Abstract
Vitamin C is known to protect mucosal tissues from oxidative stress and inhibit nitrosamine formation in the stomach. High consumption of fruits, particularly citrus, and higher circulating vitamin C concentrations may be inversely associated with gastric cancer (GC) risk. We investigated 20 polymorphisms in vitamin C transporter genes SCL23A1 and SCL23A2 and GC risk in 365 cases and 1,284 controls nested within the European Prospective Investigation into Cancer and Nutrition cohort. We also evaluated the association between these polymorphisms and baseline plasma vitamin C levels in a subset of participants. Four SNPs were predictors of plasma vitamin C levels (SLC23A1 rs11950646 and rs33972313; SLC23A2 rs6053005 and rs6133175) in multivariable linear regression models. One SNP (SLC23A2 rs6116569) was associated with GC risk, in particular non-cardia GC (OR = 1.63, 95 % CI = 1.11–2.39, based on 178 non-cardia cases), but this association was attenuated when plasma vitamin C was included in the logistic regression model. Haplotype analysis of SLC23A1 yielded no associations with GC. In SLC23A2, one haplotype was associated with both overall and non-cardia GC, another haplotype was associated with GC overall, and a third was associated with intestinal-type GC. Common variants in SLC23A1 and SLC23A2 may influence plasma vitamin C concentration independent of dietary intake, and variation in SLC23A2 may influence GC risk. Additional prospective studies in large populations and consortia are recommended. Investigation of variation in vitamin C transporter genes may shed light on the preventative properties of vitamin C in gastric carcinogenesis.
Similar content being viewed by others
Introduction
Although incidence has been declining, gastric cancer (GC) is still the second leading cause of cancer death worldwide (Jemal et al. 2010). High consumption of fruits, particularly citrus fruits, has been inversely associated with GC risk (Gonzalez et al. 2006, 2012; Tsugane and Sasazuki 2007). Studies that have specifically investigated dietary intake or plasma levels of l-ascorbic acid (vitamin C) and GC risk also have reported inverse associations, supporting the hypothesis that antioxidants (such as vitamin C) from fruit may be protective against the development of GC (Jenab et al. 2006a, b). Indeed, vitamin C, an enzymatic cofactor and scavenger of reactive oxygen species, has been shown to inhibit nitrosamine formation in the stomach (Tannenbaum et al. 1991) and protect mucosal tissues from the damaging effects of oxidative stress (Drake et al. 1996; Sasazuki et al. 2008).
Infection of the gastric epithelium with Helicobacter pylori (H. pylori cagA+ strains) is the strongest known risk factor for non-cardia GC, but H. pylori infection itself is not a sufficient cause for GC development; thus, additional lifestyle, environmental, and host genetic factors also play a role (Polk and Peek 2010; Peek and Blaser 2002). H. pylori cagA+ infection in the gastric mucosa has been associated with pro-inflammatory responses and mucosal proliferation, as well as lower vitamin C levels in blood and gastric juice, possibly due to malabsorption or decreased stability and bioavailability (Lahner et al. 2012). In addition, very high doses of vitamin C may inhibit H. pylori infection, growth, and reinfection (Pal et al. 2011; Zhang et al. 1997). As a consequence, the multistep process of gastric cancer carcinogenesis involving chronic H. pylori infection may be slowed or partially reversed in some individuals with high intake of vitamin C.
Vitamin C absorption and reabsorption by the gastrointestinal tract and renal system, respectively, is accomplished by active transport across plasma membranes involving two transporter proteins encoded by the sodium-dependent vitamin C transporter genes, SLC23A1 and SLC23A2. SLC23A1 encodes SVCT1 which is the ascorbate transporter believed to be primarily involved in whole-body homeostasis and circulating vitamin C levels, while SVCT2 encoded by SLC23A2 is believed to be involved in vitamin C regulation within specific metabolically active tissue (Savini et al. 2008). Both transporter genes have known genetic variants, but little is known about the influence of such variants on the risk for GC.
Only one case–control study has investigated variants in these genes and GC risk, and this study (based on 279 cases and 414 controls) identified an association with a variant in SLC23A2 (Wright et al. 2009). We conducted a case–control study (based on 365 cases and 1,284 controls) nested within the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort of 20 vitamin C transporter gene polymorphisms and haplotypes and GC risk, with additional consideration of these SNPs as predictors of baseline plasma levels of vitamin C in a subset of participants.
Materials and methods
EPIC cohort study population and dietary and lifestyle assessment
European Prospective Investigation into Cancer and Nutrition is a multicenter prospective cohort of over 500,000 participants recruited through 23 research center from 10 European countries including France, Italy (Florence, Turin, Varese, Naples, Ragusa), Spain (Asturias, Granada, Murcia, Navarra, San Sebastian), the United Kingdom (Cambridge, Oxford), The Netherlands (Bilthoven, Utrecht), Greece, Germany (Heidelberg, Potsdam), Sweden (Malmö, Umeå), Denmark (Aarhus, Cøpenhagen), and Norway (Riboli et al. 2002). The majority of cohort participants were recruited between 1992 and 1998 at ages between 35 and 70 years. Cohort participants were recruited from the general population residing in geographic areas including towns and provinces (in Greece, Norway and France, participants were recruited from throughout these countries). The French cohort comprised women who were members of a teachers’ organization health insurance program, cohorts from Utrecht and Florence comprised women attending population-based breast cancer screening programs, parts of the Italian and Spanish cohorts comprised blood donors, and most of the Oxford cohort comprised vegetarian volunteers. Written informed consent was obtained from all EPIC participants. The EPIC cohort and the EurGast study (nested case–control study described below) were approved by ethical committees from the International Agency for Research on Cancer (IARC) and each of the 23 EPIC study centers. Validated, country-specific food intake questionnaires were used to assess regular diet in cohort participants at baseline (Riboli et al. 2002). Vitamin C intake from food sources was estimated using standardized country-specific food composition tables (Slimani et al. 2007). Separate lifestyle questionnaires were used to collect baseline information on non-dietary factors such as tobacco smoking, physical activity, and history of medical conditions.
