC scores in class 2 obese 30.80 compared to overweight 25.80 (P < 0.01) and class 1 obese 25.50 (P < 0.01). Similarly, there were significantly worse SF-36 scores in class 2 obese 58.16 compared to overweight 63.93 (P < 0.01) and class 1 obese 63.65 (P < 0.01) There were 32 (1.47%) superficial infections, 9 (0.41%) deep infections and 19 (0.87%) revisions overall with no complications or revisions in the normal weight cohort (BMI < 25).
Post-operative functional outcome was not influenced by BMI comparing normal weight individuals with BMI > 25. Patients should not be denied total knee arthroplasty based solely on weight alone.
Core tip: We assessed the effect of body mass index (BMI) on short-term functional outcome of 2180 patients that underwent primary total knee arthroplasty at a single institution. Functional outcome was assessed using the Western Ontario and McMaster University Arthritis Index and SF-36 outcome tools. Patients were stratified according to BMI using the WHO classification and results compared. We found no statistical difference in our primary outcome measure, functional outcome of normal weight individuals compared to those with a BMI greater than 25.
- Citation: O’Neill SC, Butler JS, Daly A, Lui DF, Kenny P. Effect of body mass index on functional outcome in primary total knee arthroplasty - a single institution analysis of 2180 primary total knee replacements. World J Orthop 2016; 7(10): 664-669
- URL: https://www.wjgnet.com/2218-5836/full/v7/i10/664.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i10.664
Total knee arthroplasty (TKA) is an effective surgical treatment of osteoarthritis of the knee, with 700000 procedures performed in the United States annually with the demand for TKA projected to increase 673% by 2030[1]. Occurring in tandem with this increase in demand is the exponential increase in obesity in society. Currently in Ireland, 36% of the population are overweight and 14% obese and this is estimated to increase further in the future[2]. It is well established that obesity confers an increased risk for a number of medical conditions including ischaemic heart disease, diabetes and stroke[3]. It has also been shown that obesity increases the risk of development of osteoarthritis, particularly in the knee, which has potential implications for the demand for TKA in the future[4].
Obesity has a number of implications for surgery in general, but in particular for elective surgery such as TKA. Obesity is an independent risk factor for a number of perioperative complications including acute coronary syndrome, wound infection and urinary tract infection[5]. The outcome of obese patients that undergo TKA as compared to non-obese patients is of particular interest. Currently the evidence is unclear with some studies indicating that obese patients achieve inferior outcomes[6] with others showing equivalent functional outcome[7,8].
The aim of this study was to assess the effect of body mass index (BMI) on functional outcome in primary total knee arthroplasty.
Patients that underwent primary total replacement were identified from a prospectively collected joint registry at a single institution. Ethical approval was obtained for the establishment of the joint registry and for on going research. The joint registry is maintained by a full time clinical nurse specialist and all demographic and clinical information for each arthroplasty procedure performed at the institution is prospectively anonymously recorded. Two thousand one hundred and eighty patients were identified during the period 2007-2013. Demographic data including age and gender were collated for each patient. Body mass index (BMI) was calculated for each patient at pre-operative assessment using the standardised formula; weight in kilograms squared, divided by height in metres squared. Functional outcome scores, the Western Ontario and McMaster University Arthritis Index (WOMAC) and the Short Form 36 (SF-36) were collected pre-operatively and 6 mo post operatively. Complications including revision, superficial and deep infection, deep venous thrombosis (DVT) and pulmonary embolism (PE) were recorded prospectively in the postoperative period.
Patients were divided into two comparative groups for the purpose of the study, those with a normal BMI (less than or equal to 25) Group 1 and those who were overweight or obese (greater than 25) Group 2 according to the WHO BMI classification[9]. A separate sub-group analysis was performed comparing all five WHO BMI groups; Normal weight, overweight, class 1 obese, class 2 obese and class 3 obese.
