Abstract
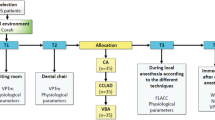
Anxiety experienced by individuals visiting the dental office to receive treatment is common. Evidence has shown biofeedback to be a useful modality of treatment for numerous maladies associated with anxiety. The purpose of the current pilot study was to investigate the use of a novel biofeedback device (RESPeRATE™) to reduce patients’ pre-operative general anxiety levels and consequently reduce the pain associated with dental injections. Eighty-one subjects participated in this study, forty in the experimental group and forty-one in the control group. Subjects in the experimental group used the biofeedback technique, while those in the control group were not exposed to any biofeedback. All subjects filled out a pre-injection anxiety survey, then received an inferior alveolar injection of local anesthetic. Post-injection, both groups were given an anxiety survey and asked to respond to four questions regarding the injection experience using a Visual Analog Scale (VAS). With the use of the respiratory rate biofeedback device, there was a significant reduction of negative feelings regarding the overall injection experience, as measured by a VAS. Our findings demonstrate that this novel biofeedback technique may be helpful in the amelioration of dental anxiety, and may help produce a more pleasant overall experience for the patient.
Similar content being viewed by others
References
Abrahamsson, K. H., Berggren, U., Hallberg, L., & Carlsson, S. G. (2002). Dental phobic patients’ view of dental anxiety and experiences in dental care: A qualitative study. Scandinavian Journal of Caring Sciences, 16, 188–196.
Agresti, A. (2010). Analysis of ordinal categorical data (2nd ed.). Hoboken, NJ: Wiley.
Arun, C. P. (2004). Flight or fight, forbearance and fortitude: the spectrum of actions of catecholamines and their cousins. Annals of the New York Academy of Sciences, 1018, 137–140.
Ayer, W. (2005). Psychology and dentistry: Mental health aspects of patient care. New York, NY: The Haworth Press.
Ballard, B. E. (1968). Biopharmaceutical considerations in subcutaneous and intramuscular drug administration. Journal of Pharmaceutical Sciences, 57, 357–378.
Bijur, P. E., Silver, W., & Gallagher, E. J. (2001). Reliability of the visual analog scale for measurement of acute pain. Academic Emergency Medicine, 8, 1153–1157.
Bouma, J., Uitenbroek, D., Westert, G., Schaub, R. M., & van de Poel, F. (1987). Pathways to full mouth extraction. Community Dentistry and Oral Epidemiology, 15, 301–305.
Breivik, E. K., Björnsson, G. A., & Skovlund, E. (2000). A comparison of pain rating scales by sampling from clinical trial data. Clinical Journal of Pain, 16, 22–28.
Cannon, W. B. (1929). Bodily changes in pain, hunger, fear, and rage (2nd ed.). New York, NY: Appleton-Century-Crofts.
Clark, M. E., & Hirschman, R. (1990). Effects of paced respiration on anxiety reduction in a clinical population. Biofeedback and Self Regulation, 15, 273–284.
Conover, W. J. (1998). Practical nonparametric statistics (3rd ed.). New York, NY: Wiley.
Corah, N. L. (1969). Development of a dental anxiety scale. Journal of Dental Research, 48, 596.
Corah, N. L., Gale, E. N., & Illig, S. J. (1978). Assessment of a dental anxiety scale. Journal of the American Dental Association, 97, 816–819.
Croog, S. H., Baume, R. M., & Nalbandian, J. (1994). Pain response after psychological preparation for repeated periodontal surgery. Journal of the American Dental Association, 125, 1353–1360.
de Burgh Daly, M. (1986). Interactions between respiration and circulation. In N. S. Cherniack & J. G. Widdicombe (Eds.), Handbook of physiology: Section 3: The respiratory system (pp. 529–594). Bethesda, MD: American Physiological Society.
Dworkin, S. F. (1986). Psychological considerations for facilitating anesthesia and sedation in dentistry. In R. A. Dionne & D. M. Laskin (Eds.), Anesthesia and sedation in the dental office (pp. 15–18). New York, NY: Elsevier.
Elliot, W. J., Izzo, J. L., Jr, White, W. B., Rosing, D. R., Snyder, C. S., Alter, A., et al. (2004). Graded blood pressure reduction in hypertensive outpatients associated with use of a device to assist with slow breathing. Journal of Clinical Hypertension (Greenwich), 6, 553–559.
Gallagher, E. J., Bijur, P. E., Latimer, C., & Silver, W. (2002). Reliability and validity of a visual analog scale for acute abdominal pain in the ED. American Journal of Emergency Medicine, 20, 287–290.
Gavish, B. (1995). Self-regulation of respiration using interactive music in a closed loop. In H. Sakura, I. Saito, & T. Kikuchi (Eds.), Biobehavioural self-regulation (pp. 386–390). Toyko, Japan: Springer.
Goodell, G. G., Gallagher, F. J., & Nicoll, B. K. (2000). Comparison of a controlled injection pressure system with a conventional technique. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics, 90, 88–94.
Grossman, E., Grossman, A., Schein, M. H., Zimlichman, R., & Gavish, B. (2001). Breathing-control lowers blood pressure. Journal of Human Hypertension, 15, 263–269.
Hersh, E. V., Houpt, M. I., Cooper, S. A., Feldman, R. S., Wolff, M. S., & Levin, L. M. (1996). Analgesic efficacy and safety of an intraoral lidocaine patch. Journal of the American Dental Association, 127, 1626–1634.
Krochak, M., & Friedman, N. (1998). Using a precision-metered injection system to minimize dental injection anxiety. Compendium of Continuing Education in Dentistry, 19, 137–146.
Liddell, A., & May, B. (1984). Some characteristics of regular and irregular attenders for dental check-ups. British Journal of Clinical Psychology, 23, 19–26.
Lindsay, S., & Jackson, C. (1993). Fear of routine dental treatment in adults: its nature and management. Psychology Health, 8, 135–153.
Malamed, S. F. (2004). Handbook of local anesthesia (5th ed.). St. Louis, MO: CV Mosby.
Malamed, S. F. (2010). Sedation: A guide to patient management (5th ed.). Toronto, ON: Elsevier.
Meles, E., Giannattasio, C., Failla, M., Gentile, G., Capra, A., & Mancia, G. (2004). Nonpharmacologic treatment of hypertension by respiratory exercise in the home setting. American Journal of Hypertension, 17, 370–374.
Milgrom, P., Fiset, L., Melnick, S., & Weinstein, P. (1988). The prevalence and practice management consequences of dental fear in a major US city. Journal of the American Dental Association, 116, 641–647.
Milgrom, P., & Weinstein, P. (1993). Dental fears in general practice: New guidelines for assessment and treatment. International Dental Journal, 43, 288–293.
Moore, R., & Birn, H. (1990). Phenomenon of dental fear. Tandlaegebladet, 94, 34–41.
National Rural Health Association. (2001). Oral health in America: A rural perspective. Kansas City, MO: National Rural Health Association.
Newton, J. T., & Edwards, J. C. (2005). Psychometric properties of the modified dental anxiety scale: An independent replication. Community Dental Health, 22, 40–42.
Nuttall, N. M. (1984). Characteristics of dentally successful and dentally unsuccessful adults. Community Dentistry and Oral Epidemiology, 12, 208–212.
Oosterink, F. M., de Jongh, A., & Aartman, I. H. (2008). What are people afraid of during dental treatment? Anxiety-provoking capacity of 67 stimuli characteristic of the dental setting. European Journal of Oral Sciences, 116, 44–51.
Parati, G., Izzo, J. L., Jr., & Gavish, B. (2007). Respiration and blood pressure. In J. L. Izzo, D. Sica, & H. R. Black (Eds.), Hypertension primer (4th ed., pp. 136–138). Baltimore, MD: Lippincott, Williams and Wilkins.
Pellino, T. A., Gordon, D. B., Engelke, Z. K., Busse, K. L., Collins, M. A., Silver, C. E., et al. (2005). Use of nonpharmacologic interventions for pain and anxiety after total hip and total knee arthroplasty. Orthopaedic Nurses, 24, 182–190.
Reiner, R. (2008). Integrating a portable biofeedback device into clinical practice for patients with anxiety disorders: Results of a pilot study. Applied Psychophysiology Biofeedback, 33, 55–61.
Rogers, K. B., Fielding, A. F., & Markiewicz, S. W. (1989). The effect of warming local anesthetic solutions prior to injection. General Dentistry, 37, 496–499.
Rood, J. P. (1978). The pressures created by inferior alveolar injections. British Dental Journal, 144, 280–282.
Rubin, J. G., Slovin, M., & Krochak, M. (1988). The psychodynamics of dental anxiety and dental phobia. Dental Clinics of North America, 32, 647–656.
Saloum, F. S., Baumgartner, J. C., Marshall, G., & Tinkle, J. (2000). A clinical comparison of pain perception to the Wand and a traditional syringe. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics, 89, 691–695.
Schein, M. H., Gavish, B., Herz, M., Rosner-Kahana, D., Naveh, P., Knishkowy, B., et al. (2001). Treating hypertension with a device that slows and regularises breathing: A randomised, double-blind controlled study. Journal of Human Hypertension, 15, 271–278.
Schuurs, A. H., & Hoogstraten, J. (1993). Appraisal of dental anxiety and fear questionnaires: A review. Community Dentistry and Oral Epidemiology, 21, 329–339.
Seymour, R. A., Charlton, J. E., & Phillips, M. E. (1983). An evaluation of dental pain using visual analogue scales and the McGill pain questionnaire. Journal of Oral and Maxillofacial Surgery, 41, 643–648.
United States General Accounting Office. (2000). Oral health: Factors contributing to low use of dental services by low-income populations. Washington, DC: US General Accounting Office.
Vargas, C. M., Dye, B. A., & Hayes, K. (2003). Oral health care utilization by US rural residents, National Health Interview Survey 1999. Journal of Public Health Dentistry, 63, 150–157.
Voss, J. A., Good, M., Yates, B., Baun, M. M., Thompson, A., & Hertzog, M. (2004). Sedative music reduces anxiety and pain during chair rest after open-heart surgery. Pain, 112, 197–203.
Wewers, M. E., & Lowe, N. K. (1990). A critical review of visual analogue scales in the measurement of clinical phenomena. Research in Nursing and Health, 13, 227–236.
Zautra, A. J., Fasman, R., Davis, M. C., & Craig, A. D. (2010). The effects of slow breathing on affective responses to pain stimuli: An experimental study. Pain, 149, 12–18.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morarend, Q.A., Spector, M.L., Dawson, D.V. et al. The Use of a Respiratory Rate Biofeedback Device to Reduce Dental Anxiety: An Exploratory Investigation. Appl Psychophysiol Biofeedback 36, 63–70 (2011). https://doi.org/10.1007/s10484-011-9148-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10484-011-9148-z