Abstract
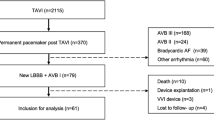
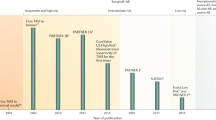
Transcatheter aortic valve implantation (TAVI) is increasingly used to treat patients with aortic stenosis who are considered to be too high-risk for surgical replacement of the aortic valve. Although the procedural risks are decreasing, the occurrence of new conduction abnormalities remains a vexing issue. Both left bundle branch block and atrioventricular dissociation can affect prognosis after TAVI. Understanding the intimate relationship between the atrioventricular conduction axis and the aortic root, in addition to elucidation of factors related specifically to the procedure, devices, and patients, might help to reduce these conduction abnormalities. The purpose of this Review is to assess, and offer insights into, the available information on the frequency of new conduction abnormalities associated with TAVI, their anatomical and procedural causes, and their clinical consequences.
Key Points
-
Transcatheter aortic valve implantation (TAVI) is increasingly used to treat patients with aortic stenosis who are considered to be too high-risk for surgical replacement of the aortic valve
-
Although the procedural risks are decreasing, the occurrence of new conduction abnormalities after TAVI remains a major issue
-
The aggregate of information concerning potential predictors is growing, but a comprehensive overview of these factors is still lacking
-
Knowledge of the intimate relationship and proximity of the atrioventricular conduction axis with the aortic root allows us to understand the pathological mechanisms underlying new conduction abnormalities after TAVI
-
Appreciation of factors related specifically to the devices, procedure, and patients makes it possible to predict the occurrence of new conduction abnormalities, and might change the procedure and devices
-
Information concerning the effects of new conduction abnormalities and new implantation of permanent pacemakers on long-term follow-up is scarce and should be further elucidated
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Andersen, H. R., Knudsen, L. L. & Hasenkam, J. M. Transluminal implantation of artificial heart valves. Description of a new expandable aortic valve and initial results with implantation by catheter technique in closed chest pigs. Eur. Heart J. 13, 704–708 (1992).
Cribier, A. et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description. Circulation 106, 3006–3008 (2002).
Rodés-Cabau, J. et al. Transcatheter aortic valve implantation for the treatment of severe symptomatic aortic stenosis in patients at very high or prohibitive surgical risk: acute and late outcomes of the multicenter Canadian experience. J. Am. Coll. Cardiol. 55, 1080–1090 (2010).
Piazza, N. et al. Procedural and 30-day outcomes following transcatheter aortic valve implantation using the third generation (18 Fr) CoreValve revalving system: results from the multicentre, expanded evaluation registry 1-year following CE mark approval. EuroIntervention 4, 242–249 (2008).
Tamburino, C. et al. Incidence and predictors of early and late mortality after transcatheter aortic valve implantation in 663 patients with severe aortic stenosis. Circulation 123, 299–308 (2011).
Eltchaninoff, H. et al. Transcatheter aortic valve implantation: early results of the FRANCE (FRench Aortic National CoreValve and Edwards) registry. Eur. Heart J. 32, 191–197 (2011).
Zahn, R. et al. Transcatheter aortic valve implantation: first results from a multi-centre real-world registry. Eur. Heart J. 32, 198–204 (2011).
Lefèvre, T. et al. One year follow-up of the multi-centre European PARTNER transcatheter heart valve study. Eur. Heart J. 32, 148–157 (2011).
Bosmans, J. M. et al. Procedural, 30-day and one year outcome following CoreValve or Edwards transcatheter aortic valve implantation: results of the Belgian national registry. Interact. Cardiovasc. Thorac. Surg. 12, 762–767 (2011).
Moat, N. E. et al. Long-term outcomes after transcatheter aortic valve implantation in high-risk patients with severe aortic stenosis: the U. K. TAVI (United Kingdom Transcatheter Aortic Valve Implantation) Registry. J. Am. Coll. Cardiol. 58, 2130–2138 (2011).
Thomas, M. et al. One-year outcomes of cohort 1 in the Edwards SAPIEN Aortic Bioprosthesis European Outcome (SOURCE) registry: the European registry of transcatheter aortic valve implantation using the Edwards SAPIEN valve. Circulation 124, 425–433 (2011).
Leon, M. B. et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N. Engl. J. Med. 363, 1597–1607 (2010).
Smith, C. R. et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N. Engl. J. Med. 364, 2187–2198 (2011).
de Jaegere, P. P. T. et al. Transcatheter aortic valve implantation. Where are we? EuroIntervention 5, 169–171 (2009).
Rodés-Cabau, J. Transcatheter aortic valve implantation: current and future approaches. Nat. Rev. Cardiol. 9, 15–29 (2011).
Grines, C. L. et al. Functional abnormalities in isolated left bundle branch block. The effect of interventricular asynchrony. Circulation 79, 845–853 (1989).
Lee, S.-J. et al. Isolated bundle branch block and left ventricular dysfunction. J. Card. Fail. 9, 87–92 (2003).
Vernooy, K. et al. Left bundle branch block induces ventricular remodelling and functional septal hypoperfusion. Eur. Heart J. 26, 91–98 (2005).
Zannad, F. et al. Left bundle branch block as a risk factor for progression to heart failure. Eur. J. Heart Fail. 9, 7–14 (2007).
El-Khally, Z. et al. Prognostic significance of newly acquired bundle branch block after aortic valve replacement. Am. J. Cardiol. 94, 1008–1011 (2004).
Dawkins, S. et al. Permanent pacemaker implantation after isolated aortic valve replacement: incidence, indications, and predictors. Ann. Thorac. Surg. 85, 108–112 (2008).
Dimarakis, I. et al. Conventional aortic valve replacement for high-risk aortic stenosis patients not suitable for trans-catheter aortic valve implantation: feasibility and outcome. Eur. J. Cardiothorac. Surg. 40, 743–748 (2011).
Erdogan, H. B. et al. Risk factors for requirement of permanent pacemaker implantation after aortic valve replacement. J. Card. Surg. 21, 211–215 (2006).
Gordon, R. S., Ivanov, J., Cohen, G. & Ralph-Edwards, A. L. Permanent cardiac pacing after a cardiac operation: predicting the use of permanent pacemakers. Ann. Thorac. Surg. 66, 1698–1704 (1998).
Huynh, H. et al. Permanent pacemaker implantation following aortic valve replacement: current prevalence and clinical predictors. Pacing Clin. Electrophysiol. 32, 1520–1525 (2009).
Limongelli, G. et al. Risk factors for pacemaker implantation following aortic valve replacement: a single centre experience. Heart 89, 901–904 (2003).
Nardi, P. et al. Permanent pacemaker implantation after isolated aortic valve replacement: incidence, risk factors and surgical technical aspects. J. Cardiovasc. Med. (Hagerstown) 11, 14–19 (2010).
Schurr, U. P. et al. Incidence and risk factors for pacemaker implantation following aortic valve replacement. Interact. Cardiovasc. Thorac. Surg. 11, 556–560 (2010).
Bates, M. G. D., Matthews, I. G., Fazal, I. A. & Turley, A. J. Postoperative permanent pacemaker implantation in patients undergoing trans-catheter aortic valve implantation: what is the incidence and are there any predicting factors? Interact. Cardiovasc. Thorac. Surg. 12, 243–253 (2011).
Bagur, R. et al. Permanent pacemaker implantation following isolated aortic valve replacement in a large cohort of elderly patients with severe aortic stenosis. Heart 97, 1687–1694 (2011).
Reynolds, M. R. et al. Health-related quality of life after transcatheter aortic valve replacement in inoperable patients with severe aortic stenosis. Circulation 124, 1964–1972 (2011).
Georgiadou, P. et al. Long-term quality of life improvement after transcatheter aortic valve implantation. Am. Heart J. 162, 232–237 (2011).
Ussia, G. P. et al. Quality-of-life in elderly patients one year after transcatheter aortic valve implantation for severe aortic stenosis. EuroIntervention 7, 573–579 (2011).
Ussia, G. P. et al. Quality of life assessment after percutaneous aortic valve implantation. Eur. Heart J. 30, 1790–1796 (2009).
Gonçalves, A. et al. Quality of life improvement at midterm follow-up after transcatheter aortic valve implantation. Int. J. Cardiol. http://dx.doi.org/10.1016/j.ijcard.2011.05.050.
Bekeredjian, R. et al. Usefulness of percutaneous aortic valve implantation to improve quality of life in patients >80 years of age. Am. J. Cardiol. 106, 1777–1781 (2010).
Melek, M. et al. Tissue Doppler evaluation of intraventricular asynchrony in isolated left bundle branch block. Echocardiography 23, 120–126 (2006).