Identification of gastric cancer cases
Follow-up for these analyses was through 2003–2006, depending upon the study center. In general, case identification was based upon information available from population cancer registries except in France, Greece, Germany, and Naples (Italy) where a combination of methods including health insurance records, hospital-based cancer and pathology registries, and active participant tracking was used. GC for these analyses included diagnoses coded as C16 according to the 10th revision of the International Classification of Disease (ICD-10). A total of 665 GC cases were observed (487 adenocarcinomas, 145 non-adenocarcinomas, 7 stump tumors and 26 not specified) of which a total of 444 were first, incident, primary gastric adenocarcinomas (hereafter referred to as gastric cancer or GC). Cases were validated for histologic (diffuse, intestinal, mixed, or not specified using Lauren’s classification) and anatomic subtypes (cardia C16.0, non-cardia C16.1-9, mixed, or not specified) by a panel of pathologists who reviewed original pathology reports, tumor slides, and paraffin blocks obtained on GC cases from EPIC centers (Carneiro et al. 2007).
Nested case–control study of gastric adenocarcinoma
A nested case–control study of primary incident gastric adenocarcinoma (Eurgast) was designed to efficiently study biomarkers and genetic susceptibility in relation to GC risk in the EPIC cohort (Sala et al. 2012). Each incident primary GC case with an available blood sample was matched by study center, sex, age group (±2.5 years), and date of blood collection (±45 days) to four control participants randomly selected from the cohort at risk at the time of diagnosis of the index case. There were 365 GC cases (181 non-cardias, 107 cardias, and 77 with mixed or unspecified anatomic subsite; and 126 intestinal, 128 diffuse, and 111 with mixed or unspecified histologic subtype) and 1,284 controls with complete genetic information. There were 172 GC cases and 311 controls with both genetic and plasma vitamin C information. Helicobacter pylori (H. pylori) infection was determined by quantification of H. pylori-specific IgG antibodies in the plasma of cases and controls (originally collected at cohort enrollment) using enzyme-linked immunosorbent assay (ELISA) (Pyloriset EIA-GIII®) and Western blot (HELICOBLOT2.1) (Gonzalez et al. 2006, 2011; Palli et al. 2007). Participants were categorized as positive for H. pylori infection if they were positive for anti-H. pylori antibodies or cagA antibodies or both (Gonzalez et al. 2011). Pepsinogen I levels were quantified in nested cases and controls by ELISA using kits from Biohit (Helsinki, Finland) in order to classify the presence or absence of severe chronic atrophic gastritis (SCAG) at the time of cohort enrollment (Palli et al. 2007). Nested participants were classified as having evidence of SCAG if their pepsinogen I level was <22 μg/l, and no evidence of SCAG if their pepsinogen I level was ≥22 μg/l (Broutet et al. 2003).
Single-nucleotide polymorphism selection and genotyping
This study was part of a candidate gene study of GC susceptibility which genotyped 1,285 single-nucleotide polymorphisms (SNPs) within 249 genetic loci on a customized array using the Illumina Beadstation Platform and GoldenGate technology (Illumina, San Diego, CA) (Duell et al. 2012; Sala et al. 2012). Genomic DNA was extracted from frozen buffy coats and genotyping performed at the Spanish National Genotyping Center (CEGEN) in Barcelona. Selection strategies for this analysis involved choosing common SNPs with haplotype-tagging potential (MAF ≥ 5 %) or with known functionality (rs33972313) (Timpson et al. 2010). Four SNPs were selected and successfully genotyped in the 21-kb region containing SLC23A1, and 19 SNPs were selected in the 205-kb region containing SLC23A2, but three of these were eliminated due to inadequate cluster separation (rs3787455, rs1776964, and rs2064842). Five percent of the samples were genotyped in duplicate to assess genotyping error (proportion concordant—99.2 %).
Plasma vitamin C assay
Vitamin C levels (μmol/L) were previously determined in thawed plasma samples using a fluorometric method described in detail in our previous study of vitamin C levels and GC risk (Vuilleumier and Keck 1989; Jenab et al. 2006b). The effect of long-term cryopreservation on the stability of plasma vitamin C in the EPIC cohort also has been previously described, and in brief, while samples with higher baseline concentrations tended to lose more vitamin C than samples with lower concentrations, the methods and assays for plasma vitamin C concentration were determined to be reliable without the addition of stabilizing agents (Jenab et al. 2005).