The Primary outcomes assessed were pre-operative and six-month post-operative WOMAC and the SF-36 scores. The WOMAC score is a validated self-administered questionnaire that assesses the condition of patients with hip and knee arthritis. It has a scale of 0 to 100, with a higher score equalling more pain, stiffness and functional limitation[10]. The SF-36 is also a self-administered questionnaire that assesses quality of life. It has a scale of 0 to 100, with a higher score equating to a greater quality of life[11]. Secondary outcomes assessed included complications revision, superficial and deep infection, DVT and PE.
Statistical analysis was performed using STATA Version 12.1. All data was collated on a Microsoft Excel© (Microsoft Corporation, Seattle WA, United States) spreadsheet. Results were analyzed and are presented as mean, percentage and standard deviation for each BMI group according to the WHO classification as appropriate. Statistical significance between the main study groups (normal weight BMI < 25 vs BMI > 25) was assessed using the student t test, with significance set at P < 0.05.
Further sub-group analysis was performed comparing each of the WHO BMI sub-groups. Initially a One-way ANOVA analysis was performed to assess any difference between the groups. Further post-hoc Tukey HSD (honest significance test) analysis was then performed, comparing each of the sub-groups with significance set at P < 0.05. Statistical analysis was performed by Shane O’Neill MD.
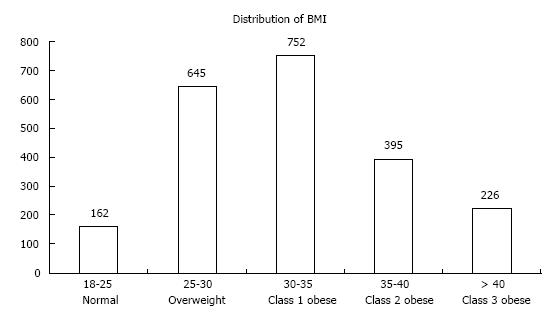
A total of 2180 primary total knee replacements were performed at the institution between 2007 and 2013. The mean age was 67.9 years (28-92), with 36% Male and 64% Female. The mean follow up was 19.3 mo, with a range of 6 mo to 5 years. The distribution according to BMI group is shown in Figure 1. The mean BMI was 31.9 (18-52) with 63% obese, 30% overweight and 7% normal weight. The two comparative study groups consisted of Group 1 (n = 162 patients) and Group 2 (n = 2018 patients).
There was no significant difference in the pre-op WOMAC scores between Group 1; 52.7 (1-84) and Group 2; 53.7 (3-96) (P = 0.5). Similarly, there was no significant difference in the post op scores between the two groups, 29.7 (1-83) and 27 (1-95) (P = 0.075) respectively. There was no significant difference in either the pre-operative (P = 0.83) or post-operative (P = 0.7) SF-36 scores. The complete functional outcome scores are presented in Tables 1 and 2.
| WHO BMI classification | |
| Underweight | < 18.5 |
| Normal range | 18.5-25 |
| Overweight | ≥ 25 |
| Obese | ≥ 30 |
| Class 1 obese | 30-34.9 |
| Class 2 obese | 35-39.9 |
| Class 3 obese | ≥ 40 |
| Group 1 (BMI < 25) | Group 2 (BMI > 25) | ||
| WOMAC scores | |||
| Pre-operative | 52.7 (1-84) | 53.7 (3-96) | P = 0.5 |
| 6 mo post-operative | 29.7 (1-83) | 27 (1-95) | P = 0.075 |
| SF-36 Scores | |||
| Pre-operative | 48.8 (10.4-90.6) | 48.25 (3.3-94.6) | P = 0.83 |
| 6 mo post-operative | 61.34 (1-83) | 62.15 (7.3-99.4) | P = 0.7 |
Table 3 outlines 6-mo post operative functional scores arranged by WHO BMI sub-group in tabular format.