Abe, H. et al. Effects of aortic valve replacement on left ventricular dyssynchrony in aortic stenosis with narrow QRS complex. J. Am. Soc. Echocardiogr. 24, 1358–1364 (2011).
Heyndrickx, G. R., Vilaine, J. P., Knight, D. R. & Vatner, S. F. Effects of altered site of electrical activation on myocardial performance during inotropic stimulation. Circulation 71, 1010–1016 (1985).
Tzikas, A. et al. Frequency of conduction abnormalities after transcatheter aortic valve implantation with the Medtronic-CoreValve and the effect on left ventricular ejection fraction. Am. J. Cardiol. 107, 285–289 (2011).
Thomas, J. L. et al. Prognostic significance of the development of left bundle conduction defects following aortic valve replacement. J. Thorac. Cardiovasc. Surg. 84, 382–386 (1982).
Moreno, R. et al. Cause of complete atrioventricular block after percutaneous aortic valve implantation: insights from a necropsy study. Circulation 120, e29–e30 (2009).
Anderson, R. H., Razavi, R. & Taylor, A. M. Cardiac anatomy revisited. J. Anat. 205, 159–177 (2004).
Abuin, G. & Nieponice, A. The first septal artery supplies the atrioventricular node. Tex. Heart Inst. J. 25, 318–319 (1998).
Abuin, G. & Nieponice, A. New findings on the origin of the blood supply to the atrioventricular node. Clinical and surgical significance. Tex. Heart Inst. J. 25, 113–117 (1998).
von Lüdinghausen, M. & Ohmachi, N. Right superior septal artery with 'normal' right coronary and ectopic 'early' aortic origin: a contribution to the vascular supply of the interventricular septum of the human heart. Clin. Anat. 14, 312–319 (2001).
Taylor, J. R. The descending septal artery. Its relation to the conduction system of the heart. Arch. Pathol. Lab. Med. 104, 599–602 (1980).
Nuis, R.-J. et al. Timing and potential mechanisms of new conduction abnormalities during the implantation of the Medtronic CoreValve System in patients with aortic stenosis. Eur. Heart J. 32, 2067–2074 (2011).
Piazza, N. et al. Early and persistent intraventricular conduction abnormalities and requirements for pacemaking after percutaneous replacement of the aortic valve. JACC Cardiovasc. Interv. 1, 310–316 (2008).
Baan, J. Jr et al. Factors associated with cardiac conduction disorders and permanent pacemaker implantation after percutaneous aortic valve implantation with the CoreValve prosthesis. Am. Heart J. 159, 497–503 (2010).
Piazza, N. et al. Persistent conduction abnormalities and requirements for pacemaking six months after transcatheter aortic valve implantation. EuroIntervention 6, 475–484 (2010).
Aktug, O. et al. Incidence and predictors of left bundle branch block after transcatheter aortic valve implantation. Int. J. Cardiol. http://dx.doi.org/10.1016/j.ijcard.2011.03.004.
Ferreira, N. D. et al. Incidence and predictors of permanent pacemaker requirement after transcatheter aortic valve implantation with a self-expanding bioprosthesis. Pacing Clin. Electrophysiol. 33, 1364–1372 (2010).
Fraccaro, C. et al. Incidence, predictors, and outcome of conduction disorders after transcatheter self-expandable aortic valve implantation. Am. J. Cardiol. 107, 747–754 (2011).
Guetta, V. et al. Predictors and course of high-degree atrioventricular block after transcatheter aortic valve implantation using the CoreValve revalving system. Am. J. Cardiol. 108, 1600–1605 (2011).
Saia, F. et al. Transcatheter aortic valve implantation with a self-expanding nitinol bioprosthesis: Prediction of the need for permanent pacemaker using simple baseline and procedural characteristics. Catheter. Cardiovasc. Interv. 79, 712–719 (2012).
Gutiérrez, M. et al. Electrocardiographic changes and clinical outcomes after transapical aortic valve implantation. Am. Heart J. 158, 302–308 (2009).
Onalan, O. et al. Determinants of pacemaker dependency after coronary and/or mitral or aortic valve surgery with long-term follow-up. Am. J. Cardiol. 101, 203–208 (2008).
Merin, O. et al. Permanent pacemaker implantation following cardiac surgery: indications and long-term follow-up. Pacing Clin. Electrophysiol. 32, 7–12 (2009).