Statistical analysis
A Kruskal–Wallis one-way analysis of variance by ranks test was used to compare median plasma vitamin C level for each SNP genotype. Multiple linear regression models of loge-transformed plasma vitamin C levels as the outcome and SNPs as predictors were also evaluated in 311 controls participants. All linear regression models of plasma vitamin C level were adjusted for age (in 5-year categories), sex, country, baseline smoking intensity (never smoker, former smoker quit 20+ years, former quit 11–20 years, former quit ≤10 years, occasional smoker or pipe or cigar user, current smoker 1–15 cigs./day, current 16–25 cigs./day, current 26+ cigs/day), H. pylori infection, and season of blood draw. To improve precision, unconditional logistic regression modeling was used to estimate the odds ratio (OR) for vitamin C SNPs and GC risk adjusting for age (in 5-year categories), sex, country, smoking status (never, former, current), H. pylori infection, and season of blood draw. Unconditional regression models included the variables used in the matching process (age at recruitment ±2.5 years, sex, center/country, date of blood draw ±45 days) and were compared with conditional models where appropriate. Analyses of vitamin C transporter SNPs and GC risk evaluated log-additive (per allele), codominant, dominant, and recessive genetic models. The possibility of population stratification was considered, but since the observed distribution of P values for the final 1,285 SNPs that passed QC in Eurgast was well fitted by a uniform distribution, genomic control was not needed (Sala et al. 2012). Vitamin C–SNP interactions were explored for those SNPs found to be significantly associated with GC risk or with plasma vitamin C levels. Cutpoints for vitamin C and dietary intake variables were based on medians or tertiles of the distributions for these variables in controls. Tests for statistical significance of interactions were based on a likelihood ratio test (LRT) and represent departures from a multiplicative model. All statistical tests were two-sided, and all analyses were performed using the R package (v. 2.12.2) and the SNPassoc library (Gonzalez et al. 2007).
Haplotype analysis
Linkage disequilibrium (LD) between SNPs in each gene region (SLC23A1 and SLC23A2) was assessed and haplotype frequencies inferred using the EM algorithm as implemented in the haplo.stats R package. SNPs with >5 % missing data were not included in haplotype analyses (rs3914810). ORs for haplotypes with minimum frequency ≥5 % and GC risk were estimated using the most common haplotype as the referent group and were adjusted for age, sex, country, smoking status, H. pylori infection, and season of blood draw. Since haploview analysis of downloaded genotype data from the CEU population in Hapmap revealed a single LD block in SLC23A1 (21-kb), the four SNP markers in this gene were analyzed as one haplotype block. SLC23A2 is a much larger gene (205 kb), and haplotypes were analyzed in four LD blocks according to haploview analysis of CEU genotype data from Hapmap.
Results
The median time interval between blood collection and diagnosis for the 365 GC cases was 4.7 years. GC cases and nested controls were similar with regard to age, country, and sex as these were variables used in the nested case–control matching procedure (Table 1). With regard to smoking status, cases were about 80 % more likely to be current smokers at baseline than controls, about 3.2 times more likely to be positive for H. pylori infection, and 30 % less likely to have plasma vitamin C concentrations at or above the upper tertile in controls (≥45 μmol/L), although differences in vitamin C concentration were not statistically significant (Table 1). Cases were 31 % less likely to have questionnaire-based vitamin C intake from food sources at or above the upper tertile in controls (≥135.8 mg/day) and were 60 % more likely to be at or above the upper tertile of the processed meat intake (≥39.6 g/day) (Table 1). All SLC23A1 and SLC23A2 SNPs passed Hardy–Weinberg equilibrium in controls (all P values >0.05). Genotype information for rs3914810 and rs6596473 in SLC23A2 was missing in 14.9 and 4.2 % of participants, respectively; the remaining SNPs had less than 1.7 % of participants with missing genotype data (data not shown).
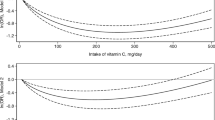
Multivariable linear regression models of loge-transformed plasma vitamin C level as the dependent variable and loge-transformed questionnaire-based vitamin C intake as the independent variable indicated that food intake explained only 5 % of the variability in plasma vitamin C levels (P value 0.001, data not shown). Median plasma vitamin C levels in controls were evaluated according to the genotype of each SNP in SLC23A1 and SLC23A2. None of the Kruskal–Wallis test statistics evaluating the unadjusted association between genotype and median plasma vitamin C level were statistically significant (all P values >0.06) (data not shown). In multiple linear regression analyses (n = 311 controls) of the natural log of plasma vitamin C as the dependent variable and SLC23A1 and SLC23A2 SNPs as independent variables, regression coefficients were statistically significant for the following four SNPs: SLC23A1 rs11950646 (dominant model P value: 0.03; log-additive model P value 0.02), SLC23A1 rs33972313 (codominant model P value 0.04), SLC23A2 rs6053005 (recessive model P value 0.007), and SLC23A2 rs6133175 (recessive model P value 0.02) (Table 2). In SLC23A1, rs11950646 GG or AG genotypes (compared with AA) were associated with a 13 % lower plasma vitamin C concentration (10 % lower per G allele in a log-additive model), and rs33972313 GA heterozygotes were associated with a 24 % lower concentration. In SLC23A2, rs6053005 TT homozygotes and rs6133175 GG homozygotes were associated with 24 % higher plasma vitamin C concentrations (Table 2). For all remaining SNPs and genetic models, there were no statistically significant predictors of plasma vitamin C levels (all β parameter P values >0.10, data not shown). We conducted regression analyses of questionnaire-based vitamin C intake (mg/day) from food sources as a predictor of plasma vitamin C levels, stratified by the genotypes of these four SNPs (one at a time) under a recessive or dominant model and found no evidence for effect modification (all P values for interaction >0.30, data not shown), but data were sparse. We also evaluated potential interactions in relation to GC risk between plasma vitamin C or questionnaire-based vitamin C intake from food sources and intakes of processed and red meat (with cutpoints based on both the median and tertiles in controls), but found no evidence for effect measure modification (all P values for interaction >0.1, data not shown).
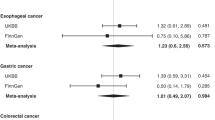
Multivariable logistic regression analysis of the association between SLC23A1 and SLC23A2 genotypes and GC risk gave evidence of a positive association for one SNP in SLC23A2 (rs6116569) (Table 3). The heterozygous genotype was statistically significantly associated with GC risk, while the homozygous variant was also associated with risk, but was not statistically significant (Table 3). In a dominant model (rs6116569 CT + TT vs. CC), the OR for overall GC was 1.36 and 95 % CI 1.04–1.79. The known functional variant in SLC23A1 (rs33972313) was not associated with GC risk in our study (Table 3).