| BMI < 25 | BMI 25-29 | BMI 30-34 | BMI 35-39 | BMI > 40 | |
| Normal | Overweight | Class 1 obese | Class 2 obese | Class 3 obese | |
| WOMAC scores | |||||
| 6 mo post-operative | 29.67 | 25.8 | 25.5 | 30.8 | 28.6 |
| SF-36 Scores | |||||
| 6 mo post-operative | 61.34 | 63.93 | 63.65 | 58.16 | 58.47 |
WOMAC: Initial One-way ANOVA analysis of the six-month post operative WOMAC scores between the 5 groups revealed a P-value < 0.01, suggesting a significant difference between one or more groups. Further post-hoc Tukey HSD testing revealed significant differences in the 6 mo postoperative WOMAC scores comparing BMI 25-29 (overweight) 25.80 vs BMI 35-39 (class 2 obese) 30.80 (P < 0.01) and BMI 30-34 (class 1 obese) 25.50 vs BMI 35-39 (class 2 obese) 30.80 (P < 0.01). There was no significant difference in post operative WOMAC scores in the other BMI subgroup analysis.
SF-36: Initial One-way ANOVA analysis of the six month post operative SF-36 scores between the 5 groups revealed a P-value < 0.01, suggesting a significant difference between one or more groups. Further post-hoc Tukey HSD Testing revealed significant differences in the six month postoperative SF-36 scores comparing BMI 25-29 (overweight) 63.93 vs BMI 35-39 (class 2 obese) 58.16 (P < 0.01) and BMI 30-34 (class 1 obese) 63.65 vs BMI 35-39 (class 2 obese) 58.16 (P < 0.01). There was no significant difference in post operative SF-36 scores in the other BMI sub-group analysis.
There were no complications in Group 1 (n = 162) at latest follow-up. There were 19 (0.87%) revisions, 32 (1.47%) superficial infections, 9 (0.41%) deep infections, 10 (0.46%) DVTs and 9 (0.41%) PEs in Group 2 (n = 2018) over the same mean follow-up. The absolute number of complications was not sufficient to perform a meaningful statistical analysis.
Overall the study revealed no significant difference in short-term post-operative functional outcome in patients with a normal BMI as compared to overweight or obese patients. Sub-group analysis found significantly lower functional outcome scores in class 2 obese patients (BMI 35-39.9) compared to both overweight and class 1 obese patient.
The study highlights that, the vast majority of patients now presenting to our institution for total knee replacement, 93% are either overweight or obese. This is significantly higher than the baseline levels in the general population, where 50% are either overweight or obese[2]. This finding is mirrored in previous studies, which also revealed a considerable proportion of patients undergoing total knee arthroplasty are now obese[12]. According to the latest National joint registry in the United Kingdom (NJR) figures (2013), the mean BMI of patients undergoing TKA in the United Kingdom is now 30.8 (Class 1 obese)[13]. This underlines the significant burden that this increase in BMI will place on orthopaedic services now and in the future.
The principle finding in this study of equivalent functional outcome comparing normal weight BMI < 25 individuals with BMI > 25 is in keeping with a recent study of 13673 primary total knee replacements by Baker et al[14] using NJR data. They found that the improvement of patient reported outcomes (PROMs) were similar irrespective of BMI. Similarly, Desmukh et al[15] revealed no correlation with BMI and functional outcome at 1 year. However, a consensus has yet to be reached in the literature, as there is also evidence that increasing BMI, particularly greater than 40 results in inferior clinical outcomes. Collins et al[16] reviewed 445 total knee replacements and found inferior clinical outcome scores in individuals with a BMI greater than 30 at 9 years follow up. Interestingly, although obese patients achieved lower outcome scores as compared to non-obese patients, they achieved significant absolute functional improvement and the authors concluded that they “found no reason to limit access to total knee replacement in obese patients”. While there was no difference in our main outcome measure, the sub-group analysis revealed significantly worse functional outcomes in the class 2 obese cohort compared to both the overweight and class 1 obese cohort. Interestingly the class 3 obese cohort did not demonstrate any significant difference in functional outcome scores. All cohorts achieved significant absolute improvements in functional outcome measures compared to preoperative values. The significance of our finding of inferior outcomes in the class 2 cohort is unclear. While we have included a relatively large cohort in this study (2180), perhaps larger numbers found in registry studies are necessary to define clear sub-group differences.