Erkapic, D. et al. Electrocardiographic and further predictors for permanent pacemaker requirement after transcatheter aortic valve implantation. Europace 12, 1188–1190 (2010).
Koos, R. et al. Electrocardiographic and imaging predictors for permanent pacemaker requirement after transcatheter aortic valve implantation. J. Heart Valve Dis. 20, 83–90 (2011).
Roten, L. et al. Incidence and predictors of atrioventricular conduction impairment after transcatheter aortic valve implantation. Am. J. Cardiol. 106, 1473–1480 (2010).
Calvi, V. et al. Incidence rate and predictors of permanent pacemaker implantation after transcatheter aortic valve implantation with self-expanding CoreValve prosthesis. J. Interv. Card. Electrophysiol. http://dx.doi.org/10.1007/s10840-011-9634-5.
Mack, M. Fool me once, shame on you; fool me twice, shame on me! A perspective on the emerging world of percutaneous heart valve therapy. J. Thorac. Cardiovasc. Surg. 136, 816–819 (2008).
Lange, R. et al. Improvements in transcatheter aortic valve implantation outcomes in lower surgical risk patients: a glimpse into the future. J. Am. Coll. Cardiol. 59, 280–287 (2012).
Tamburino, C. et al. Early- and mid-term outcomes of transcatheter aortic valve implantation in patients with logistic EuroSCORE less than 20%: a comparative analysis between different risk strata. Cathet. Cardiovasc. Interv. 79, 132–140 (2012).
Taylor, J. The time has come for a SYNTAX-like trial for transcatheter aortic valve implantation. Eur. Heart J. 32, 128–129 (2011).
Grube, E. et al. Feasibility of transcatheter aortic valve implantation without balloon pre-dilation: a pilot study. JACC Cardiovasc. Interv. 4, 751–757 (2011).
Tzikas, A., Schultz, C., Van Mieghem, N. M., de Jaegere, P. P. T. & Serruys, P. W. Optimal projection estimation for transcatheter aortic valve implantation based on contrast-aortography: validation of a prototype software. Catheter. Cardiovasc. Interv. 76, 602–607 (2010).
Dvir, D. & Kornowski, R. Percutaneous aortic valve implantation using novel imaging guidance. Catheter. Cardiovasc. Interv. 76, 450–454 (2010).
Sarkar, K., Ussia, G. P. & Tamburino, C. Transcatheter aortic valve implantation for severe aortic regurgitation in a stentless bioprosthetic valve with the CoreValve revalving system—technical tips and role of the Accutrak system. Catheter. Cardiovasc. Interv. 78, 485–490 (2011).
Schofer, J. et al. Retrograde transarterial implantation of a nonmetallic aortic valve prosthesis in high-surgical-risk patients with severe aortic stenosis: a first-in-man feasibility and safety study. Circ. Cardiovasc. Interv. 1, 126–133 (2008).
Treede, H. et al. Six-month results of a repositionable and retrievable pericardial valve for transcatheter aortic valve replacement: the Direct Flow Medical aortic valve. J. Thorac. Cardiovasc. Surg. 140, 897–903 (2010).
Gaia, D. F. et al. Transapical aortic valve implantation: results of a Brazilian prosthesis. Rev. Bras. Cir. Cardiovasc. 25, 293–302 (2010).
Gaia, D. F. et al. Off-pump transapical balloon-expandable aortic valve endoprosthesis implantation. Rev. Bras. Cir. Cardiovasc. 24, 233–238 (2009).
Kempfert, J. et al. Trans-apical aortic valve implantation using a new self-expandable bioprosthesis: initial outcomes. Eur. J. Cardiothorac. Surg. 40, 1114–1119 (2011).
Kempfert, J., Rastan, A. J., Mohr, F.-W. & Walther, T. A new self-expanding transcatheter aortic valve for transapical implantation—first in man implantation of the JenaValve™. Eur. J. Cardiothorac. Surg. 40, 761–763 (2011).
Buellesfeld, L., Gerckens, U. & Grube, E. Percutaneous implantation of the first repositionable aortic valve prosthesis in a patient with severe aortic stenosis. Catheter. Cardiovasc. Interv. 71, 579–584 (2008).
Falk, V. et al. New anatomically oriented transapical aortic valve implantation. Ann. Thorac. Surg. 87, 925–926 (2009).
Falk, V. et al. Transapical aortic valve implantation with a self-expanding anatomically oriented valve. Eur. Heart J. 32, 878–887 (2011).
