Abstract
Background
Circadian rhythms play an important role in the regulation of eating and fasting, and mistimed dietary intakes may be detrimental to metabolic health. Extended overnight fasting has been proposed as a strategy to better align the eating-fasting cycle with the internal circadian clock, and both observational and experimental studies have linked longer overnight fasting with lower body weight. However, it remains unclear if the timing of overnight fasting modifies the relationship between fasting duration and weight outcomes.
Methods
The current study included 495 men and 499 women age 50–74 years. Dietary intake over 12 months was assessed by 24-h dietary recalls every two months, and body-mass index was measured at the beginning, middle and end of the study. Logistic regression was used to estimate the relationship between overnight fasting duration and the likelihood of being overweight or obesity adjusted for multiple confounders, and assessed whether the relationship was modified by the timing of overnight fasting, measured as the midpoint of the fasting period.
Results
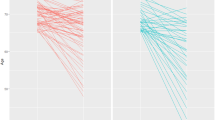
Among participants with early overnight fasting (midpoint < 02:19 am), a longer fasting duration was associated with lower odds of overweight and obesity; while among those with late fasting (≥02:19 am), longer fasting was associated with higher odds of overweight and obesity. Specifically, when compared to the shortest quintile of overnight fasting duration, the longest quintile was associated with a 53% reduction in the odds of overweight and obesity in the early fasting group (OR = 0.47, 95% CI = 0.23, 0.97), but a 2.36-fold increase in the late fasting group (OR = 3.36, 95% CI = 1.48, 7.62). Additionally adjusting for dietary intakes during morning and late evening periods did not affect the observed associations.
Conclusions
Longer overnight fasting was associated with a reduced likelihood of being overweight or obese, but only among those with an early timing of fasting.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Code availability
All programs used in this study for data analysis can be obtained by communicating with the corresponding author.
References
St-Onge MP, Ard J, Baskin ML, Chiuve SE, Johnson HM, Kris-Etherton P, et al. Meal timing and frequency: implications for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2017;135:e96–e121.
Kahleova H, Lloren JI, Mashchak A, Hill M, Fraser GE. Meal frequency and timing are associated with changes in body mass index in adventist health study 2. J Nutr. 2017;147:1722–8.
Marinac CR, Natarajan L, Sears DD, Gallo LC, Hartman SJ, Arredondo E, et al. Prolonged nightly fasting and breast cancer risk: findings from NHANES (2009–10). Cancer Epidemiol Biomarkers Prev. 2015;24:783–9.
Gill S, Panda S. A smartphone App reveals erratic diurnal eating patterns in humans that can be modulated for health benefits. Cell Metab. 2015;22:789–98.
Gabel K, Hoddy KK, Haggerty N, Song J, Kroeger CM, Trepanowski JF, et al. Effects of 8-hour time restricted feeding on body weight and metabolic disease risk factors in obese adults: a pilot study. Nutr Healthy Aging. 2018;4:345–53.
Anton SD, Lee SA, Donahoo WT, McLaren C, Manini T, Leeuwenburgh C et al. The effects of time restricted feeding on overweight, older adults: a pilot study. Nutrients. 2019;11:1500.
Arnason TG, Bowen MW, Mansell KD. Effects of intermittent fasting on health markers in those with type 2 diabetes: a pilot study. World J Diabetes. 2017;8:154–64.
Tinsley GM, La, Bounty PM. Effects of intermittent fasting on body composition and clinical health markers in humans. Nutr Rev. 2015;73:661–74.
Stote KS, Baer DJ, Spears K, Paul DR, Harris GK, Rumpler WV, et al. A controlled trial of reduced meal frequency without caloric restriction in healthy, normal-weight, middle-aged adults. Am J Clin Nutr. 2007;85:981–8.
Kesztyus D, Cermak P, Gulich M, Kesztyus T. Adherence to time-restricted feeding and impact on abdominal obesity in primary care patients: results of a pilot study in a pre-post design. Nutrients. 2019;31:11.
Wilkinson MJ, Manoogian ENC, Zadourian A, Lo H, Fakhouri S, Shoghi A, et al. Ten-hour time-restricted eating reduces weight, blood pressure, and atherogenic lipids in patients with metabolic syndrome. Cell Metab. 2020;31:92–104. e5.
McAllister MJ, Pigg BL, Renteria LI, Waldman HS. Time-restricted feeding improves markers of cardiometabolic health in physically active college-age men: a 4-week randomized pre-post pilot study. Nutr Res. 2020;75:32–43.
Antonini A, Gentile G, Giglio M, Marcante A, Gage H, Touray MML, et al. Acceptability to patients, carers and clinicians of an mHealth platform for the management of Parkinson’s disease (PD_Manager): study protocol for a pilot randomised controlled trial. Trials. 2018;19:492.
Guinter MA, Campbell PT, Patel AV, McCullough ML. Irregularity in breakfast consumption and daily meal timing patterns in association with body weight status and inflammation. Br J Nutr. 2019;122:1192–200.
Deshmukh-Taskar P, Nicklas TA, Radcliffe JD, O’Neil CE, Liu Y. The relationship of breakfast skipping and type of breakfast consumed with overweight/obesity, abdominal obesity, other cardiometabolic risk factors and the metabolic syndrome in young adults. The National Health and Nutrition Examination Survey (NHANES): 1999–2006. Public Health Nutr. 2013;16:2073–82.
van der Heijden AA, Hu FB, Rimm EB, van Dam RM. A prospective study of breakfast consumption and weight gain among U.S. men. Obesity. 2007;15:2463–9.
Xiao Q, Garaulet M, Scheer F. Meal timing and obesity: interactions with macronutrient intake and chronotype. Int J Obes. 2019;43:1701–11.
Berg C, Lappas G, Wolk A, Strandhagen E, Toren K, Rosengren A, et al. Eating patterns and portion size associated with obesity in a Swedish population. Appetite. 2009;52:21–6.
Baron KG, Reid KJ, Kern AS, Zee PC. Role of sleep timing in caloric intake and BMI. Obesity. 2011;19:1374–81.
Ruiz-Lozano T, Vidal J, de Hollanda A, Scheer F, Garaulet M, Izquierdo-Pulido M. Timing of food intake is associated with weight loss evolution in severe obese patients after bariatric surgery. Clin Nutr. 2016;35:1308–14.
Garaulet M, Gomez-Abellan P, Alburquerque-Bejar JJ, Lee YC, Ordovas JM, Scheer FA. Timing of food intake predicts weight loss effectiveness. Int J Obes. 2013;37:604–11.
Hutchison AT, Regmi P, Manoogian ENC, Fleischer JG, Wittert GA, Panda S, et al. Time-restricted feeding improves glucose tolerance in men at risk for type 2 diabetes: a randomized crossover trial. Obesity. 2019;27:724–32.
Lyden K, Keadle SK, Staudenmayer J, Freedson PS. The activPALTM accurately classifies activity intensity categories in healthy adults. Med Sci Sports Exerc. 2017;49:1022–8.
Pfister T, Matthews CE, Wang Q, Kopciuk KA, Courneya K, Friedenreich C. Comparison of two accelerometers for measuring physical activity and sedentary behaviour. BMJ Open Sport Exerc Med. 2017;3:e000227.
Breen N, Layne TM. Forty years of progress in monitoring cancer control. In: 2007 Proceedings of the Survey Research Methods Section, vol. 3901-10. VA: American Statistical Association Alexandria; 2007.
Marinac CR, Nelson SH, Breen CI, Hartman SJ, Natarajan L, Pierce JP, et al. Prolonged nightly fasting and breast cancer prognosis. JAMA Oncol. 2016;2:1049–55.
Irimie AI, Braicu C, Pasca S, Magdo L, Gulei D, Cojocneanu R, et al. Role of key micronutrients from nutrigenetic and nutrigenomic perspectives in cancer prevention. Medicina. 2019;55:283.
Jahrami HA, Alsibai J, Clark CCT, Faris MAE. A systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on body weight in healthy subjects aged 16 years and above. Eur J Nutr. 2020;59:2291–316.
Faris MA, Jahrami H, BaHammam A, Kalaji Z, Madkour M, Hassanein M. A systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on glucometabolic markers in healthy subjects. Diabetes Res Clin Pract. 2020;165:108226.
Faris MAE, Jahrami HA, Alsibai J, Obaideen AA. Impact of Ramadan diurnal intermittent fasting on metabolic syndrome components in healthy, non-athletic Muslim people aged over 15 years: a systematic review and meta-analysis. Br J Nutr. 2019;123:1–51.
Patterson RE, Sears DD. Metabolic effects of intermittent fasting. Annu Rev Nutr. 2017;37:371–93.
Hatori M, Vollmers C, Zarrinpar A, DiTacchio L, Bushong EA, Gill S, et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab. 2012;15:848–60.
Belkacemi L, Selselet-Attou G, Louchami K, Sener A, Malaisse WJ. Intermittent fasting modulation of the diabetic syndrome in sand rats. II. In vivo investigations. Int J Mol Med. 2010;26:759–65.
Chaix A, Zarrinpar A, Miu P, Panda S. Time-restricted feeding is a preventative and therapeutic intervention against diverse nutritional challenges. Cell Metab. 2014;20:991–1005.
