Abstract
Study Design:
Retrospective data analysis.
Objectives:
To determine prevalence of orthostatic hypotension (OH) in patients with spinal cord injury (SCI) during the acute rehabilitation period.
Setting:
Quaternary care spinal unit, Vancouver General Hospital, British Columbia, Canada
Methods:
Eighty-nine patients with acute SCI stratified by neurological level (cervical, 55 (62%); upper thoracic, 12 (13%); lower thoracic, 22 (25%)), and graded by American Spinal Injury Association standards. Non-invasive measurement of systolic and diastolic blood pressure and heart rate were made at baseline and 3 min following an orthostatic challenge test administered during the first month after SCI.
Results:
Patients with cervical or upper thoracic motor complete SCI more frequently experienced OH (P<0.01). OH persisted during the first month following SCI in 74% of cervical and only 20% of upper thoracic motor complete SCI patients.
Conclusion:
Patients with cervical and upper thoracic motor complete SCI are more likely to experience persistent OH than those with lower level or motor incomplete SCI during the first month of rehabilitation.
Similar content being viewed by others
Introduction
A common consequence of spinal cord injury (SCI) is the loss of normal cardiovascular regulation, which often requires immediate medical intervention.1 During the initial few hours after SCI, particularly following a cervical injury, severe hypotension and persistent bradycardia may be observed as the hallmarks of neurogenic shock.2 As spinal reflexes reappear and spinal shock subsides, cardiovascular control may continue to be severely disrupted as a result of an imbalance between the sympathetic and parasympathetic nervous systems.3 Clinical measurements of baseline cardiovascular parameters often reveal further blood pressure drops during orthostatic challenge tests, reflecting the presence of orthostatic hypotension (OH).
These cardiovascular disturbances may significantly complicate and/or delay the rehabilitation of individuals with SCI.4 In turn, immobility may contribute to complications such as pressure ulcers, contractures, and pneumonia. Furthermore, Cariga et al.5 showed that there is a high prevalence of neck pain in SCI individuals with OH that significantly delayed their rehabilitation. All these factors lead to prolonged bed rest, which increases the likelihood of OH. El Masry6 has suggested that OH can even lead to neurological deterioration in individuals who may otherwise have a stable SCI. These potential delays in rehabilitation and the development of a variety of complications provide a compelling rationale for the early identification and management of OH in this population.
The purpose of this study was to retrospectively evaluate the prevalence and severity of OH in a sample of individuals undergoing inpatient rehabilitation during the first month following SCI. We also compared changes in baseline cardiovascular parameters in individuals with varying severities of SCI.
Materials and methods
The protocol for this study was approved by the Clinical Research Ethics Board of the University of British Columbia and the Vancouver Coastal Health Authority. We conducted a retrospective chart analysis of all patients with acute traumatic SCI admitted to the Acute Spinal Cord Injury Unit at Vancouver General Hospital for a period of 1 year (1 January to 31 December 2004).
Data collection procedure
The following information was retrieved from the clinical charts: demographic data (age, gender, cause and date of injury), clinical data regarding the injury (cause, level and grade of injury) and medical and surgical management (surgery, days before mobilization and use of midodrine), data on grade and level of SCI, and cardiovascular parameters (heart rate (HR) and blood pressure) at different times during the first month of rehabilitation. The level and grade of SCI were evaluated using the international standards for neurological classification by American Spinal Injury Association (ASIA) on admission to the hospital and 30 days after admission.7 Data were collected and entered into a previously designed database.
Study groups
The patients were divided into three groups according to level of SCI: cervical (C2–C8), upper thoracic (T1–T6) and lower thoracic and lumbar, referred to as lower thoracic (T7–L2). The division of the groups into upper and lower thoracic was based on previous clinical observations of cardiovascular disturbances in this population.8, 9, 10 The patients were further divided on the basis of SCI grade into two subgroups: motor complete (ASIA A and B) and motor incomplete (ASIA C and D). Neurological recovery was defined on the basis of improvement in ASIA impairment scale.
Cardiovascular parameters and OH criterion
Baseline cardiovascular parameters (systolic and diastolic blood pressure, and HR) were retrieved from chart records on admission to Vancouver General Hospital and weekly thereafter for the first month of acute rehabilitation. Parameters reported only during the morning assessment of vital signs (supine position) were collected for this part of the study.
The orthostatic challenge test was performed by nurses or physiotherapists on the unit to determine the presence of OH. This test consists of an initial assessment of blood pressure and HR while supine (at rest), and then a repeat assessment of blood pressure and HR following 3 min of sitting up in bed or in a wheelchair. OH was defined as a decrease in systolic blood pressure of 20 mm Hg or greater, or a decrease in diastolic blood pressure of 10 mm Hg or greater, in accordance with the criteria established by the American Autonomic Society and the American Academy of Neurology.11 The results of the orthostatic challenge test on day 7 after admission and weekly thereafter for the first month of acute rehabilitation were recorded for this study. None of the individuals in this study received midodrine during the first month following injury
Statistical analysis
Analysis was performed using Microsoft Excel and Sigma Plot 2001 for Windows. Categorical variables (gender and cause of injury) were statistically analyzed using a χ2 analysis. Multiple group comparisons were performed for interval variables (blood pressure and HR) using analysis of variance-single factor statistics. Further analysis was performed using a paired or two-sample Student's t-test. Significance was set at P<0.05. Range intervals represent s.e.m.
Results
Study group and grade of SCI
A total of 89 individuals (72 (81%) men and 17 (29%) women) with acute SCI (average age, 43.0±1.98 years old) admitted to the Acute Spinal Cord Injury Unit within a 1-year period were included in the study (Table 1). Motor vehicle accidents were the major causes of SCI in our study sample (44%), followed by falls (29%) and sport-related injuries (17%). The majority of patients (62%) sustained cervical SCI, followed by lower thoracic (25%) and thoracic (13%) injuries. The most common cord injury was at the C5 level, seen in 20 (22%) cases. The average age of patients in the cervical, upper thoracic and lower thoracic groups was 46±2.44, 43±6.32, and 35±3.45 years, respectively (P=0.06). Time between SCI and admission to our center varied from 1 to 7 days.
On admission, 46 (52%) subjects presented with ASIA A, 14 (16%) with ASIA B, 11 (12%) with ASIA C and 18 (20%) with ASIA D SCI. Ninety-four percent of the patients underwent surgical decompression with stabilization. At the end of the first month following SCI injury, partial recovery occurred in 9% of the individuals.
Baseline cardiovascular parameters
On admission, there were no statistically significant differences in the baseline systolic (P=0.08) and diastolic (P=0.12) blood pressure values in individuals with cervical, upper and lower thoracic SCI. The trend, however, persisted up to the end of the first month following SCI.
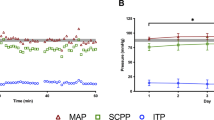
Further comparison of baseline cardiovascular parameters was conducted on the basis of grade of injury in patients with motor complete and incomplete SCI. For patients with motor complete SCI, systolic blood pressure on admission was significantly lower in the cervical SCI group (107±2.3 mm Hg), than in the upper thoracic (125±6.6 mm Hg; P=0.02) and lower thoracic SCI (119±2.8 mm Hg; P<0.01) groups. This trend persisted up to the end of the first month of rehabilitation (Figure 1). However, for patients with motor incomplete SCI, there was no difference in systolic blood pressure on admission (P=0.48) and at the end of the first month of rehabilitation (P=0.25) among the three groups (Figure 1).
We did not observe a difference in diastolic blood pressure among the cervical, upper and lower thoracic SCI subgroups during the first month of rehabilitation in either the motor complete or motor incomplete SCI groups (Figure 2).
The HR on admission was significantly lower in the cervical (68±1.7 beats/min), than in the upper thoracic (91±4.4 beats/min; P<0.01) and the lower thoracic (98±4.9 beats/min; P<0.01) SCI groups, regardless of whether these patients had motor complete or motor incomplete SCI. However, these differences disappeared by the end of the first month of rehabilitation (P=0.08).
OH
Overall, 53 of 89 (60%) patients developed OH during the first month following SCI. Eleven were women representing 65% of the female cohort, and 42 were men representing 58% of the male cohort. This difference was not significant (P=0.89). We did not observe a difference in the development of OH among the various age groups in our study (P=0.70) (Table 1). OH was significantly more common in cervical and upper thoracic patients than it was in lower thoracic SCI individuals (P<0.01). We found no difference in prevalence of OH between cervical and upper thoracic patients (P=0.50) (Table 2).