Supplemental Table S1 gives dominant model ORs and 95 % CIs for each SNP according to GC anatomic location (non-cardia, cardia) and histologic subtype (intestinal, diffuse). Analysis of rs6116569 (CT + TT vs. CC) and GC risk by anatomic location suggested that the association observed for this SNP with overall GC (Table 3) was for non-cardia GC (OR 1.63, 95 % CI 1.11–2.39, based on 178 non-cardia cases) and not cardia GC (OR 1.01, 95 % CI 0.65–1.57, based on 107 cardia cases); however, the convergence of the logistic regression model for rs6116569 and cardia GC was questionable due to the limited number of cardia cases in some EPIC countries (the corresponding OR without considering country was 1.05, 95 % CI = 0.68–1.63). Analyses of the association between rs6116569 and GC by histology indicated no major differences (for intestinal, OR 1.50, 95 % CI 0.97–2.32, based on 121 cases; and for diffuse, OR 1.20, 95 % CI 0.79–1.83, based on 123 cases). No other SNPs were associated with GC risk by anatomic location or histologic subtype (with the exception of rs1279685 and the intestinal subtype, but the OR was of borderline statistical significance) (Supplemental Table S1). Additional analyses of the association between rs6116569 and GC risk stratified by plasma vitamin C level and by the SNPs found to be associated with plasma vitamin C yielded no evidence for effect measure modification by these covariates (all P values for interaction >0.2, data not shown). We also ran a logistic regression model of the association between rs6116569 and GC risk including a variable for plasma vitamin C level (in addition to age, sex, country, smoking status, H. pylori infection, and season of blood draw): the dominant model OR was 1.15, 95 % CI 0.74–1.80, based on 172 GC cases and 311 controls. The OR for rs6116569 and GC risk in the same 172 cases and 311 controls without the variable for plasma vitamin C was 1.16, 95 % CI 0.74–1.81. We then estimated ORs for rs6116569 and GC risk stratified by SCAG status and observed slightly different adjusted ORs (SCAG ‘+’/pepsinogen I < 22 μg/l, OR 1.11, 95 % CI 0.37–3.38; SCAG ‘−’/pepsinogen I ≥ 22 μg/l, OR 1.55, 95 % CI 1.11–2.16) but the difference was not statistically significant (interaction P value: 0.66).
We investigated whether plasma vitamin C level modified associations between each SLC23A1 or SLC23A2 genotype and GC risk and found no evidence for effect measure modification (all interaction P values >0.1, except for rs6052961 which had the lowest P value of 0.07) (data not shown).
Finally, we conducted an adjusted analysis of SLC23A1 haplotype and GC risk and found no evidence for haplotype–disease associations (Table 4). An adjusted analysis of SLC23A2 haplotypes showed a statistically significant positive association between haplotype CGTC in block 1 and GC (Table 4), and further analysis revealed that the association was observed primarily in non-cardia GC (OR 1.52; 95 % CI 1.14–2.03) (subsite data not in table). When we included a variable for log plasma vitamin C in the model, CGTC haplotype-specific ORs were attenuated and no longer statistically significant (data not shown). A statistically significant positive association between haplotype ATC in block 3 and GC was also observed (Table 4). No overall association was observed between haplotypes in block 4 and GC, but an association between haplotype GCA and intestinal-type GC was identified (OR 1.43; 95 % CI 1.04–1.97) (subtype data not in table). This haplotype contains variant allele A (SNP rs1279685), which by itself was associated with intestinal-type GC (supplemental Table S1).
Discussion
In this nested case–control study of vitamin C transporter genes and GC risk within the EPIC cohort, we identified one SLC23A2 marker (rs6116569, intronic) associated with GC risk, and two markers in SLC23A2 (rs6053005, rs6133175) and two in SLC23A1 (rs33972313, rs11950646) as predictors of plasma vitamin C concentration. The magnitude of the inverse association between plasma vitamin C concentration and GC risk previously reported in EPIC was moderate (highest vs. lowest quartile, OR 0.55, 95 % CI 0.31–0.97) representing a 45 % lower risk (Jenab et al. 2006b). In the previous analysis which included fewer GC cases (n = 215), questionnaire-based vitamin C intake from foods was not associated with GC risk (Jenab et al. 2006b); however, with additional GC cases in the present analysis (n = 365), higher intakes of vitamin C from foods were statistically significantly associated with reduced GC risk. In contrast, questionnaire-based vitamin C intake was not a strong predictor of plasma vitamin C concentration in our study, and none of the SNP markers we tested improved this prediction.
Since the four markers (two in SLC23A2 and two in SLC23A1) were only moderate predictors of plasma vitamin C concentration in controls (n = 311), it is perhaps not surprising that we did not identify them as predictors of GC risk. None of the identified haplotypes in SLC23A1 (based on four markers) were associated with GC risk, but three haplotypes in SLC23A2 (based on 15 markers in 4 LD blocks) were associated with GC risk: one with both non-cardia and overall GC, one with overall GC, and one with the intestinal subtype.
The association between SLC23A2 rs6116569 and GC risk, in particular non-cardia GC, suggests that this variant may influence cancer risk in the distal stomach; however, this association (and the haplotype-specific OR) was attenuated and no longer statistically significant when we included a variable for plasma vitamin C concentration in the regression models, suggesting that this variant may not be an independent susceptibility factor for GC risk. SLC23A2 rs6116569 is a tagSNP with unknown function, and in our data, it showed no detectable effect on plasma vitamin C levels. Our results showing associations between the SNP markers rs11950646, rs6053005, and rs6133175 and plasma vitamin C concentration have not been directly observed in other study populations; however, previous studies have evaluated SLC23A1 and SLC23A2 SNPs and blood vitamin C concentrations in large sample sizes (Cahill and El-Sohemy 2009; Timpson et al. 2010).