Cribier, A. et al. Treatment of calcific aortic stenosis with the percutaneous heart valve: mid-term follow-up from the initial feasibility studies: the French experience. J. Am. Coll. Cardiol. 47, 1214–1223 (2006).
Walther, T. et al. Transapical minimally invasive aortic valve implantation; the initial 50 patients. Eur. J. Cardiothorac. Surg. 33, 983–988 (2008).
Sinhal, A. et al. Atrioventricular block after transcatheter balloon expandable aortic valve implantation. JACC Cardiovasc. Interv. 1, 305–309 (2008).
Webb, J. G. et al. Transcatheter aortic valve implantation: impact on clinical and valve-related outcomes. Circulation 119, 3009–3016 (2009).
Godin, M. et al. Frequency of conduction disturbances after transcatheter implantation of an Edwards Sapien aortic valve prosthesis. Am. J. Cardiol. 106, 707–712 (2010).
D'Ancona, G., Pasic, M., Unbehaun, A. & Hetzer, R. Permanent pacemaker implantation after transapical transcatheter aortic valve implantation. Interact. Cardiovasc. Thorac. Surg. 13, 373–376 (2011).
Bleiziffer, S. et al. Predictors for new-onset complete heart block after transcatheter aortic valve implantation. JACC Cardiovasc. Interv. 3, 524–530 (2010).
Berry, C. et al. Novel therapeutic aspects of percutaneous aortic valve replacement with the 21F CoreValve revalving system. Catheter. Cardiovasc. Interv. 70, 610–616 (2007).
Calvi, V. et al. Early conduction disorders following percutaneous aortic valve replacement. Pacing Clin. Electrophysiol. 32 (Suppl. 1), S126–S130 (2009).
Jilaihawi, H. et al. Predictors for permanent pacemaker requirement after transcatheter aortic valve implantation with the CoreValve bioprosthesis. Am. Heart J. 157, 860–866 (2009).
Latsios, G. et al. 'Device landing zone' calcification, assessed by MSCT, as a predictive factor for pacemaker implantation after TAVI. Catheter. Cardiovasc. Interv. 76, 431–439 (2010).
Haworth, P. et al. Predictors for permanent pacing after transcatheter aortic valve implantation. Catheter. Cardiovasc. Interv. 76, 751–756 (2010).
Rubín, J. M. et al. Atrioventricular conduction disturbance characterization in transcatheter aortic valve implantation with the CoreValve prosthesis. Circ. Cardiovasc. Interv. 4, 280–286 (2011).
Khawaja, M. Z. et al. Permanent pacemaker insertion after CoreValve transcatheter aortic valve implantation: incidence and contributing factors (the UK CoreValve Collaborative). Circulation 123, 951–960 (2011).
Author information
Authors and Affiliations
Contributions
R. M. van der Boon and R.-J. Nuis researched the data for the article, and all the authors contributed substantially to discussion of its content. R. M. van der Boon, R.-J. Nuis, R. H. Anderson, and P. P. T. de Jaegere wrote the article, and all the authors reviewed or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
J. Rodés Cabau is, or has been, a consultant for Edwards Lifesciences and St Jude Medical. P. P. T. de Jaegere is, or has been, a consultant for Medtronic. The other authors declare no competing interests.
Rights and permissions
About this article
Cite this article
van der Boon, R., Nuis, RJ., Van Mieghem, N. et al. New conduction abnormalities after TAVI—frequency and causes. Nat Rev Cardiol 9, 454–463 (2012). https://doi.org/10.1038/nrcardio.2012.58
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2012.58
This article is cited by
-
Predictors for new-onset conduction block in patients with pure native aortic regurgitation after transcatheter aortic valve replacement with a new-generation self-expanding valve (VitaFlow Liberty™): a retrospective cohort study
BMC Cardiovascular Disorders (2024)
-
Comparison of outcomes of self-expanding versus balloon-expandable valves for transcatheter aortic valve replacement: a meta-analysis of randomized and propensity-matched studies
BMC Cardiovascular Disorders (2023)
-
Changes in demographics, treatment and outcomes in a consecutive cohort who underwent transcatheter aortic valve implantation between 2005 and 2020
Netherlands Heart Journal (2022)
-
A Disruptive Technology: Determining Need for Permanent Pacing After TAVR
Current Cardiology Reports (2021)
-
Predictive Model for Thrombus Formation After Transcatheter Valve Replacement
Cardiovascular Engineering and Technology (2021)