Abstract
Approximately two-thirds of stroke patients initially suffer from impaired mobility.
The clinical pathways for rehabilitation of gait after stroke are based on a systematic literature search for randomized clinical studies and reviews with the following clinically relevant outcome variables: walking ability, balance, gait velocity, and walking endurance. For each of these outcome variables, evidence-based recommendations were formulated separately for the subacute and chronic stages after stroke. The German ReMoS guideline forms the basis for this work.
The recommendations are compared with those of four other European and North American guidelines. The main commonalities and differences are discussed.
This overview also helps to identify elementary rules for rehabilitation of gait. These rules should be considered when establishing regional rehabilitation programs and clinical pathways in different countries.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Stroke is one of the leading causes for disability in adults. Approximately two-thirds of stroke patients suffer initially from disturbed mobility (Jorgensen et al. 1995). The scope for functional recovery is greatest during the first few months (Kwakkel et al. 2006). Therefore, early and effective rehabilitation training is an important denominator for the final functional outcome of the patients and subsequently for their quality of life.
In the last years, more and more evidence has been accumulated for well-defined rehabilitative interventions including good-quality multicenter studies (e.g., Duncan et al. 2011) and Cochrane reviews (e.g., Saunders et al. 2009). In the German guideline about rehabilitation of mobility after stroke (ReMoS), this evidence has been structured according to clinical meaningful outcome variables separately for the acute/subacute and the chronic phase after stroke (ReMoS Working Group 2015). A similar approach has been chosen by most of the other guidelines the present results were compared with.
Practical therapy recommendations were given for restoration or improvement of gait separately in patients who are initially not able to walk without help and for those who are able to walk, for the improvement of gait velocity, of walking distance and of balance (Flowchart 1).
Unfortunately, there are hardly any high-quality studies of walking as part of everyday activities: e.g., getting up from a low, unstable chair, maneuvering a slippery surface, and carrying fragile dishes or hot meals from the kitchen to the living room.
As it is very difficult to establish a meaningful, reliable, and standardized test for these basic activities, it might be more promising to search for the underlying elementary requirements for such movements. One of the most important requirements is the ability to balance oneself in many different positions and situations. These requirements and strategies to cope with these challenges have been studied in detail by Pérennou and coworkers in the last decades.
2 Best Evidence for Rehabilitations of Gait: Methodology
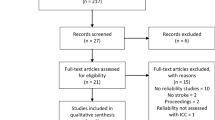
A German guideline about rehabilitation of gait after stroke (ReMoS Working Group 2015, Dohle et al. 2016) forms the basis for this chapter. As part of their systematic guideline development program, the German Society for Neurorehabilitation (DGNR) joined forces with “Physio Deutschland,” the German Society for Physiotherapy (Deutscher Verband für Physiotherapie), to develop a guideline for rehabilitation of gait after stroke (ReMoS). As an S2e-guideline, a systematic review of the literature has been performed using Medline (PubMed), Pedro und the Cochrane Library (2012), and performing additional hand search (in 2012, 2014, and again in 2015). Eleven systematic reviews and 188 RCTs were identified. Forty-one different principles of interventions have been identified.
Many RCTs present the effect of an intervention for several of the outcome parameters: restoration or improvement of gait, improvement of gait velocity and walking distance, and improvement of balance. Functional Ambulation Categories (FAC) were the predominant assessment for the ability to walk, and the 10-m walking test and 6-min walking test were most commonly used to measure the walking speed and walking distance/walking capacity and the Berg Balance Scale and the Timed Up and Go (TUG) test are most often used to assess functional aspects of balance. In addition, we distinguished whether the intervention took place within the first 6 months in the acute or subacute phase after stroke, or after 6 months in the chronic phase after stroke.
For each intervention, a coherent evaluation was performed, separately for each outcome criteria and clinical phase. The evaluation was based on the evidence of all the available literature and performed according to the principles of the GRADE scheme. The resulting quality of evidence category (high, medium, low, or very low) served as a basis for our recommendations taking into account possible side effects: (A—“ought to,” B—“should,” 0—“can,” “therapeutic option”). The recommendations given in this chapter follow the same rules as outlined in chapter “Clinical Pathways in Stroke Rehabilitation: Background, Scope, and Methods” (see Chap. 2).
The specific ReMoS guideline methodology has been described in detail in German (ReMoS Working Group). The present version has been updated to include recent literature and developments. The German version of the guideline can be obtained in print by the Hippocampus Verlag, Bad Honnef, Germany (www.hippocampus.de) or downloaded from the website of the German Society for Neurorehabilitation (https://www.dgnr.de/images/pdf/leitlinien/S2e_Leitlinie_Rehabilitation_der_Mobilitaet_nach_Schlaganfall.pdf). Tables 1, 2, 3, 4 and 5 of the present publication are modified translations from the original German version of the ReMoS guideline.
The original evidence and the resulting recommendations were compared with the evidence and the resulting recommendations presented in four other international guidelines, which also studied sensorimotor interventions after stroke in detail:
-
Practice Guideline for Physical Therapy in patients with stroke (Royal Dutch Society for Physical Therapy 2014); (KNGF guideline).
-
Guideline for adult stroke rehabilitation and recovery (American Heart Association/American Stroke Association 2016) (AHA/ASA guideline).
-
Canadian Stroke Best Practice Recommendations, Canadian Heart and Stroke Foundation, 6th Edition, 2019 (Canadian guideline)
-
Clinical Practice Guideline to improve locomotor function following chronic stroke, incomplete spinal cord injury, and brain injury; American Physical Therapy Association, 2020. (APTA guideline).
Similarities and differences between the main recommendations of the different guidelines are discussed. The structure of the ReMoS guideline was used as the structural basis for the comparison. An additional paragraph has been added about early intensive training in the acute phase after stroke (paragraph 3).
3 Early Intensive Training in the Acute Phase (24 H) After Stroke
Early intensive training in the acute phase directly after stroke may be counterproductive: a steady, but less intensive training scheme leads to a less positive effect directly after the training session, but a more positive outcome 3 months later (e.g., Avert Trial Collaboration Group 2015). This result is in line with results in some animal studies, which show that early intensive training leads to additional damage of tissue at risk close to the lesion site (e.g., Humm et al. 1998). Marzolini et al. (2019) have studied this question in more detail and argue that initial therapy sessions should be brief, and cerebral hypotension should be avoided. Furthermore, as stroke can also affect the function of the heart, possible cardiac manifestations should be kept in mind (Marzolini et al. 2019).
Thus, during the first 24 h, mobilization should be performed cautiously even in seemingly fit patients and exercise intensity should be light in the first days, slowly increasing to moderate. Specific clinical guidelines based on recovery stages from neurological and cardiovascular perspectives are provided by Marzolini et al. (2019).