In this study, OH did improve over time for individuals with all levels of SCI; however, the pattern of improvement was different in the different groups. By the end of the first month, only those cervical and upper thoracic patients with motor complete SCI had ongoing episodes of OH. Patients with cervical motor complete SCI experienced OH more than patients with other levels of injury (Table 2).
Discussion
This study shows that cardiovascular disturbances are common during the acute and subacute rehabilitation period following traumatic SCI. We have found that 60% of individuals with SCI exhibit evidence of OH during early rehabilitation. Low resting blood pressure and OH were predominantly observed in patients with cervical and upper thoracic motor complete SCI. In general, OH improved during the first month of rehabilitation. In patients with motor complete cervical or upper thoracic SCI, OH persisted until the end of the first month of their rehabilitation, suggesting significant impairment in cardiovascular autonomic control.
Demographic findings
In general, the demographic characteristics of our patient population were consistent with previous reports on acute traumatic SCI. In our study, the majority of SCI occurred in men (79%), motor vehicle accidents were the most common cause of SCI, and the majority of injuries occurred in the cervical spinal cord with C5 being the most common level.12
Cardiovascular parameters in acute rehabilitation following SCI
Initial comparison of baseline (supine) cardiovascular parameters did not reveal any differences in the systolic and diastolic blood pressure for patients with cervical or different levels of thoracic SCI at the time of admission. However, substantial differences in baseline cardiovascular parameters were revealed after we separated patients into motor complete versus motor incomplete SCI groups. Indeed, individuals with cervical motor complete SCI showed a lower baseline systolic blood pressure as well as a higher prevalence of OH during acute rehabilitation. Previously it was reported that acute SCI in humans, especially at the cervical level, results in severe hypotension and persistent bradycardia that are common components of neurogenic shock.8 Clinical observations strongly suggest that the extent over which prolonged and severe hypotension occurs, requiring vasopressor therapy, is associated with the grade of the SCI, and can last up to 5 weeks after injury.1, 8
We evaluated the influence of age, gender, level and grade of injury on the development of OH after SCI, and found that the level and grade of SCI were the two major contributing factors. These findings were consistent with observations in previous studies4, 13, 14, 15 Illman et al.4 reported that OH was most likely to develop in quadriplegic rather than in paraplegic individuals regardless of grade of injury. In our study, patients with upper thoracic SCI did not show significant decreases in baseline blood pressure, but still did experience OH, with the majority of OH observed in motor complete individuals. However, one of the limitations of our study was that with only two patients having upper thoracic motor complete injuries, our study is likely underpowered to make valid comparisons with those upper thoracic patients who were motor complete injuries. Nevertheless, the prevalence of OH was higher in upper thoracic motor complete patients, than in cervical motor incomplete patients, suggesting that the grade of the SCI has very strong influence on development of OH.
Determining a single factor which is most contributory to the development of cardiovascular disturbance in individuals with SCI remains difficult.8, 10 A variety of factors may predispose SCI individuals to OH including impaired baroreflex function16, 17 smaller plasma volumes, hyponatremia18, 19 and cardiovascular deconditioning,20 especially in the early period following SCI, owing to prolonged periods of bed rest. Any combination of these factors following SCI is likely to increase the likelihood and severity of OH. However, insufficient sympathetic control resulting in lack of reflex vasoconstriction is considered to be among the major causes of initial hypotension and persistent OH in individuals with SCI.1, 8, 10 Low sympathetic tone following SCI is a result of interruption of descending axons within the spinal cord, traveling from the brainstem to the sympathetic preganglionic neurons localized within the lateral horns of the thoracic and upper lumbar segments of the spinal cord. Previous animal experimental data and clinical observation suggest that the grade of injury to the descending spinal pathways may influence the severity of cardiovascular dysfunction following SCI.21, 22 Supraspinal control of at least one-quarter of spinal sympathetic neurons can preserve blood pressure regulation and prevent development of OH in patients with cervical SCI.23 Our present findings show that in contrast to patients with cervical complete SCI, patients with cervical incomplete SCI had a significantly lower prevalence of OH, which resolved by the end of the acute rehabilitation period (1 month after injury). Similar results were reported by Frisbie24 where patients with complete cervical injuries showed greater instability of cutaneous microcirculation than patients with incomplete cervical injuries.
Other important mechanisms of OH in SCI individuals are the lack of skeletal muscle pumping and impaired pulmonary pump. Individuals with SCI lack the continuous reciprocal activation of postural skeletal muscles that provides compression on veins and maintains venous return to the heart when in upright position.25, 26 Furthermore, Miller and co-investigators27 suggested that the skeletal muscle pump is relatively ineffective at competing with the respiratory muscle pump with respect to femoral venous return. Not surprisingly, in our study, the individuals with cervical and high thoracic SCI showed the most severe and prolonged OH. The majority of these individuals have compromised pulmonary function and a significant proportion of their total body skeletal muscle mass has no voluntary control. Patients with lower or incomplete SCI have a better functioning pulmonary pump or some (even spastic) movement in their lower extremities, which improves the return of the blood to the heart and prevents them from developing OH later in rehabilitation. Similar observations were recently reported by Frisbie.28
Limitations of the study
We would like to acknowledge some shortcomings of this study. The retrospective collection of data with possible inaccuracies in charting and the small number of patients within the thoracic subgroups of the study were limitations. Other factors contributing to OH including medications and medical complications and comorbidities may not have been captured by our study. As such, 22 patients with complete cervical SCI were managed initially with dopamine, but it was not used beyond day 5 after SCI. Some other factors were outlined in our discussion. We would also refer readers to a recent review on OH following SCI.1
Conclusions
Cardiovascular disturbances are common in the acute rehabilitation period after SCI. Changes in baseline cardiovascular parameters are characterized by a low baseline systolic blood pressure and the presence of OH. OH is observed most frequently in patients with complete cervical SCI. OH generally improves over the first month following injury, but in cases of motor complete cervical and upper thoracic SCI, it may persist beyond the first month of rehabilitation, suggesting level and completeness of injury are the strongest predictors of OH.
References
Claydon VE, Steeves JD, Krassioukov A . Orthostatic hypotension following spinal cord injury: understanding clinical pathophysiology. Spinal Cord 2006; 44: 341–351.
Bravo G, Guizar-Sahagun G, Ibarra A, Centurion D, Villalon CM . Cardiovascular alterations after spinal cord injury: an overview. Curr Med Chem Cardiovasc Hematol Agents 2004; 2: 133–148.
Mathias CJ . Orthostatic hypotension: causes, mechanisms, and influencing factors. Neurol 1995; 45: S6–S11.
Illman A, Stiller K, Williams M . The prevalence of orthostatic hypotension during physiotherapy treatment in patients with an acute spinal cord injury. Spinal Cord 2000; 38: 741–747.
Cariga P, Ahmed S, Mathias CJ, Gardner BP . The prevalence and association of neck (coat-hanger) pain and orthostatic (postural) hypotension in human spinal cord injury. Spinal Cord 2002; 40: 77–82.
El Masry WS . Physiological instability of the spinal cord following injury. Parap 1993; 31: 273–275.
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003; 26: S50–S56.
Krassioukov A, Claydon VE . The clinical problems in cardiovascular control following spinal cord injury: an overview. Prog Brain Res 2006; 152: 223–229.
Teasell R, Arnold AP, Krassioukov AV, Delaney GA . Cardiovascular consequences of loss of supraspinal control of the sympathetic nervous system following spinal cord injuries. Arch Phys Med Rehabil 2000; 81: 506–516.
Mathias CJ, Frankel HL . Autonomic disturbances in spinal cord lesions. In: Bannister R, Mathias CJ (eds). Autonomic Failure, A Textbook of Clinical Disorders of the Autonomic Nervous System. Oxford University Press, Oxford, UK, 2002.
The Consensus Committee of the American Autonomic Society and the American Academy of Neurology. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. Neurol 1996; 46: 1470.
Ackery A, Tator C, Krassioukov A . A global perspective on spinal cord injury epidemiology. J Neurotraum 2004; 21: 1355–1370.
Claydon VE, Krassioukov A . Orthostatatic hypotention and autonomic pathways following spinal cord injury. J Neurotrauma 2006; 23: 1713–1725.
Robertson D, Davis TL . Recent advances in the treatment of orthostatic hypotension. Neurol 1995; 45: S26–S32.
Mukand J, Karlin L, Barrs K, Lublin P . Midodrine for the management of orthostatic hypotension in patients with spinal cord injury: A case report. Arch Phys Med Rehabil 2001; 82: 694–696.
Engelke KA, Shea JD, Doerr DF, Convertino VA . Enhanced carotid–cardiac baroflex response and elimination of orthostatic hypotension 24 h after acute exercise in paraplegics. Parap 1992; 30: 872–879.
Wecht JM, De Meersman RE, Weir JP, Spungen AM, Bauman WA . Cardiac autonomic responses to progressive head-up tilt in individuals with paraplegia. Clin Auton Res 2003; 13: 433–438.
Frisbie JH . Salt wasting, hypotension, polydipsia, and hyponatremia and the level of spinal cord injury. Spinal Cord [E-pub ahead of print: 10 October 2006. doi: 10.1038/sj.sc.3101984].
Frisbie JH . Postural hypotension, hyponatremia, and salt and water intake: case reports. J Spinal Cord Med 2004; 27: 133–137.
Vaziri ND . Nitric oxide in microgravity-induced orthostatic intolerance: Relevance to spinal cord injury. J Spinal Cord Med 2003; 26: 5–11.
Maiorov DN, Fehlings MG, Krassioukov AV . Relationship between severity of spinal cord injury and abnormalities in neurogenic cardiovascular control in conscious rats. J Neurotraum 1998; 15: 365–374.
Furlan JC, Fehlings MG, Shannon P, Norenberg MD, Krassioukov AV . Descending vasomotor pathways in humans: correlation between axonal preservation and cardiovascular dysfunction after spinal cord injury. J Neurotraum 2003; 20: 1351–1363.
Munakata M, Kameyama J, Nunokawa T, Ito N, Yoshinaga K . Altered Mayer wave and baroreflex profiles in high spinal cord injury. Am J Hypertens 2001; 14: 141–148.
Frisbie JH . Microvascular instability in tetraplegic patients: preliminary observations. Spinal Cord 2004; 42: 290–293.
Faghri PD, Yount JP, Pesce WJ, Seetharama S, Votto JJ . Circulatory hypokinesis and functional electric stimulation during standing in persons with spinal cord injury. Arch Phys Med Rehabil 2001; 82: 1587–1595.
Guyton AC, Richardson TQ, Langston JB . Regulation of cardiac output and venous return. Clin Anesth 1964; 3: 1–34.
Miller JD, Pegelow DF, Jacques AJ, Dempsey JA . Skeletal muscle pump versus respiratory muscle pump: modulation of venous return from the locomotor limb in humans. J Physiol 2005; 563: 925–943.
Frisbie JH, Sharma GV, Brahma P, Hess MJ, Hayes JA . Recurrent pulmonary embolism and pulmonary hypertension in chronic tetraplegia. Spinal Cord 2005; 43: 625–630.
Acknowledgements
This study was supported by grant from the Rick Hansen Man In Motion Foundation (Dr A Krassioukov principal investigator). We acknowledge the help and support of Mrs Sukhpal Dhaliwal from the Health Records Department of Vancouver General Hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sidorov, E., Townson, A., Dvorak, M. et al. Orthostatic hypotension in the first month following acute spinal cord injury. Spinal Cord 46, 65–69 (2008). https://doi.org/10.1038/sj.sc.3102064
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102064
Keywords
This article is cited by
-
Using a logarithmic model to predict functional independence after spinal cord injury: a retrospective study
Spinal Cord (2019)
-
A walking disaster: a case of incomplete spinal cord injury with symptomatic orthostatic hypotension
Clinical Autonomic Research (2015)
-
Peripheral vascular function in spinal cord injury: a systematic review
Spinal Cord (2013)
-
Influence of the neurological level of spinal cord injury on cardiovascular outcomes in humans: a meta-analysis
Spinal Cord (2012)
-
International spinal cord injury cardiovascular function basic data set
Spinal Cord (2010)