Cahill and El-Sohemy reported an association between SLC23A1 rs4257763 and mean serum vitamin C levels from 12-h fasting blood in a cross-sectional study of 1,277 volunteers (39 % Caucasian, and 29 % East Asian and the remainder of mixed race/ethnicity) (Cahill and El-Sohemy 2009). SLC23A1 rs4257763 is not in HapMap, but has been reported to be in partial LD with rs6596473 (for which we observed no associations) (Cahill and El-Sohemy 2009). Timpson and colleagues performed a large-scale analysis of genetic variants at the SLC23A1 locus and 6-h fasting blood vitamin C levels in over 15,000 Caucasian participants from five longitudinal studies (Timpson et al. 2010). They identified a rare variant (rs33972313) in SLC23A1 that was statistically significantly associated with circulating blood vitamin C concentration. In our study, variant rs33972313 (GA genotype) was a predictor of lower plasma vitamin C level, which is in agreement with the much larger study of Timpson et al. This variant lies in exon 8, results in a missense change, and has MAF of 3 % in Caucasians; thus, it is relatively uncommon.
Only one previous study of SLC23A1 and SLC23A2 SNP markers and GC risk has been published, a population-based case–control study from Poland (Wright et al. 2009). In that study, the authors analyzed 279 GC cases and 414 population-based controls and identified an association between SLC23A2 rs12479919 and GC risk with no effect modification by vitamin C intake and no associations with markers in SLC23A1. SLC23A2 rs12479919 is not in LD with rs6116569 for which we observed an association with GC. Further, none of the SLC23A2 markers evaluated in the Polish study are in LD with rs6116569 (all r 2 < 0.4). Although the evaluated SNP markers were not the same, the Polish study and our study suggest that variation in SLC23A1 does not influence GC risk, but that variation in SLC23A2 could play a limited role in GC susceptibility.
The functions of SLC23A1 and SLC23A2 are to encode and express SVCT1 and SVCT2, key proteins for the transport and accumulation of vitamin C in mammalian cells and tissues (Savini et al. 2008). SVCTs are surface glycoproteins that show distinct functions and tissue distributions, with SVCT1 having a role in whole organism vitamin C homeostasis and SVCT2 playing a role in oxidative stress management in metabolically active tissues (Savini et al. 2008). Interestingly, SVCT2 has been detected in rat gastric tissue, but not SVCT1, the protein product of SLC23A1 (Tsukaguchi et al. 1999). Our study identified one SNP marker (and haplotypes) in association with GC risk from the SLC23A2 gene, the homologous gene found in rat gastric tissue. Little is known about the distribution of these proteins in humans, but the genes are highly conserved in humans and rodents, indicating a common ancestral gene (Eck et al. 2004; Savini et al. 2008). Little is known about the possible functions of the SNP markers for which we and others have observed associations (Chen et al. 2009; Erichsen et al. 2006; Wright et al. 2009; Skibola et al. 2008), but discrepancies across studies could also reflect different expression patterns for these genes in different tissues.
Potential mechanisms for a protective effect of vitamin C in gastric carcinogenesis include its antioxidant properties, as well as inhibition of N-nitroso compound formation in the stomach (often elevated in persons with high intakes of processed meat) (Drake et al. 1996; Sasazuki et al. 2008; Tannenbaum et al. 1991). In our data, we did not observe a statistically significant interaction between dietary intake of vitamin C (or plasma concentration of vitamin C) and processed meat intake. Another potential mechanism is that vitamin C may act by inhibiting or slowing the infection and growth of H. pylori in the gastric mucosa (Pal et al. 2011; Zhang et al. 1997). Weaknesses of our study include potential misclassification of dietary intake of foods containing vitamin C (and lack of information on use of dietary supplements) and imprecision in plasma vitamin C measurements. Our sample size was relatively small, especially when evaluating plasma vitamin C levels and genotypes together as these data were available only in a subset of genotyped participants; thus, we may have missed subtle effects of some SLC23A1 and SLC23A2 markers. Further, some of the associations we report may have been due to chance. Our study had limited precision for evaluating rare markers or risks within anatomic subtypes (i.e., non-cardias). Since over 80 % of our GC cases were positive for H. pylori infection, we were unable to evaluate interactions between H. pylori and vitamin C intake or plasma levels. Strengths of our study were that blood collection and dietary assessment occured at baseline; thus, our study avoided many of the biases inherent to retrospective study designs.
In conclusion, we identified two markers in SLC23A1 and two in SLC23A2 that were predictors of plasma vitamin C concentration in controls and one additional marker in SLC23A2 (and corresponding haplotype) that was moderately associated with risk for non-cardia GC in the EPIC cohort. Additional prospective studies of common and rare variants in the vitamin C pathway and GC risk in larger populations and consortia are warranted.
