Abstract
Background: The dire state of coronavirus disease (COVID-19) outbreak has had a substantial psychological impact on society.
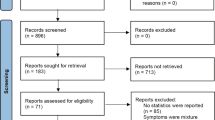
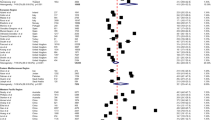
Methods: A systematic search was performed through Medline, PubMed, Embase, Scopus, and Web of Science, to investigate the impact of the COVID-19 pandemic on the psychological health of individuals in various countries. Subgroup analyses considered gender and classification of countries into three continents of America, Europe, and Asia. Only studies that used the COVID-19 Peritraumatic Distress Index (CPDI) questionnaire as a tool to assess mental distress were included in this meta-analysis. Heterogeneity among studies was assessed by I2 statistic, and the random-effects model was utilized to obtain the pooled prevalence.
Results: This pooled analysis included a large data sample of 21 studies consisting of 94,414 participants. The pooled prevalence of the psychological distress during the time of COVID-19 pandemic by CPDI for the continent of Asia was 43% (34.6% mild-to-moderate and 8.4% severe) which was greater than that for Europe (35%; 30% mild-to-moderate and 5% severe) but lower than that for America (64.3%; 45.8% mild to moderate and 18.5% severe). In addition, the prevalence of psychological distress according to CPDI was higher in females (48%; 40% mild to moderate, 13% severe) compared with males (59%; 36% mild to moderate and 5% severe).
Conclusions: Our findings suggest that psychological distress in the Americas is a larger problem than in Asia and European continents. Females appear to be more vulnerable and may therefore require further attention in terms of preventive and management strategies. Implementation of both digital and molecular biomarkers is encouraged to increase objectivity and accuracy of assessing the dynamic changes in mental health in the current and future pandemics.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Huang C, Wang Y, Li X, et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395(10223):497–506
Worldometer: COVID-19 Coronavirus Outbreak; https://www.worldometers.info/coronavirus/ (accessed October 1, 2022).
Xiong J, Lipsitz O, Nasri F, et al (2020) Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord 277:55–64
Preti E, Di Mattei V, Perego G, et al (2020) The Psychological Impact of Epidemic and Pandemic Outbreaks on Healthcare Workers: Rapid Review of the Evidence. Curr Psychiatry Rep 22(8):43. https://doi.org/10.1007/s11920-020-01166-z
Atalan A (2020) Is the lockdown important to prevent the COVID-9 pandemic? Effects on psychology, environment and economy-perspective. Ann Med Surg (Lond) 56:38–42
Brooks SK, Webster RK, Smith LE, et al (2020) The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395(10227):912–920
Vahedian-Azimi A, Moayed MS, Rahimibashar F, et al (2020) Comparison of the severity of psychological distress among four groups of an Iranian population regarding COVID-19 pandemic. BMC Psychiatry 20(1):402. https://doi.org/10.1186/s12888-020-02804-9
Park SC, Park YC (2020) Mental Health Care Measures in Response to the 2019 Novel Coronavirus Outbreak in Korea. Psychiatry Investig 17(2):85–86
Duan L, Zhu G (2020) Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry 7(4):300–302
Qiu J, Shen B, Zhao M, et al (2020) A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr 33(2):e100213. https://doi.org/10.1136/gpsych-2020-100213
Al-Hanawi MK, Mwale ML, Alshareef N, et al (2020) Psychological Distress Amongst Health Workers and the General Public During the COVID-19 Pandemic in Saudi Arabia. Risk Manag Healthc Policy 13:733–742
Ramasubramanian V, Mohandoss AA, Rajendhiran G, et al (2020) Statewide Survey of Psychological Distress Among People of Tamil Nadu in the COVID-19 Pandemic. Indian J Psychol Med 42(4):368–373
Liu S, Heinz A (2020) Cross-Cultural Validity of Psychological Distress Measurement During the Coronavirus Pandemic. Pharmacopsychiatry 53(5):237–238