Chaix A, Lin T, Le HD, Chang MW, Panda S. Time-restricted feeding prevents obesity and metabolic syndrome in mice lacking a circadian clock. Cell Metab. 2019;29:303–19. e4.
Chung H, Chou W, Sears DD, Patterson RE, Webster NJ, Ellies LG. Time-restricted feeding improves insulin resistance and hepatic steatosis in a mouse model of postmenopausal obesity. Metabolism. 2016;65:1743–54.
Sherman H, Genzer Y, Cohen R, Chapnik N, Madar Z, Froy O. Timed high-fat diet resets circadian metabolism and prevents obesity. FASEB J. 2012;26:3493–502.
Paoli A, Tinsley G, Bianco A, Moro T. The influence of meal frequency and timing on health in humans: the role of fasting. Nutrients. 2019;11:719.
Salgado-Delgado R, Angeles-Castellanos M, Saderi N, Buijs RM, Escobar C. Food intake during the normal activity phase prevents obesity and circadian desynchrony in a rat model of night work. Endocrinology. 2010;151:1019–29.
Proper KI, van de Langenberg D, Rodenburg W, Vermeulen RCH, van der Beek AJ, van Steeg H, et al. The relationship between shift work and metabolic risk factors: a systematic review of longitudinal studies. Am J Prev Med. 2016;50:e147–e157.
Horikawa C, Kodama S, Yachi Y, Heianza Y, Hirasawa R, Ibe Y, et al. Skipping breakfast and prevalence of overweight and obesity in Asian and Pacific regions: a meta-analysis. Prev Med. 2011;53:260–7.
Kutsuma A, Nakajima K, Suwa K. Potential association between breakfast skipping and concomitant late-night-dinner eating with metabolic syndrome and proteinuria in the Japanese population. Scientifica. 2014;2014:253581.
Wang JB, Patterson RE, Ang A, Emond JA, Shetty N, Arab L. Timing of energy intake during the day is associated with the risk of obesity in adults. J Hum Nutr Diet. 2014;27(Suppl 2):255–62.
Baron KG, Reid KJ, Horn LV, Zee PC. Contribution of evening macronutrient intake to total caloric intake and body mass index. Appetite. 2013;60:246–51.
Panda S. Circadian physiology of metabolism. Science. 2016;354:1008–15.
Asher G, Sassone-Corsi P. Time for food: the intimate interplay between nutrition, metabolism, and the circadian clock. Cell. 2015;161:84–92.
Mukherji A, Kobiita A, Damara M, Misra N, Meziane H, Champy MF, et al. Shifting eating to the circadian rest phase misaligns the peripheral clocks with the master SCN clock and leads to a metabolic syndrome. Proc Natl Acad Sci USA. 2015;112:E6691–8.
Mayeuf-Louchart A, Zecchin M, Staels B, Duez H. Circadian control of metabolism and pathological consequences of clock perturbations. Biochimie. 2017;143:42–50.
Madkour MI, A TE-S, Jahrami HA, Sherif NM, Hassan RE, Awadallah S, et al. Ramadan diurnal intermittent fasting modulates SOD2, TFAM, Nrf2, and sirtuins (SIRT1, SIRT3) gene expressions in subjects with overweight and obesity. Diabetes Res Clin Pract. 2019;155:107801.
Duffy JF, Dijk DJ, Hall EF, Czeisler CA. Relationship of endogenous circadian melatonin and temperature rhythms to self-reported preference for morning or evening activity in young and older people. J Investig Med. 1999;47:141–50.
Beccuti G, Pannain S. Sleep and obesity. Curr Opin Clin Nutr Metab Care. 2011;14:402–12.
Gonnissen HK, Adam TC, Hursel R, Rutters F, Verhoef SP, Westerterp-Plantenga MS. Sleep duration, sleep quality and body weight: parallel developments. Physiol Behav. 2013;121:112–6.
Chaput JP. Sleep patterns, diet quality and energy balance. Physiol Behav. 2014;134:86–91.
Kant AK, Graubard BI. Within-person comparison of eating behaviors, time of eating, and dietary intake on days with and without breakfast: NHANES 2005-10. Am J Clin Nutr. 2015;102:661–70.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Xiao, Q., Bauer, C., Layne, T. et al. The association between overnight fasting and body mass index in older adults: the interaction between duration and timing. Int J Obes 45, 555–564 (2021). https://doi.org/10.1038/s41366-020-00715-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-00715-z
This article is cited by
-
Is time of eating associated with BMI and obesity? A population-based study
European Journal of Nutrition (2024)
-
Association of meal timing with body composition and cardiometabolic risk factors in young adults
European Journal of Nutrition (2023)
-
Effect of a six-week times restricted eating intervention on the body composition in early elderly men with overweight
Scientific Reports (2022)