Abstract
Introduction and hypothesis
The aims of the study were to evaluate the per- and post-operative complications and outcomes after cystocele repair with transobturator mesh.
Methods
A retrospective continuous series study was conducted over a period of 3 years. Clinical evaluation was up to 1 year with additional telephonic interview performed after 34 months on average. When stress urinary incontinence (SUI) was associated with the cystocele, it was treated with the same mesh.
Results
One hundred twenty-three patients were treated for cystocele. Per-operative complications occurred in six patients. After 1 year, erosion rate was 6.5%, and only three cystoceles recurred. After treatment of SUI with the same mesh, 87.7% restored continence. Overall patient’s satisfaction rate was 93.5%.
Conclusions
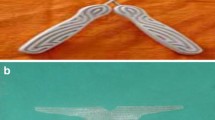
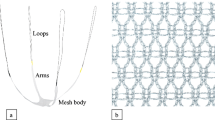
Treatment of cystocele using transobturator four arms mesh appears to reduce the risk of recurrence at 1 year, along with high rate of patient’s satisfaction. The transobturator path of the prosthesis arms seems devoid of serious per- and post-operative risks and allows restoring continence when SUI is present.



Similar content being viewed by others
Abbreviations
- SUI:
-
Stress urinary incontinence
- POP:
-
Pelvic organ prolapse
- TVT:
-
Tension-free vaginal tape
- POP-Q:
-
Pelvic organ prolapse quantification
- BMI:
-
Body mass index
- IVS:
-
Intravaginal sling
References
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Clark AL, Gregory T, Smith VJ, Edwards R (2003) Epidemiologic evaluation of reoperation for surgically treated pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol 189:1261–1267
Whiteside JL, Weber AM, Meyn LA, Walters MD (2004) Risk factors for prolapse recurrence after vaginal repair. Am J Obstet Gynecol 191:1533–1538
Julian TM (1996) The efficacy of Marlex mesh in the repair of severe, recurrent vaginal prolapse of the anterior midvaginal wall. Am J Obstet Gynecol 175:1472–1475
Hugier J, Scali P (1958) Posterior suspension of the genital axis on the lumbosacral disk in the treatment of uterine prolapse. Presse Med 66:781–784
Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 7:81–85 discussion 5–6
Delorme E (2001) Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol 11:1306–1313
Eglin G, Ska JM, Serres X (2003) Transobturator subvesical mesh. Tolerance and short-term results of a 103 case continuous series. Gynecol Obstet Fertil 31:14–19
Fatton B, Amblard J, Debodinance P, Cosson M, Jacquetin B (2007) Transvaginal repair of genital prolapse: preliminary results of a new tension-free vaginal mesh (Prolift technique)—a case series multicentric study. Int Urogynecol J Pelvic Floor Dysfunct 18:743–752
Caquant F, Collinet P, Debodinance P, Berrocal J, Garbin O, Rosenthal C et al (2008) Safety of trans vaginal mesh procedure: retrospective study of 684 patients. J Obstet Gynaecol Res 34:449–456
Nauth MA, Fünfgeld C (2008) Correction of cystocele and stress incontinence with anterior transobturator mesh. Eur J Obstet Gynecol Reprod Biol 136:249–253
Rane A, Kannan K, Barry C, Balakrishnan S, Lim Y, Corstiaans A (2008) Prospective study of the Perigee system for the management of cystocoeles—medium-term follow up. Aust NZ J Obstet Gynaecol 48:427–432
Shippey S, Gutman RE, Quiroz LH, Handa VL (2008) Contemporary approaches to cystocele repair: a survey of AUGS members. J Reprod Med 53:832–836
Petros PE, Ulmsten UI (1993) An integral theory and its method for the diagnosis and management of female urinary incontinence. Scand J Urol Nephrol Suppl 153:1–93
Stein TA, DeLancey JO (2008) Structure of the perineal membrane in females: gross and microscopic anatomy. Obstet Gynecol 111:686–693
Shek KL, Dietz HP, Rane A, Balakrishnan S (2008) Transobturator mesh for cystocele repair: a short- to medium-term follow-up using 3D/4D ultrasound. Ultrasound Obstet Gynecol 32:82–86
Nguyen JN, Burchette RJ (2008) Outcome after anterior vaginal prolapse repair: a randomized controlled trial. Obstet Gynecol 111:891–898
Sivaslioglu AA, Unlubilgin E, Dolen I (2008) A randomized comparison of polypropylene mesh surgery with site-specific surgery in the treatment of cystocele. Int Urogynecol J Pelvic Floor Dysfunct 19:467–471
Birch C, Fynes MM (2002) The role of synthetic and biological prostheses in reconstructive pelvic floor surgery. Curr Opin Obstet Gynecol 14:527–535
Klinge U, Junge K, Spellerberg B, Piroth C, Klosterhalfen B, Schumpelick V (2002) Do multifilament alloplastic meshes increase the infection rate? Analysis of the polymeric surface, the bacteria adherence, and the in vivo consequences in a rat model. J Biomed Mater Res 63:765–771
Dwyer PL, O’Reilly BA (2004) Transvaginal repair of anterior and posterior compartment prolapse with Atrium polypropylene mesh. BJOG 111:831–836
Bader G, Fauconnier A, Guyot B, Ville Y (2006) Use of prosthetic materials in reconstructive pelvic floor surgery. An evidence-based analysis. Gynecol Obstet Fertil 34:292–297
Collinet P, Belot F, Debodinance P, Ha Duc E, Lucot JP, Cosson M (2006) Transvaginal mesh technique for pelvic organ prolapse repair: mesh exposure management and risk factors. Int Urogynecol J Pelvic Floor Dysfunct 17:315–320
Mistrangelo E, Mancuso S, Nadalini C, Lijoi D, Costantini S (2007) Rising use of synthetic mesh in transvaginal pelvic reconstructive surgery: a review of the risk of vaginal erosion. J Minim Invasive Gynecol 14:564–569
Achtari C, Hiscock R, O’Reilly BA, Schierlitz L, Dwyer PL (2005) Risk factors for mesh erosion after transvaginal surgery using polypropylene (Atrium) or composite polypropylene/polyglactin 910 (Vypro II) mesh. Int Urogynecol J Pelvic Floor Dysfunct 16:389–394
Deffieux X, de Tayrac R, Huel C, Bottero J, Gervaise A, Bonnet K et al (2007) Vaginal mesh erosion after transvaginal repair of cystocele using Gynemesh or Gynemesh-Soft in 138 women: a comparative study. Int Urogynecol J Pelvic Floor Dysfunct 18:73–79
Bent AE, Ostergard DR, Zwick-Zaffuto M (1993) Tissue reaction to expanded polytetrafluoroethylene suburethral sling for urinary incontinence: clinical and histologic study. Am J Obstet Gynecol 169:1198–1204
Sergent F, Resch B, Diguet A, Verspyck E, Marpeau L (2006) Cystocele and stress urinary incontinence: assessment of a total treatment by monoprosthesis. Gynecol Obstet Fertil 34:385–392
Spinosa JP, Dubuis PY, Riederer B (2005) Transobturator surgery for female urinary continence: from outside to inside or from inside to outside: a comparative anatomic study. Prog Urol 15:700–706
Warner MA, Martin JT, Schroeder DR, Offord KP, Chute CG (1994) Lower-extremity motor neuropathy associated with surgery performed on patients in a lithotomy position. Anesthesiology 81:6–12
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendix: telephonic interview
Appendix: telephonic interview
-
1.
How will you describe your situation after the surgery, with regards to the prolapse symptoms you had before the operation?
-
(a)
No more symptoms
-
(b)
Better, but still have some
-
(c)
As it was or worse
-
2.
Do you suffer now from symptoms of prolapse? If yes, during rest or effort?
-
3.
Have you been re-operated? In our department or somewhere else?
-
4.
Do you suffer from recurrent urinary infections?
-
5.
Do you suffer from abnormal secretion from the vagina?
-
6.
Do you suffer from (the terms were further explained to the interviewee):
-
Polyuria?
-
Urgency?
-
Incomplete voiding?
-
Stress urinary incontinence?
-
-
7.
Do you practice sexual intercourse?
-
8.
After the operation, the global quality of the sexual intercourse is
-
(a)
Better
-
(b)
Unchanged
-
(c)
Deteriorated
-
9.
Do you suffer from pain during sexual intercourse?
-
10.
Do you suffer from perineal pain or other pain?
-
11.
In terms of global satisfaction from your quality of life before and after the operative intervention, you are
-
(a)
Very satisfied or satisfied
-
(b)
Moderate satisfied
-
(c)
Not satisfied or very not satisfied
-
12.
Do you have any particular remarks to add?
Rights and permissions
About this article
Cite this article
Eboue, C., Marcus-Braun, N. & von Theobald, P. Cystocele repair by transobturator four arms mesh: monocentric experience of first 123 patients. Int Urogynecol J 21, 85–93 (2010). https://doi.org/10.1007/s00192-009-0993-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-009-0993-8