References
Broutet N, Plebani M, Sakarovitch C, Sipponen P, Megraud F (2003) Pepsinogen A, pepsinogen C, and gastrin as markers of atrophic chronic gastritis in European dyspeptics. Br J Cancer 88:1239–1247
Cahill LE, El-Sohemy A (2009) Vitamin C transporter gene polymorphisms, dietary vitamin C and serum ascorbic acid. J Nutrigenet Nutrigenomics 2:292–301
Carneiro F, Moutinho C, Pera G, Caldas C, Fenger C, Offerhaus J, Save V, Stenling R, Nesi G, Mahlke U, Blaker H, Torrado J, Roukos DH, Sabourin JC, Boeing H, Palli D, Bueno-de-Mesquita HB, Overvad K, Bingham S, Clavel-Chapelon F, Lund E, Trichopoulou A, Manjer J, Riboli E, Gonzalez CA (2007) Pathology findings and validation of gastric and esophageal cancer cases in a European cohort (EPIC/EUR-GAST). Scand J Gastroenterol 42:618–627
Chen AA, Marsit CJ, Christensen BC, Houseman EA, McClean MD, Smith JF, Bryan JT, Posner MR, Nelson HH, Kelsey KT (2009) Genetic variation in the vitamin C transporter, SLC23A2, modifies the risk of HPV16-associated head and neck cancer. Carcinogenesis 30:977–981
Drake IM, Davies MJ, Mapstone NP, Dixon MF, Schorah CJ, White KL, Chalmers DM, Axon AT (1996) Ascorbic acid may protect against human gastric cancer by scavenging mucosal oxygen radicals. Carcinogenesis 17:559–562
Duell EJ, Sala N, Travier N, Munoz X, Boutron-Ruault MC, Clavel-Chapelon F, Barricarte A, Arriola L, Navarro C, Sanchez-Cantalejo E, Quiros JR, Krogh V, Vineis P, Mattiello A, Tumino R, Khaw KT, Wareham N, Allen NE, Peeters PH, Numans ME, Bueno-de-Mesquita HB, van Oijen MG, Bamia C, Benetou V, Trichopoulos D, Canzian F, Kaaks R, Boeing H, Bergmann MM, Lund E, Ehrnstrom R, Johansen D, Hallmans G, Stenling R, Tjonneland A, Overvad K, Ostergaard JN, Ferrari P, Fedirko V, Jenab M, Nesi G, Riboli E, Gonzalez CA (2012) Genetic variation in alcohol dehydrogenase (ADH1A, ADH1B, ADH1C, ADH7) and aldehyde dehydrogenase (ALDH2), alcohol consumption and gastric cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Carcinogenesis 33:361–367
Eck P, Erichsen HC, Taylor JG, Yeager M, Hughes AL, Levine M, Chanock S (2004) Comparison of the genomic structure and variation in the two human sodium-dependent vitamin C transporters, SLC23A1 and SLC23A2. Hum Genet 115:285–294
Erichsen HC, Engel SA, Eck PK, Welch R, Yeager M, Levine M, Siega-Riz AM, Olshan AF, Chanock SJ (2006) Genetic variation in the sodium-dependent vitamin C transporters, SLC23A1, and SLC23A2 and risk for preterm delivery. Am J Epidemiol 163:245–254
Gonzalez CA, Pera G, Agudo A, Bueno-de-Mesquita HB, Ceroti M, Boeing H, Schulz M, Del Giudice G, Plebani M, Carneiro F, Berrino F, Sacerdote C, Tumino R, Panico S, Berglund G, Siman H, Hallmans G, Stenling R, Martinez C, Dorronsoro M, Barricarte A, Navarro C, Quiros JR, Allen N, Key TJ, Bingham S, Day NE, Linseisen J, Nagel G, Overvad K, Jensen MK, Olsen A, Tjonneland A, Buchner FL, Peeters PH, Numans ME, Clavel-Chapelon F, Boutron-Ruault MC, Roukos D, Trichopoulou A, Psaltopoulou T, Lund E, Casagrande C, Slimani N, Jenab M, Riboli E (2006) Fruit and vegetable intake and the risk of stomach and oesophagus adenocarcinoma in the European Prospective Investigation into Cancer and Nutrition (EPIC-EURGAST). Int J Cancer 118:2559–2566
Gonzalez JR, Armengol L, Sole X, Guino E, Mercader JM, Estivill X, Moreno V (2007) SNPassoc: an R package to perform whole genome association studies. Bioinformatics 23:644–645
Gonzalez CA, Megraud F, Buissonniere A, Lujan BL, Agudo A, Duell EJ, Boutron-Ruault MC, Clavel-Chapelon F, Palli D, Krogh V, Mattiello A, Tumino R, Sacerdote C, Quiros JR, Sanchez-Cantalejo E, Navarro C, Barricarte A, Dorronsoro M, Khaw KT, Wareham N, Allen NE, Tsilidis KK, Bueno-de-Mesquita HB, Jeurnink SM, Numans ME, Peeters PH, Lagiou P, Valanou E, Trichopoulou A, Kaaks R, Lukanova-McGregor A, Bergman MM, Boeing H, Manjer J, Lindkvist B, Stenling R, Hallmans G, Mortensen LM, Overvad K, Olsen A, Tjonneland A, Bakken K, Dumeaux V, Lund E, Jenab M, Romieu I, Michaud D, Mouw T, Carneiro F, Fenge C, Riboli E (2011) Helicobacter pylori infection assessed by ELISA and by immunoblot and noncardia gastric cancer risk in a prospective study: the Eurgast-EPIC project. Ann Oncol 23:1320–1324
Gonzalez CA, Lujan-Barroso L, de Mesquita HB, Jenab M, Duell EJ, Agudo A, Tjonneland A, Boutron-Ruault MC, Clavel-Chapelon F, Touillaud M, Teucher B, Kaaks R, Boeing H, Steffen A, Trichopoulou A, Roukos D, Karapetyan T, Palli D, Tagliabue G, Mattiello A, Tumino R, Ricceri F, Siersema PD, Numans ME, Peeters PP, Parr CL, Skeie G, Lund E, Quiros JR, Sanchez-Cantalejo E, Navarro C, Barricarte A, Dorronsoro M, Ehrnstrom R, Regner S, Khaw KT, Wareham N, Key TJ, Crowe FL, Blaker H, Romieu I, Riboli E (2012) Fruit and vegetable intake and the risk of gastric adenocarcinoma: a reanalysis of the European prospective investigation into cancer and nutrition (EPIC-EURGAST) study after a longer follow-up. Int J Cancer 131(12):2910–2919
Jemal A, Center MM, DeSantis C, Ward EM (2010) Global patterns of cancer incidence and mortality rates and trends. Cancer Epidemiol Biomarkers Prev 19:1893–1907
Jenab M, Bingham S, Ferrari P, Friesen MD, Al-Delaimy WK, Luben R, Wareham N, Khaw KT, Riboli E (2005) Long-term cryoconservation and stability of vitamin C in serum samples of the European prospective investigation into cancer and nutrition. Cancer Epidemiol Biomarkers Prev 14:1837–1840
Jenab M, Riboli E, Ferrari P, Friesen M, Sabate J, Norat T, Slimani N, Tjonneland A, Olsen A, Overvad K, Boutron-Ruault MC, Clavel-Chapelon F, Boeing H, Schulz M, Linseisen J, Nagel G, Trichopoulou A, Naska A, Oikonomou E, Berrino F, Panico S, Palli D, Sacerdote C, Tumino R, Peeters PH, Numans ME, Bueno-de-Mesquita HB, Buchner FL, Lund E, Pera G, Chirlaque MD, Sanchez MJ, Arriola L, Barricarte A, Quiros JR, Johansson I, Johansson A, Berglund G, Bingham S, Khaw KT, Allen N, Key T, Carneiro F, Save V, Del Giudice G, Plebani M, Kaaks R, Gonzalez CA (2006a) Plasma and dietary carotenoid, retinol and tocopherol levels and the risk of gastric adenocarcinomas in the European prospective investigation into cancer and nutrition. Br J Cancer 95:406–415
Jenab M, Riboli E, Ferrari P, Sabate J, Slimani N, Norat T, Friesen M, Tjonneland A, Olsen A, Overvad K, Boutron-Ruault MC, Clavel-Chapelon F, Touvier M, Boeing H, Schulz M, Linseisen J, Nagel G, Trichopoulou A, Naska A, Oikonomou E, Krogh V, Panico S, Masala G, Sacerdote C, Tumino R, Peeters PH, Numans ME, Bueno-de-Mesquita HB, Buchner FL, Lund E, Pera G, Sanchez CN, Sanchez MJ, Arriola L, Barricarte A, Quiros JR, Hallmans G, Stenling R, Berglund G, Bingham S, Khaw KT, Key T, Allen N, Carneiro F, Mahlke U, Del Giudice G, Palli D, Kaaks R, Gonzalez CA (2006b) Plasma and dietary vitamin C levels and risk of gastric cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC-EURGAST). Carcinogenesis 27:2250–2257
Lahner E, Persechino S, Annibale B (2012) Micronutrients (Other than iron) and Helicobacter pylori infection: a systematic review. Helicobacter 17:1–15
Pal J, Sanal MG, Gopal GJ (2011) Vitamin-C as anti-Helicobacter pylori agent: more prophylactic than curative- Critical review. Indian J Pharmacol 43:624–627
Palli D, Masala G, Del Giudice G, Plebani M, Basso D, Berti D, Numans ME, Ceroti M, Peeters PH, Bueno de Mesquita HB, Buchner FL, Clavel-Chapelon F, Boutron-Ruault MC, Krogh V, Saieva C, Vineis P, Panico S, Tumino R, Nyren O, Siman H, Berglund G, Hallmans G, Sanchez MJ, Larranaga N, Barricarte A, Navarro C, Quiros JR, Key T, Allen N, Bingham S, Khaw KT, Boeing H, Weikert C, Linseisen J, Nagel G, Overvad K, Thomsen RW, Tjonneland A, Olsen A, Trichoupoulou A, Trichopoulos D, Arvaniti A, Pera G, Kaaks R, Jenab M, Ferrari P, Nesi G, Carneiro F, Riboli E, Gonzalez CA (2007) CagA + Helicobacter pylori infection and gastric cancer risk in the EPIC-EURGAST study. Int J Cancer 120:859–867
Peek RM Jr, Blaser MJ (2002) Helicobacter pylori and gastrointestinal tract adenocarcinomas. Nat Rev Cancer 2:28–37
Polk DB, Peek RM Jr (2010) Helicobacter pylori: gastric cancer and beyond. Nat Rev Cancer 10:403–414
Riboli E, Hunt KJ, Slimani N, Ferrari P, Norat T, Fahey M, Charrondiere UR, Hemon B, Casagrande C, Vignat J, Overvad K, Tjonneland A, Clavel-Chapelon F, Thiebaut A, Wahrendorf J, Boeing H, Trichopoulos D, Trichopoulou A, Vineis P, Palli D, Bueno-de-Mesquita HB, Peeters PH, Lund E, Engeset D, Gonzalez CA, Barricarte A, Berglund G, Hallmans G, Day NE, Key TJ, Kaaks R, Saracci R (2002) European Prospective Investigation into Cancer and Nutrition (EPIC): study populations and data collection. Public Health Nutr 5:1113–1124
Sala N, Munoz X, Travier N, Agudo A, Duell EJ, Moreno V, Overvad K, Tjonneland A, Boutron-Ruault MC, Clavel-Chapelon F, Canzian F, Kaaks R, Boeing H, Meidtner K, Trichopoulos A, Tsiotas K, Zylis D, Vineis P, Panico S, Palli D, Krogh V, Tumino R, Lund E, Bueno-de-Mesquita HB, Numans ME, Peeters PH, Quiros JR, Sanchez MJ, Navarro C, Ardanaz E, Dorronsoro M, Hallmans G, Stenling R, Manjer J, Allen NE, Travis RC, Khaw KT, Jenab M, Offerhaus GJ, Riboli E, Gonzalez CA (2012) Prostate stem-cell antigen gene is associated with diffuse and intestinal gastric cancer in Caucasians: results from the EPIC-EURGAST study. Int J Cancer 130:2417–2427
Sasazuki S, Hayashi T, Nakachi K, Sasaki S, Tsubono Y, Okubo S, Hayashi M, Tsugane S (2008) Protective effect of vitamin C on oxidative stress: a randomized controlled trial. Int J Vitam Nutr Res 78:121–128
Savini I, Rossi A, Pierro C, Avigliano L, Catani MV (2008) SVCT1 and SVCT2: key proteins for vitamin C uptake. Amino Acids 34:347–355
Skibola CF, Bracci PM, Halperin E, Nieters A, Hubbard A, Paynter RA, Skibola DR, Agana L, Becker N, Tressler P, Forrest MS, Sankararaman S, Conde L, Holly EA, Smith MT (2008) Polymorphisms in the estrogen receptor 1 and vitamin C and matrix metalloproteinase gene families are associated with susceptibility to lymphoma. PLoS ONE 3:e2816
Slimani N, Deharveng G, Unwin I, Southgate DA, Vignat J, Skeie G, Salvini S, Parpinel M, Moller A, Ireland J, Becker W, Farran A, Westenbrink S, Vasilopoulou E, Unwin J, Borgejordet A, Rohrmann S, Church S, Gnagnarella P, Casagrande C, van Bakel M, Niravong M, Boutron-Ruault MC, Stripp C, Tjonneland A, Trichopoulou A, Georga K, Nilsson S, Mattisson I, Ray J, Boeing H, Ocke M, Peeters PH, Jakszyn P, Amiano P, Engeset D, Lund E, de Magistris MS, Sacerdote C, Welch A, Bingham S, Subar AF, Riboli E (2007) The EPIC nutrient database project (ENDB): a first attempt to standardize nutrient databases across the 10 European countries participating in the EPIC study. Eur J Clin Nutr 61:1037–1056
Tannenbaum SR, Wishnok JS, Leaf CD (1991) Inhibition of nitrosamine formation by ascorbic acid. Am J Clin Nutr 53:247S–250S
Timpson NJ, Forouhi NG, Brion MJ, Harbord RM, Cook DG, Johnson P, McConnachie A, Morris RW, Rodriguez S, Luan J, Ebrahim S, Padmanabhan S, Watt G, Bruckdorfer KR, Wareham NJ, Whincup PH, Chanock S, Sattar N, Lawlor DA, Davey SG (2010) Genetic variation at the SLC23A1 locus is associated with circulating concentrations of l-ascorbic acid (vitamin C): evidence from 5 independent studies with > 15,000 participants. Am J Clin Nutr 92:375–382
Tsugane S, Sasazuki S (2007) Diet and the risk of gastric cancer: review of epidemiological evidence. Gastric Cancer 10:75–83
Tsukaguchi H, Tokui T, Mackenzie B, Berger UV, Chen XZ, Wang Y, Brubaker RF, Hediger MA (1999) A family of mammalian Na+-dependent L-ascorbic acid transporters. Nature 399:70–75
Vuilleumier J, Keck E (1989) Fluorometric assay of vitamin C in biological materials using a centrifugal analyser with fluorescence attachment. J Micronutr Anal 5:25–34
Wright ME, Andreotti G, Lissowska J, Yeager M, Zatonski W, Chanock SJ, Chow WH, Hou L (2009) Genetic variation in sodium-dependent ascorbic acid transporters and risk of gastric cancer in Poland. Eur J Cancer 45:1824–1830
Zhang HM, Wakisaka N, Maeda O, Yamamoto T (1997) Vitamin C inhibits the growth of a bacterial risk factor for gastric carcinoma: Helicobacter pylori. Cancer 80:1897–1903
Acknowledgments
The coordination of EPIC is financially supported by the European Commission (DG-SANCO) and the International Agency for Research on Cancer. The national cohorts are supported by the Health Research Fund (FIS) of the Spanish Ministry of Health (Exp P10710130), La Caixa (BM 06-130), RTICC-RD06/0020/0091, RTICC-RD12/0036/0018; Regional Governments of Andalucía, Asturias, Basque Country, Murcia (no. 6236), Navarra and the Catalan Institute of Oncology (Spain); Danish Cancer Society (Denmark); Ligue contre le Cancer, Institut Gustave Roussy, Mutuelle Générale de l’Education Nationale, Institut National de la Santé et de la Recherche Médicale (INSERM) (France); Deutsche Krebshilfe, Deutsches Krebsforschungszentrum and Federal Ministry of Education and Research (Germany); the Hellenic Health Foundation (Greece); Italian Association for Research on Cancer (AIRC) and National Research Council (Italy); Dutch Ministry of Public Health, Welfare and Sports (VWS), Netherlands Cancer Registry (NKR), LK Research Funds, Dutch Prevention Funds, Dutch ZON (Zorg Onderzoek Nederland), World Cancer Research Fund (WCRF) and Statistics Netherlands (The Netherlands); Swedish Cancer Society, Swedish Scientific Council and Regional Government of Skåne and Västerbotten (Sweden); Cancer Research UK, Medical Research Council (United Kingdom).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Duell, E.J., Lujan-Barroso, L., Llivina, C. et al. Vitamin C transporter gene (SLC23A1 and SLC23A2) polymorphisms, plasma vitamin C levels, and gastric cancer risk in the EPIC cohort. Genes Nutr 8, 549–560 (2013). https://doi.org/10.1007/s12263-013-0346-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12263-013-0346-6