Published online Sep 18, 2016. doi: 10.5312/wjo.v7.i9.546
Peer-review started: April 26, 2016
First decision: June 16, 2016
Revised: June 23, 2016
Accepted: July 11, 2016
Article in press: July 13, 2016
Published online: September 18, 2016
Periprosthetic joint infections (PJI) of the hip and the knee are grossly classified as early post-operative, acute hematogenous and late chronic infections. Whereas two-stage exchange arthroplasty is the standard of care in North America for treating chronic infections, irrigation and debridement (I and D) with retention of implants has been used in an attempt to treat the other two types of PJIs. The rationale of this approach is that a PJI may be eradicated without the need of explanting the prostheses, as long as it has not transitioned into a chronic state. With the present paper, we review current evidence regarding the role of I and D with implant retention for treating PJIs of the hip and the knee. While a very wide range of success rates is reported in different studies, a short period of time between initiation of symptoms and intervention seems to play a prominent role with regards to a successful outcome. Moreover, pathogens of higher virulence and resistance to antibiotics are associated with a poorer result. Specific comorbidities have been also correlated with a less favorable outcome. Finally, one should proceed with serial I and Ds only under the condition that a predefined, aggressive protocol is applied. In conclusion, when treating a PJI of the hip or the knee, all the above factors should be considered in order to decide whether the patient is likely to benefit from this approach.
Core tip: An infected total joint arthroplasty represents a significant burden to patients, as well as to orthopaedic surgeons. Previously, irrigation and debridement with retention of implants has been advocated for certain types of periprosthetic infections. The purpose of the present paper is to review the indications, success rates and factors determining the outcome of this treatment option for periprosthetic infections of the hip and the knee.
- Citation: Triantafyllopoulos GK, Soranoglou V, Memtsoudis SG, Poultsides LA. Implant retention after acute and hematogenous periprosthetic hip and knee infections: Whom, when and how? World J Orthop 2016; 7(9): 546-552
- URL: https://www.wjgnet.com/2218-5836/full/v7/i9/546.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i9.546
Total joint arthroplasty (TJA) is a very useful tool in the hands of orthopaedic surgeons, as it can relieve symptoms and significantly improve the quality of life in patients with end-stage arthritis of the hip and the knee. In the past decades, the use of this modality has known a remarkable growth, which is expected to continue in the future. For example, by the year 2020 the estimated annual number of total hip arthroplasties (THAs) will exceed 500000 procedures[1]. On the other hand, this will also lead to an increase in complications related with TJA, among which periprosthetic joint infection (PJI) is one of the most devastating for the patient. In spite of preventive measures available, the incidence of PJI remains substantial as it ranges from 1% to 3% after primary TJA[2-5], and can be 4 times greater after revision TJA[6].
Implant colonization may occur with either intraoperative contamination, spreading from an adjacent infectious site or hematogenous seeding from a distant site[7], with coagulase-negative staphylococci and Staphylococcus aureus species being the most dominant pathogens[8-11]. Diagnosis can be easily made when obvious sequelae of infection are present, such as a draining sinus. However, in many cases such signs are absent and a complex diagnostic evaluation is needed. No single method provides 100% diagnostic specificity and sensitivity. The Musculoskeletal Infection Society introduced specific criteria for the diagnosis of a PJI[12]. The combination of different modalities significantly increase sensitivity and specificity for diagnosing PJI[13,14]. Moreover, synovial biomarkers, including alpha-defensin and leukocyte esterase, have been proven accurate diagnostic tools for PJI with high sensitivity and specificity[15]. Nonetheless, sophisticated methods are expensive and not widely available, and therefore cannot be recommended for routine use.
PJIs of the hip are classified into four types, as proposed by Tsukayama et al[16]. Type I includes positive intraoperative cultures in patients undergoing revision surgery for non-infectious etiology; Type IIrepresents early infections developing within one month post-operatively; late infections presenting within more than one month postoperatively are characterized as Type III infections; finally, Type IV infections are of acute hematogenous nature and are correlated with an identifiable event leading to bacteremia. A similar system has been introduced for PJIs of the knee[17]: Type I includes positive intraoperative cultures obtained during a revision surgery for a cause other than infection; Type II PJIs are early infections presenting within 4 wk after surgery and include Types IIA (superficial) and IIB (deep); acute hematogenous deep infections with an onset of more than 4 wk postoperatively are classified as Type III infections; lastly, Type IV PJIs of the knee are late deep infections developing after 4 wk since the index procedure.