4 Restoration of Gait in Severely Affected Patients Who cannot Walk Without Help
In patients who cannot walk without help, rehabilitation training with a high number of walking cycles early after stroke improves the chances of patients to walk independently at 6 months considerably (Pohl et al. 2007). The present literature suggests that several hundred walking cycles should be achieved in each training session during the first weeks after stroke (e.g., Pohl et al. 2007). This aim can be achieved by the dedicated personal effort of two or more therapists who help the patient to keep in an upright position and continue to move the feet of the patients continuously early after stroke (Peurala et al. 2009). This approach is dependent on a considerable physical effort by the therapists. Machine supported training regimes have also been used for the neurologically severely affected patients based on either exoskeletons or end-effector devices (e.g., Mehrholz and Pohl 2012). A recent Cochrane analysis showed comparable evidence for both technical approaches: Patients who received physiotherapy in combination with electromechanical-assisted gait training after stroke were more likely to achieve independent walking than people who receive gait training without these devices (Mehrholz et al. 2017). This justifies now an equal recommendation for both end-effector devices and exoskeletons, (B—recommendation; different to the original ReMoS recommendation (2015)).
An improvement of gait categories from non-ambulatory (FAC 0–1) to independent ambulatory (FAC 4 + 5) was only seen in patients in their acute or early subacute phases. It was not achieved, when intensive training of gait was commenced in non-ambulatory patients in their late subacute or chronic phases after stroke.
In the subacute stage after stroke, intensive gait training should be performed, in order to reestablish the ability to walk (low-to-moderate level of evidence). If available and appropriate, intensive physiotherapy should be combined with the use of an end-effector–based device or an exoskeleton (high quality of evidence; B—recommendation, see also Table 1).
For patients, who are still bedridden, there is low quality of evidence that cyclic multichannel stimulation to generate movements similar to a walking pattern can facilitate the ability to walk later on (Yan et al. 2005); 0—recommendation, Table 1). Interestingly, an adjoining neglect training also facilitates the ability to learn to walk again (Paolucci et al. 1996); (low quality of evidence; 0—recommendation, Table 1). The same is true for motor imagery as a component of gait training (low quality of evidence, 0—recommendation, Table 1).
4.1 Discussion: Restoration of Gait in Non-Ambulatory Patients
“Intensive, repetitive mobility-task training” is recommended by the AHA/ASA guideline for all individuals with gait limitations after stroke (2016) based on a high quality of evidence. Intensive training of mobility is also advocated by the Dutch and Canadian guidelines with similarly high evidence levels. Even though there is only limited direct evidence for intensive conventional gait training in non-ambulatory patients (FAC 1–2; see for example, Peurala et al. 2009), there is strong evidence for the benefit of higher number of steps during training sessions using mechanical devices in this patient group (Table 1, see discussion above).
Similar to the present recommendations for the use of an end-effector–based device or an exoskeleton in combination with conventional physiotherapy and gait training (Table 1, see above), the Dutch KNGF guideline (2014) stated that “it has been demonstrated that robot-assisted gait training for stroke patients who are unable to walk independently improves their … walking ability and performance of basic activities of daily living, compared to conventional therapy (including overground walking).” The two North American guidelines (AHA/ASA Guideline 2016; Canadian Guideline 2019) base their recommendations on basically the same evidence as the two European guidelines of 2014 and 2015 and especially on the Cochrane reviews by Mehrholz et al. (2013, 2017). However, their recommendations are more cautious: “mechanically assisted walking may be considered in patients who are non-ambulatory or have low ambulatory ability early after stroke” (AHA/ASA Guideline 2016); “Electromechanical (robotic) assisted gait training devices could be considered for patients who would not otherwise practice walking. They should not be used in place of conventional gait therapy.” (Canadian Guideline 2019).
Three of the guidelines (ReMoS; KNGF; and AHA/ASA) advocate to consider the use of these mechanical devices mainly in the early subacute phase (up to 3 months) after stroke. The guideline of the American physiotherapists (APTA Guideline 2020) does not address the ability to walk directly. However, with regard to walking speed und duration it states explicitly that “clinicians should not perform walking interventions with exoskeletal robotics on a treadmill or elliptical devices to improve walking speed and distance in individuals greater than 6 months following acute-onset CNS injury as compared with alternative interventions (APTA Guideline 2020).”
4.2 Summary
For non-ambulatory patients after stroke, all the guidelines advocate intensive, progressive, and task-related mobility training, with direct and indirect evidence for intensive gait training especially during the (early) subacute phase after stroke. A Cochrane review (Mehrholz et al. 2017) showed that patients who received physiotherapy in combination with electromechanical-assisted gait training after stroke were more likely to achieve independent walking than people who receive gait training without these devices. However, the strength of recommendations for the use of these devices in the first months after stroke varies between guidelines.
5 Improvement of Gait in Patients Who Walk Independently or With Little Help
The high number of steps is again the key to improvement in this patient group. However, support by devices such as an exoskeleton or an end-effector device does not improve patient’s performance further (Dias et al. 2007). In rehabilitative practice, intensive training of walking on the ground and/or walking on treadmills are often used (e.g., Duncan et al. 2011). Regardless of the exact mode of training (with or without a treadmill), intensity of therapy should be progressive, e.g., with an increase of speed, difficulties or complexity over time (Pohl et al. 2002). Such training can also be performed as “circuit training.”
Progressive high-intensity training is especially effective in the subacute phase after stroke (B—recommendations, Table 2). In chronic stroke, it also led to an improvement of gait in these patients, although with a lower quality of evidence for this patient group (0—recommendation, Table 2).
The effect of botulinum toxin injections was evaluated in chronic patients with a spastic equinovarus deformity. A reduction of the use of supportive devices was achieved. There was however no improvement of the abovementioned clinical outcome parameters (Pittock et al. 2003) (B—recommendation for chronic patients with spastic equinovarus deformity).
In patients who can walk independently with or without an aid or with little help an intensive and progressive gait training should be performed in the subacute stage after stroke (moderate quality of evidence; B–recommendation, see also Table 2) and can be performed (intermittently) in the chronic phase after stroke (low quality of evidence, 0–recommendation).
Task-specific training combined with motor imagery, usage of walking devices (e.g., crane, stick), the use of functional electrical stimulation, and additional electroacupuncture all had lower levels of evidence and may be used during training (0—recommendations for the subacute phase, Table 2). The same was true for intensive and progressive training in the chronic phase after stroke (0—recommendation for the chronic phase, Table 2).
5.1 Discussion: Improving Walking Ability in Ambulatory and Nearly Ambulatory Patients
The AHA/ASA guidelines (2016) recommend an intensive, repetitive, and task-related training also for this group of patients—similar to the recommendation above. The KGNF and the Canadian guidelines support this recommendation: e.g., “task and goal-oriented training that is repetitive and progressively adapted should be used to improve performance of selected lower-extremity tasks such as sit to stand, walking distance and walking speed” (Canadian Guideline 2019). There are however open questions: Where should such training be performed: on the ground or on a treadmill? What is the advantage of circle training, which is advocated by several of the guidelines? And do the level of evidence and the class of recommendation differ between the guidelines, especially for some of “our” low-level recommendations?
Training on the ground is the most natural place and does not need any additional technical equipment. And at least for chronic stroke patients, it has been demonstrated that “overground gait training by stroke patients who are able to walk without physical support is more effective in increasing walking distance and reducing anxiety than walking on a treadmill” (KGNF Guideline 2014).
“Group therapy with circuit training is a reasonable approach to improve walking.” (AHA/ASA guideline) “It has been demonstrated that circuit class training (CCT) for walking and other mobility-related functions and activities improves walking distance/speed, sitting and standing balance and walking ability, and reduces inactivity in patients with a stroke” (KNGF Guideline 2014; evidence for patients in the subacute and chronic phases after stroke). Circuit class training allows therapists to combine advantages of group and individual treatments: if a reasonable ratio between patients and therapists is guaranteed (e.g., 2:1), therapists can use the positive aspects of group dynamics and also concentrate during individual time slots on those aspects of gait, which are especially important for individual patients. Thus, circle training tries to combine the advantages of the traditional one therapist–one patient relationship with the economically more effective therapist-patient ratio in group settings.
Overground walking exercises can be combined with treadmill training with or without body support to improve walking ability (AHA/ASA guideline). Treadmill-based training “should be used … as an adjunct to over-ground training or when over-ground training is not available or appropriate” (Canadian guideline, evidence for subacute and chronic stroke patients). Treadmill training can be especially useful for patients, which are more severely affected and may profit from body weight support to train more effectively. It has even been demonstrated “that overground gait training for patients with a stroke who are unable to walk independently at the start of therapy has an adverse effect on their aerobic endurance compared to body-weight supported walking exercises” (KNGF Guideline 2014).
Treadmill-based gait training (with or without body weight support) can also been used to enhance specific aspects of gait: walking speed and distance walked (see paragraphs 7 and 8). Thus, treadmill-based training can be used twofold: either for specifically defined patient groups (e.g., with body weight support) or for the training and optimization of specific tasks (e.g., maximal speed training (see 7) or training of endurance (see 8)). And sometimes it will just provide an alternative to a training session within a cold and rainy or snowy environment outside the building!
When we prepared the ReMoS guideline, we saw cognitive training (e.g., motor imagery in the subacute phase), external stimulation instead of usage of walking aids (e.g., FES in the subacute phase after stroke), and virtual reality in the chronic phase after stroke as treatment options, which might rapidly develop and become standard treatment methods (see Table 2).
According to the Canadian guidelines (2019), “mental practice should be considered as an adjunct to lower extremity motor retraining.” The role of cognitive training in daily routine seems to increase slowly over time. Mental imagery, movement observation, and dual-task paradigms become more and more popular (see also Table 4, paragraph 7). Cognitive training allows patients to concentrate on specific details of the tasks (motor imagery, motor observation) during a learning phase before trying to automatize the task, e.g., with the help of dual-task paradigms. It is important that the learning phase does always include not only imagined or observed but also “real practice.” Physiologically this may correspond to changing functional connections between different sensorimotor areas (e.g., Stephan et al. 1995; Hardwick et al. 2018). Only then will cognitive training develop its full potential during the learning process.
In patients with remedial foot paresis (foot drop) ankle foot orthoses (AFO) remain the standard (e.g. AHA/ASA Guideline 2016). Similarly, the Canadian Guidelines (2019) advise that “ankle-foot orthoses should be used on selected patients with foot drop following proper assessment and with follow-up to verify its effectiveness” (evidence for the subacute and chronic stages after stroke). Neuromuscular electrical stimulation remains a valid alternative to an AFO (AHA/ASA Guideline 2016).
Functional electrical stimulation (FES) is often used to improve strength and function (gait). According to the Canadian guideline, “FES should be used in selected patients, but the effects may not be sustained” (Canadian Guideline 2019, evidence for subacute and chronic stages after stroke). There was no substantial change of the quality of evidence in the last years.
Finally, VR combined with progressive training may be used in the chronic phase after stroke (Table 2). The Dutch guideline (2014) is uncertain about the advantages of VR in combination with conventional therapy. The North American guidelines consider VR as possibly beneficial (AHA/ASA Guideline 2016) or as a possible adjunct (Canadian Guideline 2019). The APTA Guideline (2020) is the only guideline which gives a strong recommendation for the use of VR in conjunction with gait training in chronic patients.
These diverging classes of recommendations even in the two guidelines which were published within the last 2 months (Canadian Guideline Dec. 2019 and APTA Guideline Jan. 2020) indicate that for the lower extremities there is still uncertainty about the exact role of VR in routine clinical therapy. Thus, a strong recommendation cannot (yet) be given.
5.2 Summary
In ambulatory patients and patients who need a little help to walk after stroke all guidelines advocate intensive, progressive, and task-related gait training in order to further improve walking ability. Recommendations are given for overground walking and additional treadmill-based therapy. Treadmill-based therapies have different advantages: a) they may be especially useful for more severely affected patients and b) they support the training of specific aspects of walking, walking speed, and distance walked (paragraphs 7 and 8).
Cognitive training, external stimulation, and virtual reality are specific methods of training, which have become more popular over the last years. However, until now, the quality of evidence is not yet very high and therefore recommendations for their therapeutic use are not yet very strong.
6 Improvement of Balance, Reduction of Falls
Isolated balance training does not lead to an improvement of balance during walking or to a reduction of falls in stroke patients. An integration of balance training into the context of standing and walking seems to be the key aspect for clinical meaningful improvements. (Duncan et al. 2003). It is therefore not surprising that a “motor relearning program” with a focus on activities of daily living shows a clear improvement of functionally relevant balance parameters (Chan et al. 2006). This evidence exists mainly for the subacute phase (moderate quality of evidence, B—recommendations for the subacute phase, Table 3) and with a lower quality of evidence also for the chronic phase (0—recommendation). Such an integration of balance exercises into gait-related training may also lead to a reduction of the number of falls (Duncan 2011).
In order to improve balance in the subacute stage after stroke and reduce the number of falls in patients who can walk independently with or without an aid or with little help dynamic balance training should be performed as an integral part of an intensive gait training (moderate quality of evidence, B—recommendation, see also Table 3). An intensive supervised home training program with progression and a motor relearning program have the same quality of evidence for the subacute stage after stroke (moderate quality of evidence, B—recommendations).
There is low quality of evidence that an increase in gait speed without accompanying balance training may lead to a higher number of falls (Duncan et al. 2011). Therefore, context dependent balance training should be part of any mobility training after stroke.
Conventional gait training combined with training using mechanical devices (treadmill, end-effector device, or exoskeleton), and strength and endurance training may also improve balance, especially in the subacute and chronic stages after stroke (low quality of evidence, 0—recommendation, Table 3). If balance training is performed as a specific training session, training with an unstable support base (Saeys et al. 2012) or with a systematic reduction of the size of the support base (McClellan and Ada 2004) is recommended. Ai Chi (Tai Chi in the water) seems also be beneficial (Noh et al. 2008) (low quality of evidence and 0—recommendations for those interventions in the subacute and/or chronic phases after stroke; see Table 3).
6.1 Discussion: Improvement of Balance, Reduction of Falls
Balance training programs are encouraged for those stroke patients who fall or who have fear of falling (e.g., AHA/ASA Guidelines 2016). The Dutch KNGF Guideline (2014) and the ReMoS guideline also encourage the use of such programs (see Table 3).
At first sight, however, the other recommendations of the different guidelines vary widely regarding the best therapies to improve balance: e.g., training on a force platform is advocated (Canadian guideline and to a lesser extent KNGF guideline) or dismissed (ReMoS Guideline, APTA guideline); similarly treadmill training may lead to an improvement of balance (Canadian guideline) or may increase the number of falls (Duncan 2011; ReMoS Guideline, paragraph 7).
A second look however reveals that the goals of the different recommendations differ; taking these different goals into account, the full picture becomes more unified again.
-
(A)
Exercising postural control with visual feedback while standing on a force platform improves the postural sway in stance (KNGF Guideline 2014), such exercises are also advocated by the Canadian guidelines (2019) to train standing. These exercises do, however, not improve dynamic balance e.g., while walking (ReMoS guideline) and are therefore discouraged, if patients want to improve their balance during walking (see also (APTA guideline for the chronic phase, 2020)).
-
(B)
Balance training on an unstable support base and balance boards (ReMoS guideline, subacute, and chronic phase (Table 3); Canadian Guideline 2019, chronic phase), and balance training with virtual reality while standing in the chronic phase (ReMoS guideline (Table 3) and Canadian Guideline 2019), but not in the subacute phase after stroke (Canadian Guideline 2019) may improve dynamic balance and especially balance while walking.
-
(C)
Treadmill training with partial body weight support in the subacute phase (Canadian Guideline 2019) and training with other mechanical devices (see Table 3, especially in severely affected patients) may improve dynamic balance. However, intensive gait training on a treadmill to improve gait speed may also lead to a higher number of falls compared to intensive home-based training (Duncan 2011; for discussion see also Nave et al. 2019). Duncan et al. (2011) argue that presumably the intensity of balance training was too low compared to the intensity of gait speed training on the treadmill. Thus, it may depend on the context whether treadmill training is facilitating or inhibiting the rehabilitation of dynamic balance during walking.
-
(D)
Exercising balance may not only improve walking abilities. It has also been demonstrated that exercising balance during various activities results in improved performance of basic activities of daily living in the subacute and chronic phases after stroke (KNGF guideline).
-
(E)
Balance may also be stabilized using assistive devices or an orthosis if appropriate (AHA/ASA Guideline 2016;).
Thus, balance training while performing functional relevant tasks will lead to an improvement of balance within the context of these tasks. As far as we know, there is not much carryover of “balance abilities” from one functional task to another. In clinical practice, patients may show different degrees of balance control between slow and fast walking, between walking in an open space, and while navigating obstacles between walking with and without carrying objects in their hands. It is important to identify those differences and address them during the rehabilitative process if necessary.
6.2 Summary
In stroke patients, environmentally adapted balance training improves those aspects of balance which are specifically trained: (a) exercising postural control on a force platform improves postural sway in stance, (b) training of walking abilities by overground gait training, circle training, or with the help of walking devices (e.g., treadmill, end-effector devices, exoskeletons) improves standing balance, walking ability, and walking distance and speed, and (c) exercising balance during various basic activities results in improved performance of those basic activities in daily living. According to the clinical data, there seems to be very limited carryover between different aspects of balance control. Therefore, balance should be trained within the context of walking, and while performing, ADL tasks in order to reduce the risk of falls and resulting injuries.
7 Improvement of Walking Speed
Once walking ability including basic balance control has been achieved, other outcome variables become important such as walking speed or walking distance. To improve walking speed, a progressive increase of training requirements is the dominant therapeutic principle. Progressive circuit training (Outermans et al. 2010) and progressive treadmill training (Pohl et al. 2002; Eich et al. 2004) have the highest quality of evidence (A—recommendations for the subacute phase, Table 4). Treadmill training without monitoring of heart frequency or perceived exertion or an intensive home exercise programs also have a positive effect (Duncan et al. 2011), but at a lower quality of evidence (B—recommendations for the subacute phase, Table 4). Progressive anaerobic training without direct functional relevance, however, does not lead to a further improvement of maximal gait speed, even when compared to “relaxation” (Nave et al. 2019). In this study (PHYS-stroke), both subacute patient groups showed a comparable increase in gait speed when the interventions were added to a standard rehabilitation program. This result demonstrates the importance of task- and goal-directed training, when patients, who have already learned the basic walking skills, try to achieve maximal walking speed.
An increase of walking velocity can also be achieved by intensive training in the chronic phase after stroke (see, for example, (Duncan et al. 2011)), however, the overall quality of evidence is lower than for patients in the subacute phase (0—recommendation, Table 4).
Stimulation of flexor-reflex afferents synchronous to the steps (Spaich et al. 2014) leads to an increase of velocity in the subacute phase (moderate quality of evidence, B—recommendation). In patients with a leg paresis, gait training with an orthosis (Thijssen et al. 2007; Erel et al. 2011) may also increase gait velocity (moderate quality of evidence, B—recommendation for the chronic phase, Table 4). Until today, there is however no evidence for a differential effectiveness of static or dynamic devices (de Seze et al. 2011).
-
In order to increase walking velocity in patients who can walk independently with or without an aid or with little help, goal-directed progressive training of gait velocity ought to be performed (high quality of evidence, A—recommendation for the subacute phase after stroke, see also Table 4).
-
If this is not possible, an intensive gait training with or without a use of a treadmill, an intensive supervised home training program or training with stimulation of flexor-reflex afferents should be performed in the subacute stage (moderate quality of evidence, B—recommendation).
-
In the chronic stage, an orthosis with or without electrical stimulation should be applied in appropriate patients if available (moderate quality of evidence, B—recommendation).
-
Intensive task specific gait, strength, endurance, and cognitive training can also be performed in the chronic stage (0—recommendation).
The effectiveness of the different intervention may be further improved by the combination of gait training with other techniques in the subacute and chronic stages. There are encouraging results for the combination of gait training with cognitive training (e.g., movement observation, movement imagery (Verma et al. 2011), training under dual-task conditions), with additional stimulations and/or feedback (electrical stimulation, acupuncture, rhythmic acoustic stimulation (Thaut et al. 1997), and acoustic feedback (Schauer and Mauritz 2003)) as well as with additional strength and endurance training (low quality of evidence and 0—recommendations for all interventions; for some interventions only for the subacute or for the chronic phase, see also Table 4). An isolated use of these techniques out of a functional context does, however, not lead to the desired improvements.
7.1 Discussion: Improvement of Walking Speed
Again repetitive, progressive, and task-related training forms, the basis for any training-related improvement of gait speed in the subacute phase (Table 4; AHA/ASA Guideline 2016; Canadian Guideline 2019).
Training on the ground, possibly also in the form of circuit training and treadmill training are the two main modes of training which are often combined. Treadmill training with or without body weight support should (Canadian guideline) or could (Dutch guideline) be used to improve walking speed after stroke. Especially with regard to maximum walking speed, it has been demonstrated that treadmill training without body weight support is more effective than conventional gait training (Dutch guideline). Mehrholz et al. (2017) have shown that the quality of evidence for the use of treadmills is highest for ambulatory patients in the first 3 months. However, although the improvement of maximum walking speed was statistically significant at the end of treatment, even these patients had no persisting beneficial effects.
Thus, whenever possible, the achieved improvements in walking speed should be transferred into meaningful and relevant tasks of daily routine (see Table 4).
Strength and endurance training and balance training are further components of such an intensive training program. Strength and aerobic endurance training are advocated by all guidelines in this context (e.g., Canadian guideline (2019) and Dutch Guideline 2014). The role of aerobic endurance training in stroke rehabilitation will be discussed in more detail in the next paragraph chapter (paragraph 8). The importance of balance training was already shown in the previous paragraph (paragraph 6).
Rhythmic acoustic stimulation (RAS) is a further technique to facilitate the speed of repetitive movements and furthermore to influence the gait dynamics. While the Dutch (2014), the ReMoS and the AHA/ASA guideline (2016) identified a low quality of evidence and gave weak recommendations (e.g., Table 4), the Canadian guideline (2019) advised that “rhythmic auditory stimulation should be considered for improving gait parameters in stroke patients, including gait velocity ….” Evidence for RAS in stroke is building up, although there is still a need for long-term evaluations and for a deeper understanding of its (patho-)physiology in healthy subjects (Stephan et al. 2002) and patients. As a reduced effect over time is known, it might be advisable to try to preserve the gain in walking speed by including such tasks in daily routine similar to the strategy after treadmill training (see above). As RAS is much easier to administer than treadmill training, shorter RAS sessions can easily be included in daily or weekly routines.
7.2 Summary
Task- and goal-oriented training that is repetitive and progressively adapted should be used to improve walking speed. Overground training and treadmill training are the most common forms of training.
In order to improve comfortable walking speed, strength and aerobic endurance training, balance training, rhythmic acoustic stimulation and mental observation, and motor imagery help to train further aspects of mobility. In order to improve specifically maximal walking speed, structured treadmill training may be most promising as it allows the patients to concentrate on this specific aspect of mobility. Thus, similar to training in sports, basic skills are the basis for advanced training with specific goals.
Unfortunately, the training at the rehabilitation center does not lead to a permanent improvement of function on a stable level. Therefore, whenever possible, the achieved improvements in walking speed should be transferred into meaningful and relevant tasks of daily routine.
8 Improvement of Walking Distance
Walking longer distances (e.g., for 6 min as in the 6-min walking test) does not only require a sufficient quality of gait parameters but also cardiovascular fitness. The American Heart Association (AHA) has developed criteria for effective endurance training such as a minimal training duration, optimal heart frequency, and perceived levels of exertion (Gordon et al. 2004). In order to improve walking distance, the cardiovascular fitness training has to be embedded into a specific functional context, e.g., treadmill training (16) or task-specific circuit training (Outermans et al. 2010) (high quality of evidence and A—recommendations for the subacute phase; moderate quality of evidence and B—recommendation for the chronic phase, Table 5). Isolated aerobic endurance training on a cycling ergometer does not improve walking distance (Katz-Leurer et al. 2003). This result stresses the importance of task- and goal-directed training also for the improvement of walking distance.
Other progressive forms of training without monitoring of heart frequency or perceived exertion such as supervised home training (Duncan et al. 2011) or progressive treadmill training (Pohl et al. 2002) have a lower quality of evidence (moderate quality of evidence and B—recommendations for the subacute phase; low quality of evidence and 0—recommendations for the chronic phase, Table 5).
Improvement can be achieved both in the subacute and in the chronic phases after stroke, once basic walking ability has been achieved (e.g., (Duncan et al. 2011)). However, the overall quality of evidence is higher for patients in the subacute phase than for patients in the chronic phase leading to different levels of recommendation (see above).
In chronic stroke, patients with paresis may benefit from the use of assistive devices such as an orthosis. Continuous use of an orthosis with electrical stimulation also leads to an improvement of walking distance (Kottink et al. 2007) (moderate quality of evidence, B—recommendation).
-
In the chronic stage, task-specific endurance training, e.g., progressive aerobic treadmill training should be performed or an orthosis with electrical peroneal stimulation should be applied if indicated and available (moderate quality of evidence, B—recommendation).
-
In order to increase walking distance in patients who can walk independently with or without an aid or with little help task- and goal-specific endurance training ought to be performed, especially in the subacute phase after stroke (high quality of evidence, A—recommendation, see also Table 5).
-
If this is not possible, an intensive gait training with or without a use of a treadmill, an intensive supervised home training program should be performed in the subacute stage (moderate quality of evidence, B—recommendation).
Elements of cognitive training (motor imagery, motor observation), additional stimulation techniques (peroneal stimulation, functional electrical stimulation), and especially task-specific endurance and strength training with or without feedback can also enhance walking distance (low quality of evidence and 0—recommendations for all interventions in the subacute and/or chronic phases after stroke, Table 5).
8.1 Discussion: Increasing Walking Distance
Strength and aerobic endurance training within a task- and goal-related training program is the key to build up walking capacity after stroke. Strength and endurance training should be repetitive and progressively adapted (e.g., Canadian Guideline 2019).
Again, a combination of overground training with treadmill training seems to be most useful to combine the strength of both training forms (see the Dutch Guideline 2014, for the advantages of overground training, the Canadian Guideline 2019 for the advantages of treadmill training).
Such a setting also allows to include strength training in a functional context. It has been shown to be less effective: for persons with mild-to-moderate impairment in lower extremity function when performed on its own (Canadian Guideline 2019). The Canadian Guideline (2019) suggests that “individually-tailored aerobic training involving large muscle groups should be incorporated into a comprehensive stroke rehabilitation program to enhance cardiovascular endurance and cognitive function.” Such training can be easily performed as part of a comprehensive training regime to further walking capacity.
The Canadian Guideline (2019) gives recommendations, which investigations should be performed and which precautions should be taken to avoid harm to the patients. They further recommend “patients should participate in aerobic exercise at least 3 times weekly for a minimum of 8 weeks, progressing as tolerated to 20 minutes or more per session, exclusive of warm-up and cooldown” and “heart rate and blood pressure should be monitored during training to ensure safety and attainment of target exercise intensity.” More detailed recommendations for patient safety are given by Marzolini et al. (2019).
Training walking distance provides implicitly some feedback about the distance walked to every patient. Different forms of structured feedback have been used to provide the patients with information about their progress and details of their performance: verbal feedback (Dutch Guideline 2014), biofeedback, in the form of visual and/or auditory signals to indicate unequal weight bearing and timing (Canadian Guideline 2019), and EMG feedback (AHA/ASA Guideline 2016; Dutch Guideline 2014). However, none of the technical feedback signals have led to a substantial enhancement of functional recovery and were strongly recommended in the guidelines. Verbal feedback seems to be the most promising form of feedback, possibly associated with a caring and supportive attitude of the therapist.
Continuous training after discharge is a problem for most patients after stroke. For aerobic exercise, the Canadian Guideline (2019) suggest: “to ensure long-term maintenance of health benefits, a planned transition from structured aerobic exercise to more self-directed physical activity at home or in the community should be implemented.” Furthermore, strategies to address specific barriers to physical activity related to patients, healthcare providers, family, and/or the environment should be employed. These recommendations are important for the transition of most learned skills on discharge from the rehabilitation hospital or center.
8.2 Summary
Task- and goal-specific strength and aerobic endurance training should be the focus of training to enhance walking distance after stroke. It should incorporate both overground training and treadmill training, if available. Pre-participation screening and monitoring during aerobic training should be performed to ensure patient safety.
Treadmill training has the advantage that it allows easy monitoring during training and attainment of target exercise intensity. However, it is difficult to maintain such a structure outside a rehabilitative setting. Therefore, a planned transition from a structured therapy setting to more self-directed physical activity at home or in the community should be implemented.
9 General Discussion and Conclusions
Five different guidelines with recommendations for rehabilitative therapies were compared. All of them were published by scientific societies. Their description of the timeline of rehabilitation was similar: the acute stage or phase lasted for about a week after stroke, the subacute stage until the end of the sixth month with a subdivision between an early subacute phase (up to 3 months) and a late subacute phase (after 3 months up to 6 months). Thereafter began the chronic phase after stroke.
Most of the evidence for specific interventions and the recommendations based on the evidence were similar between the guidelines. This is not surprising, as more or less the same literature formed the basis for the guideline, and the process of writing a guideline is now standardized internationally.
Nevertheless, the classification of the literature and the critical appraisal process also led to some different recommendations in different regions of the world.
First, the critical appraisal of a study may lead to different results regarding the level and/or quality of evidence. Second, synthesis of the evidence of individual studies may lead to different categories of quality of evidence for specific interventions. Furthermore, the quality of evidence for a specific intervention may change over time: there are up to 5 years difference between the years of publication of the different guidelines. And during this time, further studies have been published, which may change the overall quality of evidence or the estimate of therapeutic effect itself.
More often, however, the writers of the guideline will disagree about the level of recommendation. The GRADE system does explicitly require the guideline writers to include not only the quality of evidence but also relevant context factors and the degree of certainty of the recommendation. Therefore, it is not surprising when two or more writers disagree about the class of recommendation, especially when they have a different methodological, cultural, economic, and/or geographic background. From this perspective, the more or less unified view on the process of rehabilitation of walking after stroke is more surprising than the discrepancies between the guidelines.
The evidence underlying the recommendations suggests elementary rules for recovery and rehabilitation of gait according to the different stages of recovery after stroke. These elementary rules are valid for patients regardless of the country or region they live in and form a basis to shape local and regional clinical pathways.
-
In the acute phase, directly after stroke (first 24 h), very intensive training may impair the degree of recovery 3 months later.
-
In patients who cannot walk, intensive task-specific training (e.g., a high number of repetitions of the full gait cycle) supports recovery of basic walking abilities in patients who cannot walk in the subacute stage after stroke. There is no evidence that such an intensive training is still effective to regain basic walking abilities in the chronic stage after stroke in this patient group. Thus, the training of compensatory modes of mobility (e.g., wheelchair handling) may be a major therapeutic aim in these patients (see Flowchart 2).
-
In patients who can walk independently or with some help, intensive task-specific training supports improvement or even restoration of gait. Often balance, walking speed, and walking distance are the main therapeutic goals in these patients (see Flowchart 3). There is higher quality of evidence for such training in the subacute than in the chronic stage after stroke.
-
Clinically meaningful improvements of balance are best achieved when dynamic balance training is performed as an integral part of stance and gait training and/or during relevant ADL sessions. Such training may also lead to a reduction of the number of falls after stroke. Again, there is higher quality of evidence for training in the subacute than in the chronic stage after stroke.
-
While basic walking abilities and balance seem to be basic elements of mobility which have to be relearned early after stroke, walking speed and walking distance can be improved both during the subacute and chronic phases after stroke. Their training is most effective if the demands are increased progressively. It is not yet known, whether walking speed in the chronic stage is influenced by training schedules in the early phase after stroke.
-
In addition to the main interventions, a great number of possible interventions are available, which have also been shown to be effective. These may be chosen according to the specificity of the clinical deficits and the individual preferences of the patients.
-
In contrast to other tasks and activities after stroke (e.g., hand motor control, speech), gait and balance training seems to be more effective when the relevant functions are trained task and goal-specific with regard to the relevant activity. There is not much carryover from one task to another. This is even true for the training of strength and endurance.
-
In the same line, additional stimulation techniques in order to further plasticity (e.g., central and peripheral stimulation) seem to be only effective when performed in combination with functionally relevant aspects of gait training.
In the last years, goal setting during neurological rehabilitation concentrated more and more on activities, which are often more meaningful to patients than basic functions, which were mainly trained earlier in the twentieth century. Not surprisingly, the main outcome parameters of scientific studies are today mostly activities and participation including quality of life—but not functions any longer. Therefore, we learned a lot about how to help patients to regain predefined activities and skills—but less on how to change basic networks in the brain and train basic sensorimotor abilities outside the labs.
The aim of our work was not only to evaluate the different forms of rehabilitative interventions but also to distill the principles of effective treatment for the different aspects of mobility. This is especially important as worldwide most strokes happen in low- and middle-income countries (Norrving and Kissela 2013) and thus not in Western Europe, North America, or Australia, where most of the guideline development takes place. Local and regional culture and traditions in Africa, the Middle East, or South America may stress the importance of other aspects of mobility, e.g., “standing and walking without a visible aid” and of therapeutic settings, e.g., “therapeutic sessions with individual therapists instead of sessions in a group setting.” Regional and local traditions and the cultural background will influence goal setting and the choice of therapeutic interventions. Regardless of regional and local traditions, the above described elementary rules should be part of these clinical pathways to further the recovery of walking ability after stroke.
References
AHA/ASA Guideline (2016) Guidelines for adult stroke rehabilitation and recovery. A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 47:e98–e169. https://doi.org/10.1161/STR.0000000000000098
APTA Guideline (2020) Clinical practice guideline to improve locomotor function following chronic stroke, incomplete spinal cord injury, and brain injury. Academy of Neurologic Physical Therapy. JNPT 44:49–100
AVERT Trial Collaboration Group, Bernhardt J, Langhorne P, Lindley RI, Thrift AG, Ellery F, Collier J, Churilov L, Moodie M, Dewey H, Donnan G (2015) Efficacy and safety of very early mobilisation within 24 h of stroke onset (AVERT): a randomised controlled trial. Lancet 386:46–55
Canadian Guideline (2019) Rehabilitation and recovery following stroke module 2019. Canadian stroke best practice reecommendations, 2019. Heart and Stroke Foundation, Ottawa, ON
Chan DY, Chan CC, Au DK (2006) Motor relearning programme for stroke patients: a randomized controlled trial. Clin Rehabil 20(3):191–200
de Seze MP, Bonhomme C, Daviet JC, Burguete E, Machat H, Rousseaux M, Mazaux JM (2011) Effect of early compensation of distal motor deficiency by the chignon ankle-foot orthosis on gait in hemiplegic patients: a randomized pilot study. Clin Rehabil 25(11):989–998
Dias D, Lains J, Pereira A, Nunes R, Caldas J, Amaral C et al (2007) Can we improve gait skills in chronic hemiplegics? A randomised control trial with gait trainer. Eura Medicophys 43(4):499–504
Dohle C, Tholen R, Wittenberg H, Quintern J, Saal S, Stephan KM (2016) Evidence-based rehabilitation of mobility after stroke. [Article in German]. Nervenarzt 87(10):1062–1067. https://doi.org/10.1007/s00115-016-0188-8
Duncan P, Studenski S, Richards L, Gollub S, Lai SM, Reker D et al (2003) Randomized clinical trial of therapeutic exercise in subacute stroke. Stroke 34(9):2173–2180
Duncan PW, Sullivan KJ, Behrman AL, Azen SP, Wu SS, Nadeau SE et al (2011) Body-weight-supported treadmill rehabilitation after stroke. N Engl J Med 364(21):2026–2036. https://doi.org/10.1056/NEJMoa1010790
Eich HJ, Mach H, Werner C, Hesse S (2004) Aerobic treadmill plus Bobath walking training improves walking in subacute stroke: a randomized controlled trial. Clin Rehabil 18(6):640–651
Erel S, Uygur F, Engin SI, Yakut Y (2011) The effects of dynamic ankle-foot orthoses in chronic stroke patients at three-month follow-up: a randomized controlled trial. Clin Rehabil 25(6):515–523
Gordon NF, Gulanick M, Costa F, Fletcher G, Franklin BA, Roth EJ, Shephard T (2004) Physical activity and exercise recommendations for stroke survivors: an American Heart Association scientific statement from the council on clinical cardiology, subcommittee on exercise, cardiac rehabilitation, and prevention; the council on cardiovascular nursing; the council on nutrition, physical activity, and metabolism; and the stroke council. Circulation 109(16):2031–2041
Hardwick RM, Caspers S, Eickhoff SB, Swinnen SP (2018) Neural correlates of action: comparing meta-analyses of imagery, observation, and execution. Neurosci Biobehav Rev 94:31–44
Humm JL, Kozlowski DA, James DC, Gotts JE, Schallert T (1998) Use-dependent exacerbation of brain damage occurs during an early post-lesion vulnerable period. Brain Res 783:286–292
Jorgensen HS, Nakayama H, Raaschou HO, Vive-Larsen J, Stoier M, Olsen TS (1995) Outcome and time course of recovery in stroke. Part I: outcome. The Copenhagen Stroke Study. Arch Phys Med Rehabil 76(5):399–405
Katz-Leurer M, Shochina M, Carmeli E, Friedlander Y (2003) The influence of early aerobic training on the functional capacity in patients with cerebrovascular accident at the subacute stage. Arch Phys Med Rehabil 84(11):1609–1614
KNGF Guideline (2014) Royal Dutch Society for physical therapy (Koninklijk Nederlands Genootschap voor Fysiotherapie, KNGF)
Kottink AI, Hermens HJ, Nene AV, Tenniglo MJ, van der Aa HE, Buschman HP, Ijzerman MJ (2007) A randomized controlled trial of an implantable 2-channel peroneal nerve stimulator on walking speed and activity in poststroke hemiplegia. Arch Phys Med Rehabil 88(8):971–978
Kwakkel G, Kollen B, Twisk J (2006) Impact of time on improvement of outcome after stroke. Stroke 37(9):2348–2353
Marzolini S, Robertson AD, Oh P, Goodman JM, Corbett D, Du X, MacIntosh BJ (2019) Aerobic training and mobilization early post-stroke: cautions and consideration. Front Neurol 10:article 1187