Moayed MS, Vahedian-Azimi A, Mirmomeni G, et al (2021) Coronavirus (COVID-19)-Associated Psychological Distress Among Medical Students in Iran. Advances in Experimental Medicine and Biology 1321, 245–251. https://doi.org/10.1007/978-3-030-59261-5_21
Moayed MS, Vahedian-Azimi A, Mirmomeni G, et al (2021) A Survey of Psychological Distress Among the Community in the COVID-19 Epidemic: A Cross-Sectional Study. Advances in Experimental Medicine and Biology 1321, 253–260. https://doi.org/10.1007/978-3-030-59261-5_22
Moayed MS, Vahedian-Azimi A, Mirmomeni G, et al (2021) Survey of Immediate Psychological Distress Levels Among Healthcare Workers in the COVID-19 Epidemic: A Cross-Sectional Study. Advances in Experimental Medicine and Biology 1321, 237–243. https://doi.org/10.1007/978-3-030-59261-5_20
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
National Heart, Lung, and Blood Institute (2021) Study Quality Assessment Tools; https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed September 28, 2022
Batra K, Singh TP, Sharma M, Batra R,Schvaneveldt N (2020) Investigating the Psychological Impact of COVID-19 among Healthcare Workers: A Meta-Analysis. Int J Environ Res Public Health 17(23):9096. https://doi.org/10.3390/ijerph17239096
Egger M, Davey Smith G, et al (1997) Bias in meta-analysis detected by a simple, graphical test. Bmj 315(7109):629–634
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Miller JJ, Niu C, Moody S (2020) Child welfare workers and peritraumatic distress: The impact of COVID-19. Child Youth Serv Rev 119:105508. https://doi.org/10.1016/j.childyouth.2020.105508
Abad A, da Silva J, de Paiva Teixeira L, et al (2020) Evaluation of Fear and Peritraumatic Distress during COVID-19 Pandemic in Brazil. Advances in Infectious Diseases 101:84–194. https://doi.org/10.4236/aid.2020.103019
Hübner CVK, Lima Bruscatto M, Dourado Lima R (2020) Distress among Brazilian university students due to the Covid-19 pandemic: survey results and reflections. medRxiv. https://doi.org/10.1101/2020.06.19.20135251
Zhang SX, Wang Y, Afshar Jahanshahi A, et al (2020) First study on mental distress in Brazil during the COVID-19 crisis. medRxiv. https://doi.org/10.1101/2020.04.18.20070896
Krüger-Malpartida H, Pedraz-Petrozzi B, Arevalo-Flores M, et al (2020) Effects on Mental Health After the COVID-19 Lockdown Period: Results From a Population Survey Study in Lima, Peru. medRxiv. https://doi.org/10.21203/rs.3.rs-81117/v1
Picchianti Diamanti A, Cattaruzza MS, Di Rosa R, et al (2020) Psychological Distress in Patients with Autoimmune Arthritis during the COVID-19 Induced Lockdown in Italy. Microorganisms 8(11):1818. https://doi.org/10.3390/microorganisms8111818
Bonati M, Campi R, Zanetti M, et al (2021) Psychological distress among Italians during the 2019 coronavirus disease (COVID-19) quarantine. BMC Psychiatry 21(1):20. https://doi.org/10.1186/s12888-020-03027-8
Pakenham KI, Landi G, Boccolini G, et al (2020) The moderating roles of psychological flexibility and inflexibility on the mental health impacts of COVID-19 pandemic and lockdown in Italy. J Contextual Behav Sci 17:109–118
Landi G, Pakenham KI, Boccolini G, et al (2020) Health Anxiety and Mental Health Outcome During COVID-19 Lockdown in Italy: The Mediating and Moderating Roles of Psychological Flexibility. Front Psychol 11:2195. https://doi.org/10.3389/fpsyg.2020.02195
Ciprandi R, Bonati M, Campi R, et al (2020) Psychological distress in adults with and without cystic fibrosis during the COVID-19 lockdown. J Cyst Fibros 20(2):198–204
Costantini A, Mazzotti E (2020) Italian validation of CoViD-19 Peritraumatic Distress Index and preliminary data in a sample of general population. Riv Psichiatr 55(3):145–151
Marzo RR, Singh A, Mukti RF (2021) A survey of psychological distress among Bangladeshi people during the COVID-19 pandemic. Clin Epidemiol Glob Health 10:100693. https://doi.org/10.1016/j.cegh.2020.100693
Shrestha DB, Thapa BB, Katuwal N, et al (2020) Psychological distress in Nepalese residents during COVID-19 pandemic: a community level survey. BMC Psychiatry 20(1):491. https://doi.org/10.1186/s12888-020-02904-6
Jahanshahi AA, Dinani MM, Madavani AN, et al (2020) The distress of Iranian adults during the Covid-19 pandemic - More distressed than the Chinese and with different predictors. Brain Behav Immun 87:124–125
Nair AKR, Karumaran CS, Kattula D, et al (2020) Stress levels of Indian endodontists during COVID-19 pandemic. Rev Cubana Estomatol 57(3):e3445. https://www.redalyc.org/journal/3786/378664876002/html/. Accessed September 28, 2022
Samson P, Narayan Shah J (2020) Peritraumatic distress and perceived mental healthcare needs among residents of a community housing during COVID-19. Journal of Patan Academy of Health Sciences 7(2):14–22
Marzo RR, Quilatan Villanueva III E, Martinez Faller E, Moralidad Baldonado A (2020) Factors Associated with Psychological Distress among Filipinos during Coronavirus Disease-19 Pandemic Crisis. Open Access Maced J Med Sci 8(T1):309–313
El-Abasiri RA, RilleraMarzo R, Abdelaziz H, et al (2020) Evaluating the Psychological Distress of the Coronavirus Disease 2019 Pandemic in Egypt. European Journal of Molecular & Clinical Medicine 7(5):1–12
Political Map of Countries of Western Asia. https://www.nationsonline.org/oneworld/map/Political-Map-of-Countries-of-Western-Asia.htm. Accessed September 29, 2022
Middle East region, Asia, Africa, and Europe. https://www.britannica.com/place/Middle-East. Accessed September 29, 2022
Sareen J, Erickson J, Medved MI, et al (2013) Risk factors for post-injury mental health problems. Depress Anxiety 30(4):321–327
Chaplin TM (2015) Gender and Emotion Expression: A Developmental Contextual Perspective. Emot Rev 7(1):14–21
COVID-19 and gender equality: Countering the regressive effects; July 15, 2020. https://www.mckinsey.com/featured-insights/future-of-work/covid-19-and-gender-equality-countering-the-regressive-effects. Accessed September 29, 2022
Chakraborty A, Karmakar S (2020) Impact of COVID-19 on Obsessive Compulsive Disorder (OCD). Iran J Psychiatry 15(3):256–259
Yassa M, Yassa A, Yirmibeş C, et al (2020) Anxiety levels and obsessive compulsion symptoms of pregnant women during the COVID-19 pandemic. Turk J Obstet Gynecol 17(3):155–160
Marques de Miranda D, da Silva Athanasio B, Sena Oliveira AC, Simoes ESAC (2020) How is COVID-19 pandemic impacting mental health of children and adolescents? Int J Disaster Risk Reduct 51:101845. https://doi.org/10.1016/j.ijdrr.2020.101845
Kovess-Masfety V, Sowa D, Keyes K, et al (2017) The association between car accident fatalities and children’s fears: A study in seven EU countries. PLoS One 12(8):e0181619. https://doi.org/10.1371/journal.pone.0181619
Mortensen CR, Becker DV, Ackerman JM, et al (2010) Infection breeds reticence: the effects of disease salience on self-perceptions of personality and behavioral avoidance tendencies. Psychol Sci 21(3):440–447
Derivois D, Cénat JM, Joseph NE, et al (2017) Prevalence and determinants of post-traumatic stress disorder, anxiety and depression symptoms in street children survivors of the 2010 earthquake in Haiti, four years after. Child Abuse Negl 67:174–181
Amerio A, Bianchi D, Santi F, et al (2020) Covid-19 pandemic impact on mental health: a web-based cross-sectional survey on a sample of Italian general practitioners. Acta Biomed 91(2):83–88
Kanellopoulos D, Solomonov N, Ritholtz S, et al (2021) The CopeNYP program: A model for brief treatment of psychological distress among healthcare workers and hospital staff. Gen Hosp Psychiatry 73:24–29
Khaing NEE, Lim CS, Soon SP, Oh HC (2022) Prevalence and correlates of psychological distress and coronavirus anxiety among hospital essential services workers in Singapore. Ann Acad Med Singap 51(5):283–291
Osório FL, Zuardi AW, Silveira ILM, et al (2022) Monitoring the Mental Health and Professional Overload of Health Workers in Brazil: A Longitudinal Study Considering the First Wave of the COVID-19 Pandemic. Front Psychiatry 13:852157. https://doi.org/10.3389/fpsyt.2022.852157
Beck E, Daniels J (2022) Intolerance of uncertainty, fear of contamination and perceived social support as predictors of psychological distress in NHS healthcare workers during the COVID-19 pandemic. Psychol Health Med; Jul 6:1–13. https://doi.org/10.1080/13548506.2022.2092762
P1vital® PReDicT Test. https://www.p1vital.com/healthcare/p1vital-predict-test/. Accessed September 30, 2022
Browning M, Bilderbeck AC, Dias R, et al (2021) The clinical effectiveness of using a predictive algorithm to guide antidepressant treatment in primary care (PReDicT): an open-label, randomised controlled trial. Neuropsychopharmacology 46(7):1307–1314
Aardal-Eriksson E, Eriksson TE, Holm AC, Lundin T (1999) Salivary cortisol and serum prolactin in relation to stress rating scales in a group of rescue workers. Biol Psychiatry 46(6):850–855
Wüst S, Wolf J, Hellhammer DH, et al (2000) The cortisol awakening response - normal values and confounds. Noise Health 2(7):79–88
Fekedulegn DB, Andrew ME, Burchfiel CM, et al (2007) Area under the curve and other summary indicators of repeated waking cortisol measurements. Psychosom Med 69(7):651–659
Stalder T, Kirschbaum C, Kudielka BM, et al (2016) Assessment of the cortisol awakening response: Expert consensus guidelines. Psychoneuroendocrinology 63:414–432
Voller A (1978) The enzyme-linked immunosorbent assay (ELISA) (theory, technique and applications). Ric Clin Lab 8(4):289–298
Hunter MR, Gillespie BW, Chen SY (2019) Urban Nature Experiences Reduce Stress in the Context of Daily Life Based on Salivary Biomarkers. Front Psychol 10:722. https://doi.org/10.3389/fpsyg.2019.00722
Stephen L (2017) Multiplex Immunoassay Profiling. Methods Mol Biol 1546:169–176
Stephen L, Schwarz E, Guest PC (2017) Multiplex Immunoassay Profiling of Serum in Psychiatric Disorders. Adv Exp Med Biol 974:149–156
Guest PC, Abbasifard M, Jamialahmadi T, et al (2022) Multiplex Immunoassay for Prediction of Disease Severity Associated with the Cytokine Storm in COVID-19 Cases. Methods Mol Biol 2511:245–256
Engeland CG, Bosch JA, Rohleder N (2019) Salivary Biomarkers in Psychoneuroimmunology. Curr Opin Behav Sci 28:58–65
Young JJ, Bruno D, Pomara N (2014) A review of the relationship between proinflammatory cytokines and major depressive disorder. J Affect Disord 169:15–20
Quagliato LA, Nardi AE (2018) Cytokine alterations in panic disorder: A systematic review. J Affect Disord 228:91–96
Perkins DO, Jeffries CD, Addington J, et al (2015) Towards a psychosis risk blood diagnostic for persons experiencing high-risk symptoms: preliminary results from the NAPLS project. Schizophr Bull 41(2):419–428
Chan MK, Krebs MO, Cox D, et al (2015) Development of a blood-based molecular biomarker test for identification of schizophrenia before disease onset. Transl Psychiatry 5(7):e601. https://doi.org/10.1038/tp.2015.91
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
1 Electronic Supplementary Material
Supplementary Table 4.ST1
Methodological quality assessment of included studies using the National Institutes of Health (NIH) tool (DOCX 16 kb)
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ashtari, S. et al. (2023). Psychological Distress Impact of Coronavirus Disease (COVID-19) Outbreak on Three Continents: A Systematic Review and Meta-analysis. In: Guest , P.C. (eds) Application of Omic Techniques to Identify New Biomarkers and Drug Targets for COVID-19. Advances in Experimental Medicine and Biology(), vol 1412. Springer, Cham. https://doi.org/10.1007/978-3-031-28012-2_4
Download citation
DOI: https://doi.org/10.1007/978-3-031-28012-2_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-28011-5
Online ISBN: 978-3-031-28012-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)