The standard of treatment for PJI is a combination of surgical interventions with the goal of reducing microbial load and administration of antibiotics. Two-stage revision is considered to be the gold standard for management of late chronic PJIs in North America[18]. On the other hand, eradicating infection with retention of the prosthesis when possible may be associated with superior functional outcomes. Irrigation and debridement (I and D) with exchange of prosthetic modular parts has been long used with respect to that goal. The purpose of the present paper is to review the indications, success rates and risk factors that determine the outcome of I and D for PJIs of the hip and the knee.
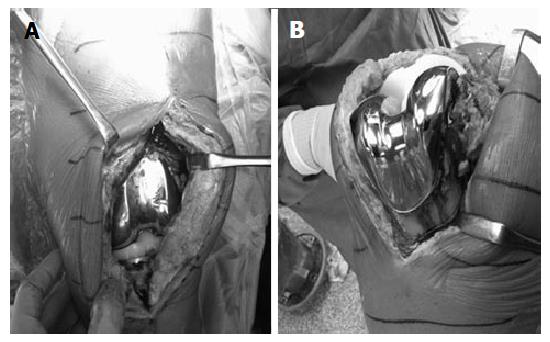
The patient should be off any antibiotics for at least 5 d before the procedure. The affected limb is prepped and draped, the previously healed incision is used and the affected joint is adequately exposed (Figure 1A). A total number of six tissue samples should be obtained and sent for cultures and sensitivity testing. Next, the modular parts, including femoral head and polyethylene liner for a THA and the polyethylene liner for TKA, are removed to gain access to all aspects of the joint and a thorough debridement is performed. All grossly infected and necrotic soft-tissues are meticulously excised (Figure 1B). Great care should be taken to circumferentially debride the articular capsule in both the hip and the knee. After the joint is debrided to macroscopically healthy tissues, the joint is copiously irrigated with antibiotic containing saline. Modular parts are exchanged and the wound is closed. It should be noted that even though exchange of modular parts is advised[18], it may not be always feasible, especially in settings where implant availability is limited. There is no consensus on the duration of intravenous antibiotics administration after the procedure[19]. A common approach is to place the patient on a 6 wk treatment with antibiotics (two weeks of intravenously administered antibiotics followed by another 4 wk of p.o. antibiotics), based on culture and sensitivity results.
The technique described above is the open technique with exchange of modular parts. In the previous years, there was a trend towards performing I and D arthroscopically, especially for periprosthetic infections of the knee[20,21]. However, recently there has been a recommendation against this approach, as it does not allow access to all aspects of the joint and therefore the debridement may be suboptimal[22].
Previously, Del Pozo et al[23] have outlined the indications of I and D for treating PJIs. According to the authors, these include an infected prosthesis that was implanted within less than 3 mo or a hematogenous infection, with duration of symptoms of less than 3 wk, absence of sinus tract or abscess, stability of implants and a pathogen other than multi-drug resistant microorganisms, Enterococcus species, quinolone-resistant Pseudomonas and fungi.
Recently, the participants of a consensus meeting on periprosthetic infections strongly agreed that I and D may be a viable alternative for patients with early infections that develop within 3 mo post index procedure, as well as with late hematogenous infections; symptoms should have a duration of less than 3 wk[19]. Eradicating infection while avoiding removal of the prostheses may allow for lower morbidity and better function. Published series of patients treated with I and D for PJI of the hip and the knee show great variability in methodology, success rates and identified prognostic factors with regards to outcome.
Implant retention with I and D of the hip for a Type IIor IV PJI has been previously reported to be 70% in a previous large series[24]. Westberg et al[25] have reported a 71% success rate of I and D in early hip PJIs. In the series of Tsukayama et al[16], retention of implants was attained in 70.3% of cases. Barberán et al[26] had a success rate of 71.9%, and Vilchez et al[27] reported that I and D successfully treated infection with implant retention in 75.5% of patients. On the other hand, other authors have published greatly variable results, with success rates ranging from 14% to 100%[21,28-46] (Table 1).
