Published online Dec 18, 2017. doi: 10.5312/wjo.v8.i12.935
Peer-review started: September 21, 2017
First decision: October 23, 2017
Revised: November 1, 2017
Accepted: December 3, 2017
Article in press: December 3, 2017
Published online: December 18, 2017
To evaluate our modified deepening trochleoplasty combined with a balanced medial patellofemoral ligament (MPFL) reconstruction for soft tissue alignement.
Thirty-three knees with with recurrent patellar dislocations and a trochlear dysplasia in 30 patients (m/f = 12/21, mean age 24 ± 9 years) underwent a combination of a modified deepening trochleoplasty and a balanced MPFL reconstruction for a medial soft tissue alignement. After a mean follow-up period of 29 ± 23 mo, patients’ return to sports, possible complications as well as the clinical outcomes using the Kujala, International Knee Documentation Committee (IKDC) and Lysholm scoring were evaluated. Moreover, patients’ satisfaction with the general outcome, the cosmetic outcome, the pre- and postoperative pain and a potential avoidance behaviour were assessed with additional standardized questionnaires which also included different visual analog scales.
There were no signs of a persistent instability. The Kujala score improved from a mean of 64 ± 16 points to 94 ± 9 points, the Lysholm score improved from a mean of 63 ± 17 to 95 ± 6 points and the IKDC score from 58 ± 11 to 85 ± 12 points, P < 0.0001, respectively. The assessment of pain using a visual analog scale showed a significant pain reduction from a mean of 4.8 ± 2.0 to 1.3 ± 3.4 points (P < 0.0001). Two of 26 cases (92%) who were engaged in regular physical activity before surgery did not return to full sporting activities. One patient felt that his sport was too risky for his knee and reported an ongoing avoidance behaviour. The other patient preferred to wait for surgery of her contralateral knee. Of the eight patients who were not engaged in sporting activities before surgery, three started regular sporting activities after surgery. In 31 of the 33 cases (94%), the patients were very satisfied with the clinical outcome of the surgery. Regarding the cosmetic results, no patients felt impaired in their self-confidence and in their clothing decisions.
Our technique shows a good clinical outcome in terms of the common scorings as well as in terms of pain, return to sports and patient satisfaction.
Core tip: Patients with recurrent patella dislocations typically have an insufficiency of the medial patellofemoral ligament (MPFL), which is an additional instability factor in a symptomatic trochlear dysplasia. Following a trochleoplasty, the articulation of the patella is changed to a more medial and dorsal mechanical position. As a consequence, a balanced alignment of the medial soft tissue restraints during a trochleoplasty is very reasonable to achieve an adequate stabilization. The combination of a modified Bereiter trochleoplasty and our MPFL reconstruction technique allowing a simple intra-operative tensioning shows encouraging results.
- Citation: von Engelhardt LV, Weskamp P, Lahner M, Spahn G, Jerosch J. Deepening trochleoplasty combined with balanced medial patellofemoral ligament reconstruction for an adequate graft tensioning. World J Orthop 2017; 8(12): 935-945
- URL: https://www.wjgnet.com/2218-5836/full/v8/i12/935.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i12.935
In flexion angles of more than 30°, the patella is predominantly guided by the trochlear groove. Between 30° of flexion and the full extension, both the medial patellofemoral ligament (MPFL) and the trochlear groove stabilize the patella[1,2]. In trochlear dysplasia, the trochlea is shallow, flat, or dome shaped, leading to an inadequate resistance to lateral patellar dislocations. Therefore, it has been described to be a major risk factor for patellofemoral instability[3]. Trochlear dysplasia is described in less than 2% of the population, whereas it occurs in up to 85% of patients with patellar instability[4]. An isolated MPFL reattachment or reconstruction in the presence of a severe dysplasia of the trochlea shows a relatively poor clinical outcome and leads to an increased risk for a recurrent instability with persistent apprehension and/or dislocations[5-10]. Therefore, a severe dysplasia of the trochlea should be addressed when corresponding clinical findings are present.
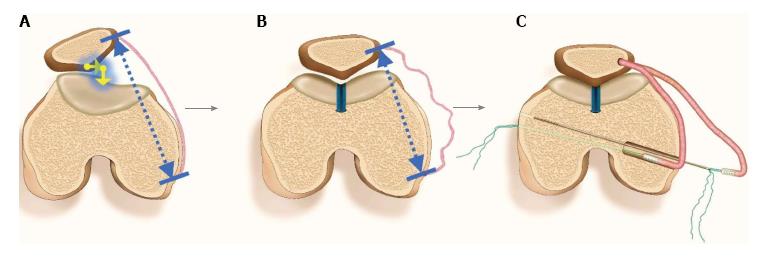
Following an acute patellar dislocation, the MPFL is ruptured with a frequency of more than 90%, which can cause recurrent dislocations and/or a significant instability[1,11,12]. During a trochleoplasty, the intra-operative impression that the patella is moved to a more medial and dorsal mechanical position has been proven by a computed tomography (CT) study on corrective postoperative changes[13]. As a logical consequence, a MPFL plastic surgery seems advisable, not only to address a torn, insufficient ligament, but also because a balancing and alignment of the medial soft tissue restraints is necessary (Figure 1). Therefore, our technique of a MPFL reconstruction allowing a simple intra-operative testing and adjustment of the graft tension[14], might be convenient especially in cases with a combined trochleoplasty. This might help in minimizing common complications of MPFL reconstructions, such as an overtensioning with anterior knee pain and/or motion deficits, patellar fractures, etc. or an undertensioning with an ongoing instability[6,15,16]. This study was necessary to explore our combination of a deepening trochleoplasty and our technique of a balanced MPFL reconstruction for a medial soft tissue alignment. Our hypothesis is that this technique provides reasonable advantages.
This study has been approved by the Ethical Committee of the University of Witten/Herdecke (Study No. 108/2015) and was carried out in accordance with the ethical standards laid down in the Declaration of Helsinki. The participation was voluntary and all patients gave their informed consent to this study.
This study includes 33 knees with a severe trochlear dysplasia in 30 patients (m/f = 12/21, mean age 24 ± 9 years) who underwent surgery with a combination of trochleoplasty and MPFL reconstruction as described below. The estimated mean number of dislocations before surgery was 35 ± 24 (range: 1-250). Before surgery, all patients had a clear positive patella apprehension sign. Exclusion criteria were additional surgeries such as corrections of the knee rotation and/or axis, tibial tuberosity transfers, etc. Moreover, patients with advanced osteoarthritic changes or previous fractures of the knee were not included in this study. Factors of patellar instability were measured on preoperative radiographs and magnetic resonance imagings (MRIs) or CT scans[4]. In our series, the mean Caton-Deschamps index was 1.09 ± 0.09 and the tibial tubercle-trochlear groove distance was 16 mm ± 3 mm. The lateral trochlea inclination (LTI) angle was measured on the most superior MRI slice depicting the cartilage of the trochlear surface using the method described by Carrillon et al[17]. In our patients, the mean angle between the posterior contours of the condyles and the lateral facet of the trochlear groove was -9° ± 6°. Trochlear dysplasia was graded using the Dejour classification. Nine knees showed a type B, ten a type C and 14 a type D trochlear dysplasia.
The mean follow-up period was 29 ± 23 mo. Possible complications such as recurrent dislocations, fractures, knee stiffness, etc. were registered. In addition to a routinely performed clinical examination, the knee function was assessed with different scoring scales. In this study, the Kujala anterior knee pain scoring, the knee-specific outcome measure of the International Knee Documentation Committee (IKDC) and the Lysholm knee scale was used. Moreover, additional questionnaires and different visual analog scales were used to assess the general satisfaction of the patients, the satisfaction with the cosmetic outcome, the return to sports, a potential avoidance behaviour, different sports activities as well as a potential anterior knee pain.
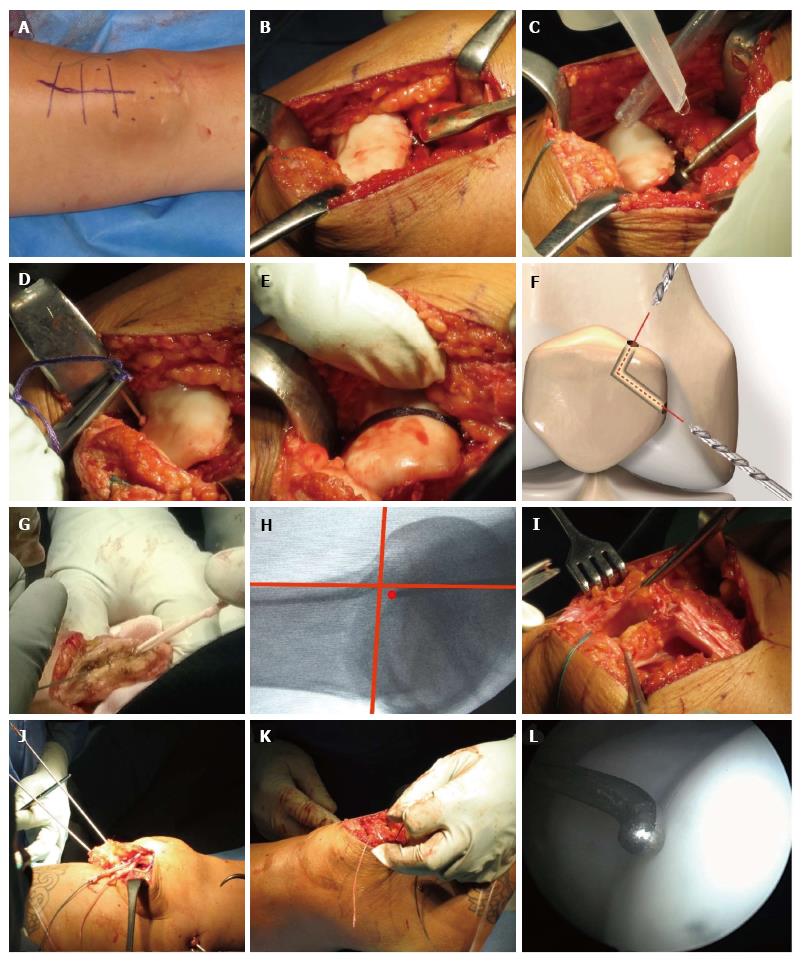
The gracilis tendon is harvested through a minimal invasive posterior or anterior harvest over the pes anserinus. After whip-stitching the armed graft has been given in a Vancomycin solution for presoaking in most cases. In contrast to the Bereiter technique, which describes a lateral parapatellar approach, we prefer a short medial parapatellar access to expose the trochlea. A seven to 10 cm long skin incision running from the medial part of the patella to the distal part of the quadriceps tendon is made (Figure 2A). The medial patellar retinaculum is divided by leaving enough tissue near the patella for later reattachment. The proximal joint capsule is incised between the superomedial pole of the patella and the vastus medialis obliquus muscle. Finally, the distal quadriceps tendon is split. Using this distally shortened medial parapatellar approach, the saphenous nerve with its infrapatellar branch is usually not affected. With this simple arthrotomy and a dislocation of the patella towards lateral, the trochlea can be completely exposed (Figure 2B). A soft tissue tunnel between both layers and running down from medial patella to the femoral MPFL insertion can be created easily by using this approach. After exposure of the trochlea, the articular cartilage is separated from the synovium. Using a curved osteotome, a thin osteochondral flap, leaving 2 mm of subchondral bone, is very carefully chiselled off the medial and lateral trochlea (Figure 2B). The flap is extended down to the intercondylar notch. The trochlear bone is then deepened using chisels and a high-speed diamond burr (Figure 2C). The lateral edge of the trochlea is not lowered to obtain a raised lateral inclination angle with an effective bony stabilization. This way, a recentralized groove is created. In cases with an increased TT-TG distance, the groove can also be deepened in a lateralized position. Then, the thin and flexible osteochondral flap is pressed into the newly formed groove. When the flap is not flexible enough, it should be thinned with the high-speed burr. The osteochondral flap is fixed into the new formed groove with a transosseous resorbable 3 mm Vicryl band (Ethicon Products, Norderstedt, Germany). For this step, the Vicryl band is passed from the distal start of the formed groove, which is usually a couple of millimeters above the intercondylar notch, through the femoral condyle using a big and eyed curved needle (Figure 2D). A second, proximal transosseous passage through the femoral condyle is performed starting exactly at the proximal end of the new groove. After pressing the flap onto the femoral bone, the Vicryl band is tightened and fastened (Figure 2E). If needed, a second Vicryl band, running from the distal part of the sulcus to the craniolateral edge of the trochlea, can be used to press the flap more firmly to the bone. After preparation of the medial patella facet and a debridement of the bone between both layers, two guide wires, coming from the middle of the medial edge of the patella and the superomedial pole, are advanced into the bone. Using a 4.5 mm cannulated drill bit, a V-shaped tunnel with an angulation of around 120° is created. The drillings should run as vertically as possible and leave a bone bridge between both ends of at least 15 mm (Figure 2F). The starting points of both patellar tunnels may correspond to a recent anatomic study on the MPFL, where the attachment spreads out along the upper and middle third of the medial patella edge[18]. Using a curved needle, the graft is passed through the tunnel (Figure 2G). After palpation of the bony femoral MPFL insertion, the origin is marked with a K wire under fluoroscopic guidance. As described by Schöttle et al[19], the radiographic landmark of the femoral attachment is located 2.5 mm distal to the posterior origin of the femoral condyle and 1.3 mm anterior to a line at the posterior cortical bone of the femur (Figure 2H). After a stab incision, the guide wire is advanced to the opposite cortical bone of the femur and overreamed to a depth of at least 4 cm. Then the medial capsule is exposed and a soft tissue tunnel between both layers of the capsule is extended down to the femoral insertion of the MPFL graft (Figure 2I). Two beath pins are introduced into the femoral bone tunnel. From the end of this blind-ending tunnel, both pins are advanced in divergent directions and passed through the lateral cortical bone of the femur (Figure 2J). Using the prepared soft tissue tunnel between both layers of the medial capsule, both armed ends of the graft loop are shuttled from the patella down to the femoral bone tunnel. Each strand of the whipstitch sutures at both ends of the graft is passed through the eyelets of the beath pins. By passing the pins through the femur, the ends of the whipstitch sutures are passed through the lateral femoral cortex. By pulling on each suture pair, both armed ends of graft are introduced into the tunnel (Figure 2K). On the lateral femur, a temporary knot is tied down to the lateral femoral cortex in approximately 30° knee flexion. This knot is temporarily fastened with a needle driver or by hand. The tension of the MPFL graft and the achieved motion of the patella is assessed by knee flexion and lateral translation of the patella. If necessary, the tension of the double limbed graft can be adjusted and functionally tested again. Finally, the knot is permanently tied up by using a series of half hitches. The inner layer of the capsule underneath the graft and the thicker superior layer which lies above the graft are closed separately and right up to both layers at the patellar margin (Figure 2G and I). The tendon of the vastus medialis obliquus muscle can be tightened medially to the patella if needed. Finally, the longitudinal incision within the distal part of the quadriceps tendon is closed up.
In the first two post-operative weeks, a partial load was recommended. In the first six weeks, an adjustable knee brace was prescribed. During the first two weeks, the motion was restricted to a knee flexion between 0° and 30°. During the third and fourth weeks, the flexion was limited to 60° and to 90° within the fifth and sixth weeks. In this context, we have to amend that we do not recommend these limitations any more (please see discussion). A rehabilitation of 12 wk was recommended before starting with sporting activities.
The statistical analyses in this study were done by using the SPSS statistics 22.0 software (SPSS Inc, Chicago, IL, United States). A statistical review of the study was performed by a biomedical statistician. The Wilcoxon signed-rank test was used to compare the pre- and postoperative clinical scores. For the comparison of the scoring between different groups within this study we used the Mann-Whitney-U test.
No patients showed signs of a persistent instability. Thus, persistent postoperative instabilities from subtle instability with anamnestic subluxations to frank dislocations were not reported. The apprehension tests were negative in all patients. Two patients reported a persistent avoidance behavior. Even if they had already mastered typical stress situations with experienced luxations in the past, they continued a slight avoidance behavior. Both patients reported that this behaviour was caused psychologically and not instability- and/or pain-related. All other patients reported being able to fully load their knee without anxiety.
In 31 of the 33 cases (94%) the patients were very satisfied with the clinical outcome of the surgery. All of them would again decide for the same procedure. Two patients (6%) were dissatisfied. Both patients had a flexion deficit between 20° and 30°. One of these patients also reported an anterior knee pain. However, the main reason for her disappointment was that she was not able to play and to crawl an all fours with her toddler.
Regarding the cosmetic outcome, all patients were satisfied with the outcome. Thus, no patients felt impaired in their self-confidence and/or in their clothing choices such as skirts or trousers. Two patients were only partially satisfied because they would have preferred a shorter and narrower scar. On the other hand, they would not decide for an aesthetic correction operation assuming that this would be most likely successful.
Four patients (12%) reported no changes of their pain symptoms, which could be described in all of these cases as a slight anterior knee pain occurring occasional during exercise and/or longer runs. A further four patients (12%) reported an increase of pain at the last follow-up. Further six patients (18%) reported a severe knee pain before surgery which improved almost completely at the last follow-up. Further 14 patients (42%), who mainly showed severe pain symptoms before surgery, became completely pain-free. Further five patients (15%) had no knee pain before surgery as well as at the last follow-up. Taken together, in 29 of 33 cases (89%), the patients either remained unchanged with mild symptoms or no pain, or showed a notable improvement to an almost or completely pain-free situation. The assessment of pain using a visual analog scale showed a significant pain reduction from a mean of 4.8 ± 2.0 to 1.3 ± 3.4 points (P < 0.0001).
In 25 of the 33 cases, patients were engaged in regular physical activity before surgery. After surgery, two of these did not return to full sporting activities. Both did not have any complaints. One patient reported an anxiety or avoidance behaviour for typical stress situations as a reason for not returning to his full sporting activities. He played soccer and he felt that this sport is too strenuous or risky for his knee. The other patient preferred to wait for the surgery of her contralateral knee. Of the eight patients who were not engaged in sporting activities before surgery, three moved to the group of patients engaging in regular physical activity. The remaining five patients were very satisfied with their knee function during daily activities and none of them reported any complaints or recurrent luxations. Nevertheless, four of them still had no interest in sporting activities. One of the five patients who remained uninvolved in sports reported a continuing avoidance behavior in her daily activities. Although she had already mastered typical stress situations with previously experienced dislocations, she reported persistent avoidance behavior.
No deep infection or wound infection occurred. Recurrent dislocations, patella fractures, breakages of the osteochondral flap during surgery etc, were not registered. The re-operation rate in our study was 6% (2/33). In both cases, an early postoperative motion deficit with a markedly reduced flexion between 70° and 90° was treated. After the hospital stay, both patients did not attend the recommended physiotherapy. In both cases, arthroscopy with an arthrolysis and a mobilization was performed around three months after the initial surgery. During arthroscopy, adhesions within the joint were removed. Arthroscopy of the trochlear groove and the cartilage of the patellofemoral joint showed regular findings, the vicryl fiber was fully resorbed (Figure 2L). Subsequently, both patients had better motion and decreased pain during motion. At the final follow-up, they showed an unlimited motion and no anterior knee pain. Furthermore, we have to report three patients with a slight flexion deficit at the last follow-up. Two showed a deficit of around 20°. Both patients reported a slight anterior knee pain occurring after prolonged load during physical exercise such as longer runs, etc. A persistent and/or severe anterior knee pain was denied. The third patient showed a flexion deficit of 35° compared to the contralateral side. He was pain-free.
As depicted, the Kujala score improved significantly from a mean of 64 ± 16 points preoperatively to 94 ± 9 points postoperatively (P < 0.0001). The Lysholm score improved significantly from a mean of 63 ± 17 to 95 ± 6 points and the IKDC score from 58 ± 11 to 85 ± 12 points, P < 0.0001, respectively. There were no significant differences regarding age, sex, BMI and affected side of the knee (P > 0.05).
Different deepening trochleoplasty techniques are currently performed in a symptomatic dysplasia[20]. Dejour et al[21] describes an osteotomy and bone removal at both femoral condyles to create a V-shaped trochlear groove. Both trochlear fragments are refixed with metallic staples. Goutallier et al[22,23] described the recession trochleoplasty, where the trochlear bump is settled into a deeper position after the removal of a wedge at the lateral femoral condyle. The Bereiter et al[24]’s technique describes a lateral parapatellar approach to raise an osteochondral flap from the anterior aspect of the femur. After remodeling the trochlear groove, the flap is seated and pressed into the deepened trochlea. A histological follow-up study reported no further cartilaginous damage or degeneration for this “thin flap technique”[25]. This corresponds to our findings of an intact and stable cartilage in two patients who underwent an arthroscopic arthrolysis (Figure 2L). All authors who use the Bereiter trochleoplasty describe a lateral parapatellar approach[26-32]. In contrast, the Dejours’ Lyons’ procedure uses a modified midvastus approach with a dissection of the vastus medialis muscle fibers extending around 4 cm into the muscle belly[21]. As described above, we routinely use a shortened medial parapatellar approach (Figure 2A). This approach provides a good exposure of the medial edge of the patella to create our bony tunnel for the graft loop (Figure 2G). Furthermore, it provides a good access to the medial capsule for the preparation of a soft tissue tunnel between both layers going down to the femoral insertion of the MPFL graft (Figure 2I). An extensive skin mobilization or a further skin incision to expose the medial edge of the patella is not needed for the MPFL reconstruction. Moreover, we feel that this approach provides a much easier access to the trochlear groove (Figure 2B). After the closure of both capsular layers, the tendon of the vastus medialis obliquus muscle can be tightened medially to the patella if needed. Taken together, this medial parapatellar approach might have several advantages.
Even if MPFL reconstruction is a proven method, an optimized tensioning of the graft should not be taken for granted. Regarding the literature, an excessive graft tension is one of the most common complications during MPFL reconstruction[10,33]. This might lead to stiffness, pain, cartilage degradation, arthrosis and patella fractures[10,33,34]. Thus, techniques which provide an adequate tensioning might help to achieve a sufficient stabilization with a minimized risk of an overtightened graft. Regarding the literature, a variety of techniques are described to get an appropriate amount of graft tension. Thaunat and Erasmus[35] recommend a full extension and the use of a hook to pull the patella proximal to avoid an overtensioning. Feller et al[36] tension the graft with one quadrant of lateral translation in knee extension, then the knee is flexed to 20° for permanent fixation. Other authors prefer techniques with the use of 30° of knee flexion for graft fixation[8,26,28] and some prefer a position between 60° and 90° of flexion because this might allow a more precise settling of the patella within the deeper, more inferior parts of the trochlear groove[37]. Therefore, finding the most appropriate technique for graft fixation seems quite confusing. Furthermore, there is currently no consensus on the question of how many degrees the knee should be flexed when the graft is secured to its insertion points. Therefore, our technique to simply test and balance the tension during knee motion before permanent fixation might be a feasible and satisfying solution. Considering that 30° of knee flexion seems to be recommended most frequently in the literature[8,26,28], we begin with a temporary graft fixation at 30° of flexion. Only after testing and balancing the tension is the graft permanently fastened[14]. Because our technique uses nearly the entire length of the gracilis tendon with a loop through the patella, this construct appears less rigid (Figure 1C). This might additionally reduce the risk of an overloading. Besides the advantage to reach a balanced and less rigid construct, the avoidance of hardware such as screws and/or anchors might be another benefit of our technique. This does not only save money, it also reduces possible implant specific complications such as an implant loosening and/or discomfort with the anchoring material[6,16,28].
An important finding of the present study is that the combination of a modified Bereiter trochleoplasty and our hardware-free, balanced MPFL reconstruction technique, provides a sufficient and reliable stabilization of the patellofemoral joint. Thus, the apprehension tests were negative in all cases and no subluxations or recurrent dislocations were reported at the last follow-up. This is in accordance to a recent systematic review, where the overall rate of recurrent dislocations after different trochleoplasty techniques was 2%[20]. The highest rate for recurrent dislocations was reported for the recession type trochleoplasty (10.5%), followed by the Dejour (3.2%) and Bereiter (0.8%) techniques[20]. Interestingly, all studies on the combination of a Bereiter trochleoplasty and a MPFL reconstruction describe a 0% rate for recurrent dislocations[26,28,38]. Regarding a residual apprehensiveness, studies on a Bereiter or Dejour throcheloplasty without a routinely added MPFL reconstruction might be of interest. These studies reported a residual apprehensiveness in 16%[39], 20%[31], 21%[32] and 47%[40] of cases. In contrast, in studies where a MPFL reconstruction was routinely performed in combination with a trochleoplasty, the apprehension sign was eliminated in all patients[26,28,38]. These data imply that a MPFL reconstruction seems to be a useful addition to a trochleoplasty. Regarding the clinical outcome, studies on trochleoplasties which were routinely combined with a MPFL reconstruction demonstrate similar postoperative Kujala scores of 96[26], 88[28] and 95[38] points, respectively. In comparison, studies on trochleoplasties which were not routinely combined with a MPFL reconstruction showed Kujala scores of 76[31], 80[32], 75[40] and 71 points[27], respectively. At this point, we would like to mention that we did not consider all studies with different types of trochleoplasty techniques, soft tissue procedures, additional procedures, etc. Rather, we aim to highlight possible tendencies. Thus, differences that are apparent at first sight might not be substantial or at least statistically significant. However, the superior results of a combined surgery in terms of a persisting apprehensiveness, recurrent dislocations, as well as in terms of the clinical outcome scoring can also be explained by the pathophysiology of the patient cohort. Thus, in more than 90% of cases, a dislocation of the patella results in a traumatic disruption and insufficiency of the MPFL[1,11,12]. Moreover, a trochleoplasty changes the articulation of the patella to a more medial and dorsal biomechanical position (Figure 1A). These changes, measuring at least 5 mm in each direction, have been nicely shown in this series with pre- and postoperative CT scans after a Bereiter trochleoplasty[13]. This might lead to a reduced distance between the femoral and patellar insertions of the medial soft tissue restraints (Figure 1B). Thus, a preexisting insufficiency of the MPFL might be aggravated by the biomechanical changes following a trochleoplasty. As a consequence, a balanced alignment of the medial soft tissue restraints, such as an adequately tensioned MPFL reconstruction (Figure 1C), seems very reasonable during a trochleoplasty.
Another additional surgery, which is not so rarely combined with a trochleoplasty, is a tibial tuberosity transfer to reduce an elevated TT-TG as a further instability factor [27,40-42]. During a trochleoplasty we normally prefer to deepen and set the created trochlear groove more laterally to tendentially correct an asymmetry of the trochlear facets (Figure 1A and B). This possibility to address an elevated TT-TG distance has already been described by several authors for both the Dejour and the Bereiter technique[29,41,42]. Fucentese et al[13] demonstrated a case series with pre- and postoperative CT scans showing a successful lateralized trochlear groove after trochleoplasty. This possibility might influence the decision to perform an additional medialization osteotomy of the tuberosity. Considering this, we perform this additional procedure only in cases with an excessive TT-TG distance.
Showing an overall rate of 6.7%, a significant motion deficit is the second most common complication in trochleoplasty procedures[20]. In our series, at the last follow-up, three patients (9.1%) showed a slight flexion deficit compared to the contralateral side. Two had a deficit of 20° and one patient had a deficit of 30°. In regard to these data, we reconsidered our rehabilitation protocol, which limited the flexion to 30° for the first two weeks, to 60° in the third and fourth weeks and to 90° in the fifth and sixth weeks. The rationale behind these limitations was to avoid a shearing of the osteochondral flap. Reviewing the literature, we had to recognize that the majority of authors are much more progressive. Thus, most of them use protocols without a postoperative flexion limitation[26,27,30,31,38,40]. Other authors limit the flexion to 100°[21], 90°[28] or 60°[23,29]. Interestingly, some authors recommend a 20° or 30° block to full extension[30,31,38]. The idea of this protocol is to centralize the patella within the remodeled groove and to facilitate a healing of the trochlear osteotomy[30]. However, considering our results we do not use or recommend the protocol previously described in the methods section any more. Currently, we do not limit the flexion after trochleoplasty. Moreover, the two patients who needed an early arthroscopic arthrolysis as a result of a failed physiotherapy emphasize the importance of motion exercises. Therefore, physiotherapy including a continuous passive motion (CPM) is performed immediately after surgery. Moreover, each patient receives a knee CPM machine as a loan for at least four weeks after surgery. Regarding the return to sports rates, we had two patients who did not return to full sporting activities. One of these was in the group which was engaged in sports before surgery, the other patient did not in participate in regular physical activity before surgery. Neither patient had complaints or an ongoing instability. However, even if they had already mastered situations with experienced luxations in the past, both reported an ongoing anxiety for typical stress situations. Both reported that this behavior was psychologically caused and not instability- and/or pain-related. Thus, despite a sufficient stabilization, an unlearning process of such an acquired avoidance behavior should not be taken for granted. This study result is important to us because it highlights the need for a prolonged postoperative physiotherapy according to the individual need of the patient. This might minimize the reported avoidance behaviour.
The major limitations of this study are the short mean follow-up of 29 mo and the lack of a direct comparison to other surgical techniques. A larger clinical outcome study is needed to ensure the efficacy of our method. Therefore, the outcome results should be regarded cautiously. Being able to present only short-term results, data on the prevention of a secondary arthritis are lacking. However, the study presented here was a necessary first step in exploring our modified method, which seems to provide reasonable advantages. The preliminary clinical results demonstrate a good efficiency in relieving the symptoms and improving the function of the affected knee.
Our modified technique shows encouraging results in terms of a sufficient stabilization of the patellofemoral joint, a low incidence of complications and a good outcome in terms of pain, cosmetic results and return to sports. In accordance to these results, a significant improvement in all evaluated scores was achieved and a high patient satisfaction was demonstrated. These findings correlate with the literature on similar techniques, which combine a trochleoplasty with an alignment of the medial soft tissue restraints. Nevertheless, the good outcome in our case series and in previous studies should not be taken for granted. The need for an individual postoperative physio- and sports therapy is also outlined in this study.
Trochlear dysplasia is an important and frequent instability factor in patients with recurrent patella dislocations. These patients typically have an insufficiency of the medial patellofemoral ligament (MPFL), which is an additional instability factor. During a trochleoplasty, the articulation of the patella is changed to a more dorsomedial position, which might worsen the insufficiency of the medial soft tissue restraints. All these patho-biomechanical conditions are relevant for a symptomatic instability and should therefore be addressed during surgery. Despite its relevance, studies on combined concepts to address all pathological conditions are rare.
Regardless of whether a MPFL reconstruction is performed as an isolated surgery or as in combination with a trochleoplasty, an adequate tensioning of the graft is a key problem during these surgical procedures. Thus, an overtensioning might lead to stiffness, pain, cartilage degradation, arthrosis and patella fractures, whereas an undertensioning leads to persistent instability complaints. Authors’ technique, which provides an adequate graft tensioning, appears to be helpful to solve these problems. Thus, the study presented here was a necessary first step in exploring authors’ method, which seems to provide reasonable advantages.
To realize a combination of authors’ technique of a balanced MPFL reconstruction to the bony alignment procedure, authors modified both, the technique and especially the approach of the Bereiter trochleoplasty as well as authors’ recently published technique of a balanced MPFL reconstruction. To evaluate authors’ method, 33 knees with with recurrent patellar dislocations and a trochlear dysplasia were evaluated after a mean follow-up of 29 mo.
To assess the outcome of authors’ modified technique, the Kujala, IKDC and Lysholm scoring were evaluated. Moreover, patients’ satisfaction with the general outcome, the return to sports, the cosmetic outcome, the pre- and postoperative pain and a potential avoidance behaviour were assessed.
The preliminary clinical results of this technique demonstrate a good efficiency in relieving the symptoms and improving the function of the affected knee. There were no signs of a persistent instability. A significant pain reduction and a significant improvement at the Kujala, Lysholm and IKDC scoring is demonstrated. 94% of the patients were very satisfied with the clinical and cosmetic outcome of the surgery. 92% of the patients who were engaged in regular physical activity before surgery returned to full sporting activities. In regard to three patients showing a slight flexion deficit compared to the contralateral side at the last follow-up, authors changed the postoperative treatment protocol. Thus, authors do not limit the flexion any more post-operatively and authors try to ensure intensive motion exercises. One patient did not return to sports and another patient, who was not active in sports before surgery, still did not participate in regular physical activity after surgery. Both reported that this was related to a persistent avoidance behavior and not instability- and/or pain-related. This specific problem, which reduced authors’ return to sports rate, might highlight the need for an intensive individual sports therapy.
In patients with a symptomatic patellar instability, both a trochlear dysplasia and an insufficiency of the MPFL should be addressed during surgery. Regarding the literature, an inadequate graft tensioning is one of the most important reasons for complications during MPFL reconstruction such as stiffness, pain, cartilage degradation, arthrosis, patella fractures, etc. Therefore, authors’ balanced MPFL reconstruction technique might optimize the alignment of the medial soft tissue restraints with a correspondingly low incidence of complications. The authors technique is a practicable solution to achieve a feasible correction of the bony dysplasia combined with a balanced alignment of the medial soft tissue restraints. Thus, authors’ technique shows a reliable stabilization of the patellofemoral joint and a low incidence of complications. The results in common clinical outcome scorings as well as in terms of pain, return to sports and patient satisfaction are encouraging. To realize a simple combination of authors’ recently published techniques of a balanced MPFL reconstruction with sulcus deepening trocheloplasty, authors modified both techniques. Especially the described approach to the medial margin of the patella, the medial retinaculum and to the trochlear groove appears very feasible. On the one hand, the study presented here was a necessary first step in exploring authors’ modified method, which seems to provide reasonable advantages. On the other hand, this study gives an original insight to the patients‘ outcome. Besides the assessment of the commonly used scorings and the incidence of complications, this investigation gives a deeper insight to understand the outcome in terms of pain, cosmetic results, patient satisfaction and the return to sports. This might give us a better understanding of the patients‘ expectations and the role of physio- as well as an individual sports therapy. Because both trochlear dysplasia and an insufficiency of the medial soft tissue restraints are relevant for a symptomatic patellar instability, a method which addresses both patho-biomechanical conditions might be a good solution. A balanced medial soft tissue reconstruction might optimize the procedure. To combine authors’ technique of a balanced MPFL reconstruction to the bony alignment procedure, authors modified both the technique and especially the approach of the Bereiter trochleoplasty as well as authors’ MPFL reconstruction technique. Authors’ balanced MPFL reconstruction technique might help to get an adequate alignment of the medial soft tissue restraints. Besides the assessment of the commonly used outcome scorings, this study gives a better understanding of the outcome in terms of pain, cosmetic results, patient satisfaction and the return to sports. A new phenomenon author noticed in two patients was a persistent avoidance behaviour for typical stress situations during sports. Even if both patients reported that this was not instability- and/or pain-related, this behaviour interfered with their return to sports. Even if this phenomenon was seldom, these findings might highlight the need for an intensive physiotherapy as well as the need of an individual sports therapy. The modified technique shows encouraging results in terms of a sufficient stabilization of the patellofemoral joint, a low incidence of complications and a good outcome in terms of pain, cosmetic results and return to sports. The preliminary clinical results of authors’ technique demonstrate a good efficiency in relieving the symptoms and improving the function of the affected knee. Therefore, authors will continue this method in the future when indicated. In three patients, authors noticed a slight flexion deficit at the last follow-up. Considering this phenomenon, authors changed the postoperative treatment schedule to a protocol without any postoperative limitations of flexion. Furthermore, authors will try to ensure intensive postoperative motion exercises by using continuous passive motion devices, etc.
The comparatively good outcome presented in authors’ study should not be taken for granted. The need for an individual postoperative physio- and sports therapy is also outlined in this study. A larger clinical outcome study with longer follow-up periods is needed to investigate long-term outcome results of authors’ methods. This will assess the durability of the clinical results. Furthermore, data on the prevention of a secondary arthritis are of interest in this patient group, which normally shows high rates of osteoarthritis development. Besides further improvements of the surgical technique, the questions of how to optimize and individualize the postoperative physio- and sports therapy will be of interest. A larger long-term clinical outcome study on the clinical results and the prevention of secondary arthritis will be a useful method for the future research.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Germany
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Mariano FF, Tuncyurek O S- Editor: Cui LJ L- Editor: A E- Editor: Lu YJ
| 1. | Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10:215-220. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 533] [Cited by in F6Publishing: 541] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 2. | Heegaard J, Leyvraz PF, Curnier A, Rakotomanana L, Huiskes R. The biomechanics of the human patella during passive knee flexion. J Biomech. 1995;28:1265-1279. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 135] [Cited by in F6Publishing: 114] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 3. | Amis AA, Oguz C, Bull AM, Senavongse W, Dejour D. The effect of trochleoplasty on patellar stability and kinematics: a biomechanical study in vitro. J Bone Joint Surg Br. 2008;90:864-869. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 4. | Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19-26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1326] [Cited by in F6Publishing: 1170] [Article Influence: 39.0] [Reference Citation Analysis (0)] |
| 5. | Arendt EA, Moeller A, Agel J. Clinical outcomes of medial patellofemoral ligament repair in recurrent (chronic) lateral patella dislocations. Knee Surg Sports Traumatol Arthrosc. 2011;19:1909-1914. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 76] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 6. | Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40:1916-1923. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 308] [Cited by in F6Publishing: 321] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 7. | Howells NR, Barnett AJ, Ahearn N, Ansari A, Eldridge JD. Medial patellofemoral ligament reconstruction: a prospective outcome assessment of a large single centre series. J Bone Joint Surg Br. 2012;94:1202-1208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 129] [Cited by in F6Publishing: 138] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 8. | Sanchis-Alfonso V, Montesinos-Berry E, Ramirez-Fuentes C, Leal-Blanquet J, Gelber PE, Monllau JC. Failed medial patellofemoral ligament reconstruction: Causes and surgical strategies. World J Orthop. 2017;8:115-129. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 27] [Cited by in F6Publishing: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Wagner D, Pfalzer F, Hingelbaum S, Huth J, Mauch F, Bauer G. The influence of risk factors on clinical outcomes following anatomical medial patellofemoral ligament (MPFL) reconstruction using the gracilis tendon. Knee Surg Sports Traumatol Arthrosc. 2013;21:318-324. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 161] [Cited by in F6Publishing: 157] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 10. | Nelitz M, Williams RS, Lippacher S, Reichel H, Dornacher D. Analysis of failure and clinical outcome after unsuccessful medial patellofemoral ligament reconstruction in young patients. Int Orthop. 2014;38:2265-2272. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 11. | Nomura E, Horiuchi Y, Inoue M. Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee. 2002;9:139-143. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 163] [Cited by in F6Publishing: 161] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 12. | Kang HJ, Wang F, Chen BC, Zhang YZ, Ma L. Non-surgical treatment for acute patellar dislocation with special emphasis on the MPFL injury patterns. Knee Surg Sports Traumatol Arthrosc. 2013;21:325-331. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Fucentese SF, Schöttle PB, Pfirrmann CW, Romero J. CT changes after trochleoplasty for symptomatic trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2007;15:168-174. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 14. | von Engelhardt LV, Fuchs T, Weskamp P, Jerosch J. Effective patellofemoral joint stabilization and low complication rates using a hardware-free MPFL reconstruction technique with an intra-operative adjustment of the graft tension. Knee Surg Sports Traumatol Arthrosc. 2017; Epub ahead of print. [PubMed] [Cited in This Article: ] |
| 15. | Parikh SN, Nathan ST, Wall EJ, Eismann EA. Complications of medial patellofemoral ligament reconstruction in young patients. Am J Sports Med. 2013;41:1030-1038. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 177] [Cited by in F6Publishing: 176] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 16. | Neri T, Philippot R, Carnesecchi O, Boyer B, Farizon F. Medial patellofemoral ligament reconstruction: clinical and radiographic results in a series of 90 cases. Orthop Traumatol Surg Res. 2015;101:65-69. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 17. | Carrillon Y, Abidi H, Dejour D, Fantino O, Moyen B, Tran-Minh VA. Patellar instability: assessment on MR images by measuring the lateral trochlear inclination-initial experience. Radiology. 2000;216:582-585. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 235] [Cited by in F6Publishing: 213] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 18. | Aframian A, Smith TO, Tennent TD, Cobb JP, Hing CB. Origin and insertion of the medial patellofemoral ligament: a systematic review of anatomy. Knee Surg Sports Traumatol Arthrosc. 2017;25:3755-3772. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 58] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 19. | Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:801-804. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 460] [Cited by in F6Publishing: 430] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 20. | Longo UG, Vincenzo C, Mannering N, Ciuffreda M, Salvatore G, Berton A, Denaro V. Trochleoplasty techniques provide good clinical results in patients with trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2017; Epub ahead of print. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 21. | Dejour D, Saggin P. The sulcus deepening trochleoplasty-the Lyon‘s procedure. Int Orthop. 2010;34:311-316. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 195] [Cited by in F6Publishing: 176] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 22. | Goutallier D, Raou D, Van Driessche S. Retro-trochlear wedge reduction trochleoplasty for the treatment of painful patella syndrome with protruding trochleae. Technical note and early results. Rev Chir Orthop Reparatrice Appar Mot. 2002;88:678-685. [PubMed] [Cited in This Article: ] |
| 23. | Thaunat M, Bessiere C, Pujol N, Boisrenoult P, Beaufils P. Recession wedge trochleoplasty as an additional procedure in the surgical treatment of patellar instability with major trochlear dysplasia: early results. Orthop Traumatol Surg Res. 2011;97:833-845. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 24. | Bereiter H, Gautier E. Trochleoplasty as surgical approach for the treatment of recurrent patella instability in patients with trochlear dysplasia of the femur [in German. Arthroskopie. 1994;7:281-286. [Cited in This Article: ] |
| 25. | Schöttle PB, Schell H, Duda G, Weiler A. Cartilage viability after trochleoplasty. Knee Surg Sports Traumatol Arthrosc. 2007;15:161-167. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 67] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 26. | Nelitz M, Dreyhaupt J, Lippacher S. Combined trochleoplasty and medial patellofemoral ligament reconstruction for recurrent patellar dislocations in severe trochlear dysplasia: a minimum 2-year follow-up study. Am J Sports Med. 2013;41:1005-1012. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 96] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 27. | Metcalfe AJ, Clark DA, Kemp MA, Eldridge JD. Trochleoplasty with a flexible osteochondral flap: results from an 11-year series of 214 cases. Bone Joint J. 2017;99-B:344-350. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 28. | Banke IJ, Kohn LM, Meidinger G, Otto A, Hensler D, Beitzel K, Imhoff AB, Schöttle PB. Combined trochleoplasty and MPFL reconstruction for treatment of chronic patellofemoral instability: a prospective minimum 2-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2014;22:2591-2598. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 87] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 29. | Fucentese SF, Zingg PO, Schmitt J, Pfirrmann CW, Meyer DC, Koch PP. Classification of trochlear dysplasia as predictor of clinical outcome after trochleoplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19:1655-1661. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 76] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 30. | von Knoch F, Böhm T, Bürgi ML, von Knoch M, Bereiter H. Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia. A 4- to 14-year follow-up study. J Bone Joint Surg Br. 2006;88:1331-1335. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 200] [Cited by in F6Publishing: 204] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 31. | Utting MR, Mulford JS, Eldridge JD. A prospective evaluation of trochleoplasty for the treatment of patellofemoral dislocation and instability. J Bone Joint Surg Br. 2008;90:180-185. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 114] [Cited by in F6Publishing: 116] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 32. | Schöttle PB, Fucentese SF, Pfirrmann C, Bereiter H, Romero J. Trochleaplasty for patellar instability due to trochlear dysplasia: A minimum 2-year clinical and radiological follow-up of 19 knees. Acta Orthop. 2005;76:693-698. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 149] [Cited by in F6Publishing: 152] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 33. | Chouteau J. Surgical reconstruction of the medial patellofemoral ligament. Orthop Traumatol Surg Res. 2016;102:S189-S194. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 34. | Elias JJ, Cosgarea AJ. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med. 2006;34:1478-1485. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 282] [Cited by in F6Publishing: 239] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 35. | Thaunat M, Erasmus PJ. The favourable anisometry: an original concept for medial patellofemoral ligament reconstruction. Knee. 2007;14:424-428. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 91] [Cited by in F6Publishing: 89] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 36. | Feller JA, Richmond AK, Wasiak J. Medial patellofemoral ligament reconstruction as an isolated or combined procedure for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22:2470-2476. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 94] [Cited by in F6Publishing: 91] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 37. | Steiner TM, Torga-Spak R, Teitge RA. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med. 2006;34:1254-1261. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 234] [Cited by in F6Publishing: 204] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 38. | Blønd L, Haugegaard M. Combined arthroscopic deepening trochleoplasty and reconstruction of the medial patellofemoral ligament for patients with recurrent patella dislocation and trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2014;22:2484-2490. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 39. | Camathias C, Studer K, Kiapour A, Rutz E, Vavken P. Trochleoplasty as a Solitary Treatment for Recurrent Patellar Dislocation Results in Good Clinical Outcome in Adolescents. Am J Sports Med. 2016;44:2855-2863. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 40. | Donell ST, Joseph G, Hing CB, Marshall TJ. Modified Dejour trochleoplasty for severe dysplasia: operative technique and early clinical results. Knee. 2006;13:266-273. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 133] [Cited by in F6Publishing: 126] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 41. | Dejour D, Byn P, Ntagiopoulos PG. The Lyon‘s sulcus-deepening trochleoplasty in previous unsuccessful patellofemoral surgery. Int Orthop. 2013;37:433-439. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 77] [Cited by in F6Publishing: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 42. | Ntagiopoulos PG, Byn P, Dejour D. Midterm results of comprehensive surgical reconstruction including sulcus-deepening trochleoplasty in recurrent patellar dislocations with high-grade trochlear dysplasia. Am J Sports Med. 2013;41:998-1004. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 105] [Article Influence: 9.5] [Reference Citation Analysis (0)] |