McClellan R, Ada L (2004) A six-week, resource-efficient mobility program after discharge from rehabilitation improves standing in people affected by stroke: placebo-controlled, randomised trial. Aust J Physiother 50(3):163–167
Mehrholz J, Pohl M (2012) Electromechanical-assisted gait training after stroke: a systematic review comparing end-effector and exoskeleton devices. J Rehabil Med 44(3):193–199
Mehrholz J, Elsner B, Werner C, Kugler J, Pohl M (2013) Electromechanical-assisted training for walking after stroke: updated evidence. Stroke 44(10):e127–e128
Mehrholz J, Thomas S, Werner C, Kugler J, Pohl M, Elsner B (2017) Electromechanical-assisted training for walking after stroke. Cochrane Database Syst Rev 5:CD006185. https://doi.org/10.1002/14651858.CD006185
Nave AH, Rackoll T, Grittner U et al (2019) Physical fittness training in patients with subacute stroke (PHYS-STROKE): multicentre, randomised controlled, endpoint blinded trial. BMJ 366:I5101
Noh DK, Lim JY, Shin HI, Paik NJ (2008) The effect of aquatic therapy on postural balance and muscle strength in stroke survivors--a randomized controlled pilot trial. Clin Rehabil 22(10–11):966–976
Norrving B, Kissela B (2013) The global burden of stroke and need for a continuum of care. Neurol 80(Suppl 2):S5–S12. https://doi.org/10.1212/WNL.0b013e3182762397
Outermans JC, Van Peppen RP, Wittink H, Takken T, Kwakkel G (2010) Effects of a high-intensity task-oriented training on gait performance early after stroke: a pilot study. Clin Rehabil 24(11):979–987
Paolucci S, Antonucci G, Guariglia C, Magnotti L, Pizzamiglio L, Zoccolotti P (1996) Facilitatory effect of neglect rehabilitation on the recovery of left hemiplegic stroke patients: a cross-over study. J Neurol 243(4):308–314
Peurala SH, Airaksinen O, Huuskonen P, Jakala P, Juhakoski M, Sandell K et al (2009) Effects of intensive therapy using gait trainer or floor walking exercises early after stroke. J Rehabil Med 41(3):166–173
Pittock SJ, Moore AP, Hardiman O, Ehler E, Kovac M, Bojakowski J et al (2003) A double-blind randomised placebo-controlled evaluation of three doses of botulinum toxin type a (Dysport) in the treatment of spastic equinovarus deformity after stroke. Cerebrovasc Dis 15(4):289–300
Pohl M, Mehrholz J, Ritschel C, Ruckriem S (2002) Speed-dependent treadmill training in ambulatory hemiparetic stroke patients: a randomized controlled trial. Stroke 33(2):553–558
Pohl M, Werner C, Holzgraefe M, Kroczek G, Mehrholz J, Wingendorf I, Hoölig G, Koch R, Hesse S (2007) Repetitive locomotor training and physiotherapy improve walking and basic activities of daily living after stroke: a single-blind, randomized multicentre trial (DEutsche GAngtrainerStudie, DEGAS). Clin Rehabil 21:17–27
ReMoS Arbeitsgruppe, Dohle C, Quintern J, Saal S, Stephan KM, Tholen R, Wittenberg H (2015) S2e-Leitlinie Rehabilitation der Mobilität nach Schlaganfall (ReMoS). Neurol Rehabil 21(7):355–494
Saeys W, Vereeck L, Truijen S, Lafosse C, Wuyts FP, Heyning PV (2012) Randomized controlled trial of truncal exercises early after stroke to improve balance and mobility. Neurorehabil Neural Repair 26(3):231–238
Saunders DH, Greig CA, Mead GE, Young A (2009) Physical fitness training for stroke patients. Cochrane Database Syst Rev (4):CD003316
Schauer M, Mauritz KH (2003) Musical motor feedback (MMF) in walking hemiparetic stroke patients: randomized trials of gait improvement. Clin Rehabil 17(7):713–722
Spaich EG, Svaneborg N, Jorgensen HR, Andersen OK (2014) Rehabilitation of the hemiparetic gait by nociceptive withdrawal reflex-based functional electrical therapy: a randomized, single-blinded study. J Neuroeng Rehabil 11(81)
Stephan KM, Fink GR, Passingham RE, Silbersweig D, Ceballos-Baumann AO, Frith CD, Frackowiak RS (1995) Functional anatomy of the mental representation of upper extremity movements in healthy subjects. J Neurophysiol 73(1):373–386
Stephan KM, Thaut MH, Wunderlich G, Schicks W, Tian B, Tellmann L, Schmitz T, Herzog H, McIntosh GC, Seitz RJ, Hömberg V (2002) Conscious and subconscious sensorimotor synchronization—prefrontal cortex and the influence of awareness. Neuroimage 15(2):345–352
Thaut MH, McIntosh GC, Rice RR (1997) Rhythmic facilitation of gait training in hemiparetic stroke rehabilitation. J Neurol Sci 151(2):207–212
Thijssen DH, Paulus R, van Uden CJ, Kooloos JG, Hopman MT (2007) Decreased energy cost and improved gait pattern using a new orthosis in persons with long-term stroke. Arch Phys Med Rehabil 88(2):181–186
Verma R, Arya KN, Garg RK, Singh T (2011) Task-oriented circuit class training program with motor imagery for gait rehabilitation in poststroke patients: a randomized controlled trial. Top Stroke Rehabil 18(Suppl 1):620–632
Yan T, Hui-Chan CW, Li LS (2005) Functional electrical stimulation improves motor recovery of the lower extremity and walking ability of subjects with first acute stroke: a randomized placebo-controlled trial. Stroke 36(1):80–85
Acknowledgments
K. M. Stephan is member of the ReMoS working group (Dohle C, Quintern J, Saal S, Stephan KM, Tholen R, Wittenberg H; in alphabetical order) that developed the evidence-based guideline on “Rehabilitation of Mobility after Stroke (ReMoS)” for the German Society of Neurorehabilitation (DGNR). As the systematic search, critical appraisal and best evidence synthesis of that guideline development has been a major information source for this chapter the work of the ReMoS working group is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (http://creativecommons.org/licenses/by-nc-nd/4.0/), which permits any noncommercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if you modified the licensed material. You do not have permission under this license to share adapted material derived from this chapter or parts of it.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2021 The Author(s)
About this chapter
Cite this chapter
Stephan, K.M., Pérennou, D. (2021). Mobility After Stroke: Relearning to Walk. In: Platz, T. (eds) Clinical Pathways in Stroke Rehabilitation. Springer, Cham. https://doi.org/10.1007/978-3-030-58505-1_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-58505-1_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-58504-4
Online ISBN: 978-3-030-58505-1
eBook Packages: MedicineMedicine (R0)