Despite no difference in functional outcome, the incidence of all complications was higher in the overweight and obese cohort as compared to the normal weight cohort. The evidence in the literature is clear in relation to the increased risk of perioperative complications with increasing BMI in TKA. The aetiology behind this is multifactorial. Wound healing and the development of both superficial and deep peri-prosthetic joint infections are significantly more common with increasing BMI. A recent meta-analysis by Kerkhoffs et al[17] revealed an odds ratio of 1.9 for all infection and 2.38 for deep infection in obese patients as compared to non-obese patients in an analysis of 15276 and 5061 patients respectively. Obese patients are also at a higher risk of thromboembolic disease post operatively[18]. It is imperative that patients are counselled in detail regarding the increased risk of perioperative complications with increasing BMI. While it would seem intuitive that patients should attempt to lose weight prior to surgery, some recent evidence suggests that obese patients that lose a significant proportion of bodyweight preoperatively, actually have a higher rate of surgical site infection compared to control[19]. Further research is needed in relation to perioperative weight management, however it raises interesting questions about the best way to manage this ever-expanding cohort of overweight and obese patients.
Due to the current demographics of our patient cohort, there were relatively few normal weight individuals presenting for surgery and therefore available for inclusion in the study. Similarly, larger studies using registry data may be necessary to elucidate clear sub-group differences. While the patient numbers were sufficient to statistically compare the functional outcome scores, there was an insufficient incidence of complications to draw any statistical conclusions in relation to complication differences. We acknowledge that early functional outcome may not correspond to long-term functional outcome and further research in this area is required.
In conclusion, overall there was no difference in early post-operative functional outcome comparing normal weight individuals with those of a BMI > 25 in a cohort of 2080 primary total knee replacements. Patients should be counselled regarding the potential increased risk of complications with increasing BMI, however they should not be denied TKA based solely on weight if medically fit to undergo the procedure.
The demand for total knee arthroplasty is increasing year on year and is projected to increase further in the future. Parallel to this the average weight of individuals is also increasing year on year. This directly corresponds to an increase in demand for total knee replacement (TKR), as increasing weight is associated with increased risk of symptomatic degenerative change in the knee. It is therefore imperative that the authors study the efficacy and safety of performing TKR on this patient cohort.
The author’s group perform high volume multi-surgeon arthroplasty at a single dedicated unit. This paper provides evidence for the efficacy for TKR in this patient cohort irrespective of body mass index (BMI).
Recent innovations in perioperative pain management and the enhanced recovery protocol have had a positive impact in decreasing length of stay and rehab potential for patients undergoing this procedure. This is particularly relevant to overweight and obese individuals for whom it imperative that they mobilise early to try and minimise the risk of perioperative complications.
Patients with severe degenerative change affecting their quality of life and mobility can benefit from total knee arthroplasty. The procedure can transform a patient’s life, relieving them of chronic pain and improving mobility.
TKR involves the replacement of the worn surfaces of the distal femur and proximal tibia and replacement with prosthetic implants, which can be secured with or without cement.