| Ref. | Patients | Success rate for PJI of the hip | Success rate for PJI of the knee | Cumulative success rate |
| Aboltins et al[28] | 13 | 92% | 85.70% | 90% |
| Azzam et al[29] | 53 | 47.83% | 45.30% | 44.60% |
| Barberán et al[26] | 32 | 71.90% | 57.20% | 65% |
| Bradbury et al[52] | 19 | - | 16% | - |
| Brandt et al[30] | 7 | 28.60% | 38.50% | 36.40% |
| Buller et al[40] | 62 | 56.50% | 50.60% | 51.80% |
| Burger et al[49] | 39 | - | 17.90% | - |
| Byren et al[21] | 52 | 86.50% | 74.50% | 80.60% |
| Chiu et al[51] | 40 | - | 30% | - |
| Choi et al[31] | 92 | 50% | - | - |
| Choong et al[32] | 14 | 78.60% | - | - |
| Cierny et al[48] | 43 | - | - | 66% |
| Crockarell et al[44] | 42 | 14% | - | - |
| Engesæter et al[46] | 180 | 76% | - | - |
| Estes et al[37] | 20 | 100% | 87.50% | 90% |
| Fehring et al[43] | 86 | 37.50% | 37% | 37.20% |
| Gardner et al[50] | 44 | - | 43.20% | - |
| Geurts et al[45] | 69 | 82.60% | 85% | 83.10% |
| Klouche et al[63] | 12 | 75% | - | - |
| Konigsberg et al[33] | 20 | 80% | 77.30% | 78.50% |
| Koyonos et al[41] | 60 | 30% | 38.50% | 35% |
| Kuiper et al[42] | 62 | 61.30% | 75.90% | 66% |
| Marculescu et al[56] | 91 | - | - | 60% |
| Martel-Lafarrière et al[59] | 34 | - | - | 60% |
| Martínez-Pastor et al[34] | 15 | 73.30% | 75% | 74.50% |
| Meehan et al[35] | 19 | 66.70% | 100% | 89.55% |
| Mont et al[53] | 24 | - | 83.30% | - |
| Peel et al[60] | 43 | 71.40% | 93% | 79.10% |
| Rasouli et al[38] | 10 | 83.30% | 0% | 50% |
| Segawa et al[55] | 28 | - | 78% | - |
| Sukeik et al[36] | 26 | 77% | - | - |
| Tattevin et al[57] | 69 | - | - | 38.20% |
| Teeny et al[54] | 21 | - | 29% | - |
| Triantafyllopoulos et al[47] | 78 | - | 55.10% | - |
| Triantafyllopoulos et al[24] | 60 | 70% | - | - |
| Tsukayama et al[16] | 106 | 70.30% | - | - |
| Van Kleunen et al[61] | 13 | - | - | 61.50% |
| Vilchez et al[27] | 18 | 88.90% | 68.60% | 75.50% |
| Westberg et al[25] | 38 | 71% | - | - |
| Zürcher-Pfund et al[20] | 21 | - | 33% | - |
Symptom duration is a significant factor predicting the outcome of I and D of the hip. When a cut-off point of 5 d of symptom duration was used, it was noted that patients with symptoms of more than 5 d had 95.2% lower odds of success compared to patients with shorter duration of symptoms[24]. Similarly, Sukeik et al[36] found that performing I and D more than 5 d after the onset of symptoms led to less favorable outcomes. Others have proposed an even prompter intervention, in as shortly as within 2 d from symptom onset[30]. In other studies, the suggested duration of symptoms within which such an intervention is more probable to be successful ranges from one to four weeks[40,42,45]. Despite this variability, we may conclude that once the diagnosis of a type II or IV PJI of the hip is established, action should be prompt from the part of the surgeon when the goal is to retain the implants. The decrease in the probability of successful I and D has been calculated to be 17.7% for each additional day of delay in treatment[24]. A greater duration of symptoms allows formation of the biofilm layer, which provides protection against immune response and resistance against antibiotics. Once this biofilm is formed, I and D with implant retention is less probable to control the infection[43].
The type of pathogen also plays a role in the outcomes of I and D of the hip. Patients with methicillin-resistant staphylococci have been correlated with worse outcomes[24]. Barberán et al[26] also reported worse outcomes in patients infected with methicillin-resistant Staphylococcus aureus (MRSA). In addition, infections with MRSA, methicillin-resistant Staphylococcus epidermidis and vancomycin-resistant Enterococci have been associated with inferior success rates after I and D[40]. Staphylococcal infections have been identified as a negative prognostic factor by other investigators as well[21,29,31,41,42]. In cases of infections with multi-drug resistant pathogens, a more aggressive treatment strategy is warranted and even exchange arthroplasty (either in one or two stages) may be considered.
Other factors that have been found to predict outcomes of I and D of the hip include obesity[24], ASA score and purulence[29], a history of previous infection[40] and elevated inflammatory markers[27,34,40,42]. These factors are associated either with host’s impaired immune system response to infection, or with severity of infections and should be considered for decision-making. Additionally, patients with one or more local or systemic compromises according to the Cierny classification have been also correlated with inferior outcomes after I and D for a PJI of the hip[48].
Buller et al[40], in their large series of 247 patients with PJI of the knee, reported a success rate of 50.6% for I and D. Similarly, in a series of 78 patients with PJI of the knee treated with I and D, the success rate was found to be 56.3%[47]. A higher success rate (74.5%) was reported by Byren et al[21] among 51 patients with PJI of the knee. In contrast, in the study of Koyonos et al[41], I and D was successful in only 38.5%. In the literature, there are studies with highly variable success rates, that range from 16% to 100%[20,26-30,33-35,37,42,43,45,49-55] (Table 1). These studies, however, show significant methodological inconsistencies.
Similarly to the hips, duration of symptoms is also identified as a factor predicting the outcomes of I and D. In studies where PJIs of both the hip and the knee were included, favorable outcomes were reported when the intervention was undertaken within an interval ranging from 1-4 wk[40,42,45,56]. In other reports, the suggested timing for a successful outcome is within 5 d since symptom onset[47,57]. Others have proposed an even lower cut-off point of 2 d[30]. For each additional day that treatment delays, a 7.5% decrease in the odds of success has been calculated[47]. This highlights the importance of timely intervention, as the gradual formation of the protective biofilm may prevent eventual eradication of the pathogen without removal of the prosthesis.
The type of pathogen also predicts outcomes of I and D in the setting of a PJI of the knee. As is the case for the hip, MRSA infections have been associated with poorer outcomes[26,40,47]. Treatment failure has been correlated with staphylococcal infections in several previous reports[21,29,33,41,56]. This may be explained by the higher microorganism virulence[58], the formation of biofilm and the increased rates of resistance to antibiotics that characterize staphylococcal strains.
For PJI of the knee, ASA score and joint purulence[29,56,59], preoperative levels of inflammatory markers[34,40,42], and prior infection[40] have been also identified as factors affecting outcomes of I and D. In contrast to the hip, revision surgery[21], as well as thyroid disease[47], has been reported as additional prognostic factors for I and D of a knee PJI.
In a previous consensus meeting, the participants recommended against performing serial I and Ds, unless this approach is included in a specific protocol[22]. Studies utilizing a predefined protocol of serial interventions exhibit high success rates. When gentamycin-loaded cement beads were used in combination with a repeat I and D after 2 wk, infection control was established in 83.1% of patients[45]. Kuiper et al[42] used a similar protocol, with a success rate of 66.1%. A more aggressive approach was adopted by Peel et al[60], which included three I and Ds within 7-10 d; the authors reported an 86% success rate. Estes et al[37] performed 2 I and Ds 7 d apart using antibiotic-loaded cement beads and reported a 90% success rate. With a protocol consisting at least 2 I and Ds within 2-3 d, Choong et al[32] reported successful outcomes in 78.6% of patients. On the other hand, in studies where no particular protocol for performing serial I and Ds is followed, the results have been more variable and range from 25% to 100%[20,21,25,27-29,31,36,53,61,62].
Time is still a significant factor when the approach of serial I and Ds is chosen. It has been shown that performing a subsequent I and D within more than 20 d after the first procedure is associated with 97.4% lower odds of implant retention[62]. Specific protocols with serial I and Ds involve performing the subsequent procedure in no more than 14 d and, as already described, were associated with superior results. Again, longer duration of symptoms has been also associated with failure of multiple I and Ds[62] as it allows for biofilm formation and transition to infection chronicity, as previously described.
Serial I and Ds have been found less likely to be of success in PJIs of the knee than in hip infections[62]. This may be attributed to differences with regards to the soft-tissue envelope of each joint, as well as to vascular supply. In the same study, patients treated with multiple I and Ds were more likely to have vascular disease[62]. These findings, however, have not been reproduced by other reports and therefore further investigation is needed in order to elucidate their potential impact.
I and D with the goal of implant retention is still an important tool in the armamentarium of the orthopaedic surgeon for early postoperative and late acute hematogenous PJIs. In such cases, intervention should be timely and aggressive, as each additional day lowers the odds for a successful outcome. Furthermore, the ideal candidate should have an infection with a low-virulence pathogen and be without comorbidities that have been associated with a less favorable result. Finally, after one failed I and D, the surgeon should be very cautious about repeating the procedure, unless a structured and aggressive protocol incorporating serial I and Ds within a short time interval is applied.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Buttaro MA, Fenichel I S- Editor: Ji FF L- Editor: A E- Editor: Li D
| 1. | Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014;96:624-630. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 623] [Cited by in F6Publishing: 633] [Article Influence: 63.3] [Reference Citation Analysis (0)] |
| 2. | Salvati EA, González Della Valle A, Masri BA, Duncan CP. The infected total hip arthroplasty. Instr Course Lect. 2003;52:223-245. [PubMed] [Cited in This Article: ] |
| 3. | Hanssen AD, Rand JA. Evaluation and treatment of infection at the site of a total hip or knee arthroplasty. Instr Course Lect. 1999;48:111-122. [PubMed] [Cited in This Article: ] |
| 4. | Phillips JE, Crane TP, Noy M, Elliott TS, Grimer RJ. The incidence of deep prosthetic infections in a specialist orthopaedic hospital: a 15-year prospective survey. J Bone Joint Surg Br. 2006;88:943-948. [PubMed] [Cited in This Article: ] |
| 5. | Peersman G, Laskin R, Davis J, Peterson M. Infection in total knee replacement: a retrospective review of 6489 total knee replacements. Clin Orthop Relat Res. 2001;15-23. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 555] [Cited by in F6Publishing: 485] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 6. | Mortazavi SM, Molligan J, Austin MS, Purtill JJ, Hozack WJ, Parvizi J. Failure following revision total knee arthroplasty: infection is the major cause. Int Orthop. 2011;35:1157-1164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 127] [Cited by in F6Publishing: 135] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 7. | Zimmerli W, Ochsner PE. Management of infection associated with prosthetic joints. Infection. 2003;31:99-108. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 264] [Cited by in F6Publishing: 273] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 8. | Bjerke-Kroll BT, Christ AB, McLawhorn AS, Sculco PK, Jules-Elysée KM, Sculco TP. Periprosthetic joint infections treated with two-stage revision over 14 years: an evolving microbiology profile. J Arthroplasty. 2014;29:877-882. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 80] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 9. | Stefánsdóttir A, Johansson D, Knutson K, Lidgren L, Robertsson O. Microbiology of the infected knee arthroplasty: report from the Swedish Knee Arthroplasty Register on 426 surgically revised cases. Scand J Infect Dis. 2009;41:831-840. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 106] [Cited by in F6Publishing: 119] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 10. | Nickinson RS, Board TN, Gambhir AK, Porter ML, Kay PR. The microbiology of the infected knee arthroplasty. Int Orthop. 2010;34:505-510. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 81] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Moran E, Masters S, Berendt AR, McLardy-Smith P, Byren I, Atkins BL. Guiding empirical antibiotic therapy in orthopaedics: The microbiology of prosthetic joint infection managed by debridement, irrigation and prosthesis retention. J Infect. 2007;55:1-7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 146] [Cited by in F6Publishing: 163] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 12. | Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res. 2011;469:2992-2994. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1212] [Cited by in F6Publishing: 1317] [Article Influence: 101.3] [Reference Citation Analysis (1)] |
| 13. | Kwee TC, Kwee RM, Alavi A. FDG-PET for diagnosing prosthetic joint infection: systematic review and metaanalysis. Eur J Nucl Med Mol Imaging. 2008;35:2122-2132. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 110] [Cited by in F6Publishing: 98] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 14. | Gemmel F, Van den Wyngaert H, Love C, Welling MM, Gemmel P, Palestro CJ. Prosthetic joint infections: radionuclide state-of-the-art imaging. Eur J Nucl Med Mol Imaging. 2012;39:892-909. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 133] [Cited by in F6Publishing: 139] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 15. | Wyatt MC, Beswick AD, Kunutsor SK, Wilson MJ, Whitehouse MR, Blom AW. The Alpha-Defensin Immunoassay and Leukocyte Esterase Colorimetric Strip Test for the Diagnosis of Periprosthetic Infection: A Systematic Review and Meta-Analysis. J Bone Joint Surg Am. 2016;98:992-1000. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 136] [Cited by in F6Publishing: 140] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 16. | Tsukayama DT, Estrada R, Gustilo RB. Infection after total hip arthroplasty. A study of the treatment of one hundred and six infections. J Bone Joint Surg Am. 1996;78:512-523. [PubMed] [Cited in This Article: ] |
| 17. | Tsukayama DT, Goldberg VM, Kyle R. Diagnosis and management of infection after total knee arthroplasty. J Bone Joint Surg Am. 2003;85-A Suppl 1:S75-S80. [PubMed] [Cited in This Article: ] |
| 18. | Windsor RE. Management of total knee arthroplasty infection. Orthop Clin North Am. 1991;22:531-538. [PubMed] [Cited in This Article: ] |
| 19. | Haasper C, Buttaro M, Hozack W, Aboltins CA, Borens O, Callaghan JJ, de Carvalho PI, Chang Y, Corona P, Da Rin F. Irrigation and debridement. J Arthroplasty. 2014;29:100-103. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Zürcher-Pfund L, Uçkay I, Legout L, Gamulin A, Vaudaux P, Peter R. Pathogen-driven decision for implant retention in the management of infected total knee prostheses. Int Orthop. 2013;37:1471-1475. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 21. | Byren I, Bejon P, Atkins BL, Angus B, Masters S, McLardy-Smith P, Gundle R, Berendt A. One hundred and twelve infected arthroplasties treated with ‘DAIR’ (debridement, antibiotics and implant retention): antibiotic duration and outcome. J Antimicrob Chemother. 2009;63:1264-1271. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 274] [Cited by in F6Publishing: 276] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 22. | Parvizi J, Gehrke T, Chen AF. Proceedings of the International Consensus on Periprosthetic Joint Infection. Bone Joint J. 2013;95-B:1450-1452. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 632] [Cited by in F6Publishing: 649] [Article Influence: 59.0] [Reference Citation Analysis (0)] |
| 23. | Del Pozo JL, Patel R. Clinical practice. Infection associated with prosthetic joints. N Engl J Med. 2009;361:787-794. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 611] [Cited by in F6Publishing: 548] [Article Influence: 36.5] [Reference Citation Analysis (0)] |
| 24. | Triantafyllopoulos GK, Poultsides LA, Sakellariou VI, Zhang W, Sculco PK, Ma Y, Sculco TP. Irrigation and debridement for periprosthetic infections of the hip and factors determining outcome. Int Orthop. 2015;39:1203-1209. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 25. | Westberg M, Grøgaard B, Snorrason F. Early prosthetic joint infections treated with debridement and implant retention: 38 primary hip arthroplasties prospectively recorded and followed for median 4 years. Acta Orthop. 2012;83:227-232. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 75] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 26. | Barberán J, Aguilar L, Carroquino G, Giménez MJ, Sánchez B, Martínez D, Prieto J. Conservative treatment of staphylococcal prosthetic joint infections in elderly patients. Am J Med. 2006;119:993.e7-993.10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 137] [Cited by in F6Publishing: 123] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 27. | Vilchez F, Martínez-Pastor JC, García-Ramiro S, Bori G, Maculé F, Sierra J, Font L, Mensa J, Soriano A. Outcome and predictors of treatment failure in early post-surgical prosthetic joint infections due to Staphylococcus aureus treated with debridement. Clin Microbiol Infect. 2011;17:439-444. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 105] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 28. | Aboltins CA, Page MA, Buising KL, Jenney AW, Daffy JR, Choong PF, Stanley PA. Treatment of staphylococcal prosthetic joint infections with debridement, prosthesis retention and oral rifampicin and fusidic acid. Clin Microbiol Infect. 2007;13:586-591. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 140] [Cited by in F6Publishing: 151] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 29. | Azzam KA, Seeley M, Ghanem E, Austin MS, Purtill JJ, Parvizi J. Irrigation and debridement in the management of prosthetic joint infection: traditional indications revisited. J Arthroplasty. 2010;25:1022-1027. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 164] [Cited by in F6Publishing: 167] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 30. | Brandt CM, Sistrunk WW, Duffy MC, Hanssen AD, Steckelberg JM, Ilstrup DM, Osmon DR. Staphylococcus aureus prosthetic joint infection treated with debridement and prosthesis retention. Clin Infect Dis. 1997;24:914-919. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 286] [Cited by in F6Publishing: 253] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 31. | Choi HR, von Knoch F, Kandil AO, Zurakowski D, Moore S, Malchau H. Retention treatment after periprosthetic total hip arthroplasty infection. Int Orthop. 2012;36:723-729. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 32. | Choong PF, Dowsey MM, Carr D, Daffy J, Stanley P. Risk factors associated with acute hip prosthetic joint infections and outcome of treatment with a rifampinbased regimen. Acta Orthop. 2007;78:755-765. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 108] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 33. | Konigsberg BS, Della Valle CJ, Ting NT, Qiu F, Sporer SM. Acute hematogenous infection following total hip and knee arthroplasty. J Arthroplasty. 2014;29:469-472. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 34. | Martínez-Pastor JC, Muñoz-Mahamud E, Vilchez F, García-Ramiro S, Bori G, Sierra J, Martínez JA, Font L, Mensa J, Soriano A. Outcome of acute prosthetic joint infections due to gram-negative bacilli treated with open debridement and retention of the prosthesis. Antimicrob Agents Chemother. 2009;53:4772-4777. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 113] [Cited by in F6Publishing: 120] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 35. | Meehan AM, Osmon DR, Duffy MC, Hanssen AD, Keating MR. Outcome of penicillin-susceptible streptococcal prosthetic joint infection treated with debridement and retention of the prosthesis. Clin Infect Dis. 2003;36:845-849. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 118] [Cited by in F6Publishing: 127] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 36. | Sukeik M, Patel S, Haddad FS. Aggressive early débridement for treatment of acutely infected cemented total hip arthroplasty. Clin Orthop Relat Res. 2012;470:3164-3170. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 58] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 37. | Estes CS, Beauchamp CP, Clarke HD, Spangehl MJ. A two-stage retention débridement protocol for acute periprosthetic joint infections. Clin Orthop Relat Res. 2010;468:2029-2038. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 38. | Rasouli MR, Tripathi MS, Kenyon R, Wetters N, Della Valle CJ, Parvizi J. Low rate of infection control in enterococcal periprosthetic joint infections. Clin Orthop Relat Res. 2012;470:2708-2716. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 39. | Klouche S, Leonard P, Zeller V, Lhotellier L, Graff W, Leclerc P, Mamoudy P, Sariali E. Infected total hip arthroplasty revision: one- or two-stage procedure? Orthop Traumatol Surg Res. 2012;98:144-150. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 88] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 40. | Buller LT, Sabry FY, Easton RW, Klika AK, Barsoum WK. The preoperative prediction of success following irrigation and debridement with polyethylene exchange for hip and knee prosthetic joint infections. J Arthroplasty. 2012;27:857-864.e1-4. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 103] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 41. | Koyonos L, Zmistowski B, Della Valle CJ, Parvizi J. Infection control rate of irrigation and débridement for periprosthetic joint infection. Clin Orthop Relat Res. 2011;469:3043-3048. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 145] [Cited by in F6Publishing: 157] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 42. | Kuiper JW, Vos SJ, Saouti R, Vergroesen DA, Graat HC, Debets-Ossenkopp YJ, Peters EJ, Nolte PA. Prosthetic joint-associated infections treated with DAIR (debridement, antibiotics, irrigation, and retention): analysis of risk factors and local antibiotic carriers in 91 patients. Acta Orthop. 2013;84:380-386. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 119] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 43. | Fehring TK, Odum SM, Berend KR, Jiranek WA, Parvizi J, Bozic KJ, Della Valle CJ, Gioe TJ. Failure of irrigation and débridement for early postoperative periprosthetic infection. Clin Orthop Relat Res. 2013;471:250-257. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 135] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 44. | Crockarell JR, Hanssen AD, Osmon DR, Morrey BF. Treatment of infection with débridement and retention of the components following hip arthroplasty. J Bone Joint Surg Am. 1998;80:1306-1313. [PubMed] [Cited in This Article: ] |
| 45. | Geurts JA, Janssen DM, Kessels AG, Walenkamp GH. Good results in postoperative and hematogenous deep infections of 89 stable total hip and knee replacements with retention of prosthesis and local antibiotics. Acta Orthop. 2013;84:509-516. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 46. | Engesæter LB, Dale H, Schrama JC, Hallan G, Lie SA. Surgical procedures in the treatment of 784 infected THAs reported to the Norwegian Arthroplasty Register. Acta Orthop. 2011;82:530-537. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 86] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 47. | Triantafyllopoulos GK, Poultsides LA, Zhang W, Sculco PK, Ma Y, Sculco TP. Periprosthetic knee infections treated with irrigation and debridement: outcomes and preoperative predictive factors. J Arthroplasty. 2015;30:649-657. [PubMed] [Cited in This Article: ] |
| 48. | Cierny G, DiPasquale D. Periprosthetic total joint infections: staging, treatment, and outcomes. Clin Orthop Relat Res. 2002;23-28. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 74] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 49. | Burger RR, Basch T, Hopson CN. Implant salvage in infected total knee arthroplasty. Clin Orthop Relat Res. 1991;105-112. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 38] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 50. | Gardner J, Gioe TJ, Tatman P. Can this prosthesis be saved?: implant salvage attempts in infected primary TKA. Clin Orthop Relat Res. 2011;469:970-976. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 118] [Cited by in F6Publishing: 125] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 51. | Chiu FY, Chen CM. Surgical débridement and parenteral antibiotics in infected revision total knee arthroplasty. Clin Orthop Relat Res. 2007;461:130-135. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 59] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 52. | Bradbury T, Fehring TK, Taunton M, Hanssen A, Azzam K, Parvizi J, Odum SM. The fate of acute methicillin-resistant Staphylococcus aureus periprosthetic knee infections treated by open debridement and retention of components. J Arthroplasty. 2009;24:101-104. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 163] [Cited by in F6Publishing: 171] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 53. | Mont MA, Waldman B, Banerjee C, Pacheco IH, Hungerford DS. Multiple irrigation, debridement, and retention of components in infected total knee arthroplasty. J Arthroplasty. 1997;12:426-433. [PubMed] [Cited in This Article: ] |
| 54. | Teeny SM, Dorr L, Murata G, Conaty P. Treatment of infected total knee arthroplasty. Irrigation and debridement versus two-stage reimplantation. J Arthroplasty. 1990;5:35-39. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 119] [Cited by in F6Publishing: 115] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 55. | Segawa H, Tsukayama DT, Kyle RF, Becker DA, Gustilo RB. Infection after total knee arthroplasty. A retrospective study of the treatment of eighty-one infections. J Bone Joint Surg Am. 1999;81:1434-1445. [PubMed] [Cited in This Article: ] |
| 56. | Marculescu CE, Berbari EF, Hanssen AD, Steckelberg JM, Harmsen SW, Mandrekar JN, Osmon DR. Outcome of prosthetic joint infections treated with debridement and retention of components. Clin Infect Dis. 2006;42:471-478. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 347] [Cited by in F6Publishing: 344] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 57. | Tattevin P, Crémieux AC, Pottier P, Huten D, Carbon C. Prosthetic joint infection: when can prosthesis salvage be considered? Clin Infect Dis. 1999;29:292-295. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 179] [Cited by in F6Publishing: 193] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 58. | Li M, Diep BA, Villaruz AE, Braughton KR, Jiang X, DeLeo FR, Chambers HF, Lu Y, Otto M. Evolution of virulence in epidemic community-associated methicillin-resistant Staphylococcus aureus. Proc Natl Acad Sci USA. 2009;106:5883-5888. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 302] [Cited by in F6Publishing: 309] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 59. | Martel-Laferrière V, Laflamme P, Ghannoum M, Fernandes J, Di Iorio D, Lavergne V. Treatment of prosthetic joint infections: validation of a surgical algorithm and proposal of a simplified alternative. J Arthroplasty. 2013;28:395-400. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 60. | Peel TN, Buising KL, Dowsey MM, Aboltins CA, Daffy JR, Stanley PA, Choong PF. Outcome of debridement and retention in prosthetic joint infections by methicillin-resistant staphylococci, with special reference to rifampin and fusidic acid combination therapy. Antimicrob Agents Chemother. 2013;57:350-355. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 67] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 61. | Van Kleunen JP, Knox D, Garino JP, Lee GC. Irrigation and débridement and prosthesis retention for treating acute periprosthetic infections. Clin Orthop Relat Res. 2010;468:2024-2028. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 62. | Triantafyllopoulos G, Poultsides LA, Zhang W, Sculco PK, Ma Y, Sculco TP. Multiple Irrigation and Debridements for Periprosthetic Joint Infections: Facing a Necessity or Just Prolonging the Inevitable? J Arthroplasty. 2016;31:219-224. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 63. | Klouche S, Lhotellier L, Mamoudy P. Infected total hip arthroplasty treated by an irrigation-debridement/component retention protocol. A prospective study in a 12-case series with minimum 2 years’ follow-up. Orthop Traumatol Surg Res. 2011;97:134-138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |