Abstract
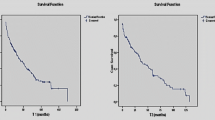
Proximal obstruction is reported to be the most common cause of ventriculoperitoneal (VP) shunt failure, suggesting that imperfect ventricular catheter placement and inadequate valve mechanisms are major causes. This study retrospectively examined patterns of shunt failure in 128 consecutive patients with symptoms of shunt malfunction over a 2-year period. Factors analyzed included site of failure, time from shunt placement or last revision to failure, age of patient at time of failure, infections, and primary etiology of the hydrocephalus. One hundred of these patients required revisions; 14 revisions were due to infections. In this series there was a higher incidence of distal (43%) than of proximal (35%) failure. The difference was not statistically significant when the overall series was considered; however, when factoring time to failure as a variable, marked differences were noted regardless of the underlying cause of hydrocephalus or the age of the patient. Of the 49 patients needing a shunt revision or replacement within 2 years of the previous operation, 50% had proximal malfunction, 14% distal, and 10% had malfunctions attributable directly to the valve itself. Also, 12 of the 14 infections occurred during this time interval. In sharp contrast, of the 51 patients having shunt failure from 2 to more than 12 years after the previous procedure, 72% had distal malfunction, 21% proximal, and only 6% had a faulty valve or infection. This difference between time to failure for proximal versus distal failures was statistically significant (P<0.00001 for both Student's t-test and non-parametric Mann-Whitney U-test). It is concluded that these data are valuable for interpreting outcome studies of novel valve systems and ventricular catheter placement techniques, by defining a time frame during which these modifications can be reliably evaluated.
Similar content being viewed by others
References
Albright AL, Haines SJ, Taylor FH (1988) Function of parietal and frontal shunts in childhood hydrocephalus. J Neurosurg 69: 883–886
Amacher AL, Wellington J (1987) Infantile hydrocephalus: long-term results of surgical therapy. Child's Brain 11: 217–229
Andersson H (1966) Craniosynostosis as a complication after operation for hydrocephalus. Acta Pediatr Scand 55: 192–196
Bierbrauer KS, Storrs B, McClone D, et al (1992) A prospective randomized study of shunt function and infections as a function of shunt placement. Pediatr Neurosurg 16: 287–291
Epstein F (1984) How to keep shunts functioning, or “the impossible dream.” Clin Neurosurg 32: 608–631
Fischer EG, Shillito J (1969) Large abdominal cysts: a complication of peritoneal shunts. Case report. J Neurosurg 31: 441–444
Grosfeld JL, Cooney DR, Smith J (1974) Intra-abdominal complications following ventriculoperitoneal shunt procedures. Pediatrics 54: 791–796
Hoffman HJ, Smith MSM (1987) The use of shunting devices for cerebrospinal fluid in Canada. Can J Neurol Sci 13: 81–87
Keucher TR, Mealey J (1979) Long-term results after ventriculoatrial and ventriculopertoneal shunting for infantile hydrocephalus. J Neurosurg 50: 179–186
McLaurin RL (1989) Ventricular shunts: complications and results. In: McLaurin RL, Schut L, Venes JL, Epstein F (eds) Pediatric neurosurgery. Saunders, Philadelphia, pp 219–229
McLaurin RL, Frame PT (1985) The role of shunt externalization in the management of shunt infection. In: Chapman PH (ed) Concepts in pediatric neurosurgery, vol 6. Karger, Basel, pp 133–146
Oi S, Matsumoto S (1986) Morphological findings of postshunt slit-ventricle in experimental canine hydrocephalus: aspects of causative factors of isolated ventricles and slit-ventricle syndrome. Child's Nerv Syst 2: 179–184
Piatt JH, Carlson CV (1993) A search for determinants of cerebrospinal fluid shunt survival: retrospective analysis of a 14-year institutional experience. Pediatr Neurosurg 19: 233–242
Renier D, Lacombe J, Pierre-Kahn A, Saint-Rose C, Hirsch JF (1984) Factors causing acute shunt infection. J Neurosurg 61: 1072–1078
Scott RM (1990) Preventing and treating shunt complications. In: Scott RM (ed) Hydrocephalus. (Concepts in neurosurgery, vol 3) Williams & Wilkins, Baltimore, pp 115–121
Sekhar LN, Moossy J, Guthkelch AN (1982) Malfunctioning ventriculoperitoneal shunts, clinical and pathological features. J Neurosurg 56: 411–416
Shurtleff DB, Stuntz JT, Hayden PW (1986) Experience with 1201 cerebrospinal fluid shunt procedures. Pediatr Neurosci 12: 49–57
Venes JL, Dauser RC (1987) Epilepsy following ventricular shunt placement. J Neurosurg 66: 154–155
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Kast, J., Duong, D., Nowzari, F. et al. Time-related patterns of ventricular shunt failure. Child's Nerv Syst 10, 524–528 (1994). https://doi.org/10.1007/BF00335075
Received:
Revised:
Issue Date:
DOI: https://doi.org/10.1007/BF00335075