This is an interesting clinical study concerning the effect of BMI on functional outcome and complications in primary total knee arthroplasty.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Ireland
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Cui QT, De Fine M, Drosos GI, Fernandez-Fairen M, Hasegawa M S- Editor: Qiu S L- Editor: A E- Editor: Lu YJ
| 1. | Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780-785. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2079] [Cited by in F6Publishing: 3103] [Article Influence: 182.5] [Reference Citation Analysis (0)] |
| 2. | Morgan KMH, Watson D, Perry I, Barry M, Shelley E, Harrington J, Molcho M, Layte , RTN , van Lente E. SLAN 2007 Survey of lifestyle attitudes and nutrition in Ireland. Main Report. Dublin: Department of Health and Children 2007; . [Cited in This Article: ] |
| 3. | Bray GA. Overweight is risking fate. Definition, classification, prevalence, and risks. Ann N Y Acad Sci. 1987;499:14-28. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 187] [Cited by in F6Publishing: 199] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 4. | Felson DT, Anderson JJ, Naimark A, Walker AM, Meenan RF. Obesity and knee osteoarthritis. The Framingham Study. Ann Intern Med. 1988;109:18-24. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 747] [Cited by in F6Publishing: 693] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 5. | Bamgbade OA, Rutter TW, Nafiu OO, Dorje P. Postoperative complications in obese and nonobese patients. World J Surg. 2007;31:556-560; discussion 561. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 222] [Cited by in F6Publishing: 236] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 6. | Foran JR, Mont MA, Rajadhyaksha AD, Jones LC, Etienne G, Hungerford DS. Total knee arthroplasty in obese patients: a comparison with a matched control group. J Arthroplasty. 2004;19:817-824. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 122] [Cited by in F6Publishing: 117] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 7. | Amin AK, Patton JT, Cook RE, Brenkel IJ. Does obesity influence the clinical outcome at five years following total knee replacement for osteoarthritis? J Bone Joint Surg Br. 2006;88:335-340. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 114] [Cited by in F6Publishing: 122] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 8. | Spicer DD, Pomeroy DL, Badenhausen WE, Schaper LA, Curry JI, Suthers KE, Smith MW. Body mass index as a predictor of outcome in total knee replacement. Int Orthop. 2001;25:246-249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 146] [Cited by in F6Publishing: 157] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 9. | WHO. Global database on Body Mass Index: BMI Classification. Geneva: World Health Organization 2006; . [Cited in This Article: ] |
| 10. | WOMAC Osteoarthritis Index User Guide. Version V. Australia: Brisbane 2002; . [Cited in This Article: ] |
| 11. | Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473-483. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23352] [Cited by in F6Publishing: 22722] [Article Influence: 710.1] [Reference Citation Analysis (0)] |
| 12. | Kremers HM, Visscher SL, Kremers WK, Naessens JM, Lewallen DG. The effect of obesity on direct medical costs in total knee arthroplasty. J Bone Joint Surg Am. 2014;96:718-724. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 63] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 13. | National Joint Registry. National Joint Registry Annual Report, 2014. Available from: http://www.hqip.org.uk/resources/national-joint-registry-annual-report-2014/. [Cited in This Article: ] |
| 14. | Baker P, Petheram T, Jameson S, Reed M, Gregg P, Deehan D. The association between body mass index and the outcomes of total knee arthroplasty. J Bone Joint Surg Am. 2012;94:1501-1508. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 15. | Deshmukh RG, Hayes JH, Pinder IM. Does body weight influence outcome after total knee arthroplasty? A 1-year analysis. J Arthroplasty. 2002;17:315-319. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 89] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | Collins RA, Walmsley PJ, Amin AK, Brenkel IJ, Clayton RA. Does obesity influence clinical outcome at nine years following total knee replacement? J Bone Joint Surg Br. 2012;94:1351-1355. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 63] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 17. | Kerkhoffs GM, Servien E, Dunn W, Dahm D, Bramer JA, Haverkamp D. The influence of obesity on the complication rate and outcome of total knee arthroplasty: a meta-analysis and systematic literature review. J Bone Joint Surg Am. 2012;94:1839-1844. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 334] [Cited by in F6Publishing: 350] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 18. | Mantilla CB, Horlocker TT, Schroeder DR. Risk factors for clinically relevant pulmonary embolism and deep venous thrombosis in patients undergoing primary hip or knee arthroplasty. Anesthesiology. 2003;99:552-560. [PubMed] [Cited in This Article: ] |
| 19. | Inacio MC, Kritz-Silverstein D, Raman R, Macera CA, Nichols JF, Shaffer RA, Fithian DC. The risk of surgical site infection and re-admission in obese patients undergoing total joint replacement who lose weight before surgery and keep it off post-operatively. Bone Joint J. 2014;96-B:629-635. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |