Abstract
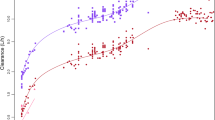
The aim of this work was to determine whether optimizing the study design in terms of ages and sampling times for a drug eliminated solely via cytochrome P450 3A4 (CYP3A4) would allow us to accurately estimate the pharmacokinetic parameters throughout the entire childhood timespan, while taking into account age- and weight-related changes. A linear monocompartmental model with first-order absorption was used successively with three different residual error models and previously published pharmacokinetic parameters (“true values”). The optimal ages were established by D-optimization using the CYP3A4 maturation function to create “optimized demographic databases.” The post-dose times for each previously selected age were determined by D-optimization using the pharmacokinetic model to create “optimized sparse sampling databases.” We simulated concentrations by applying the population pharmacokinetic model to the optimized sparse sampling databases to create optimized concentration databases. The latter were modeled to estimate population pharmacokinetic parameters. We then compared true and estimated parameter values. The established optimal design comprised four age ranges: 0.008 years old (i.e., around 3 days), 0.192 years old (i.e., around 2 months), 1.325 years old, and adults, with the same number of subjects per group and three or four samples per subject, in accordance with the error model. The population pharmacokinetic parameters that we estimated with this design were precise and unbiased (root mean square error [RMSE] and mean prediction error [MPE] less than 11% for clearance and distribution volume and less than 18% for ka), whereas the maturation parameters were unbiased but less precise (MPE < 6% and RMSE < 37%). Based on our results, taking growth and maturation into account a priori in a pediatric pharmacokinetic study is theoretically feasible. However, it requires that very early ages be included in studies, which may present an obstacle to the use of this approach. First-pass effects, alternative elimination routes, and combined elimination pathways should also be investigated.



Similar content being viewed by others
References
Kearns GL, Abdel-Rahman SM, Alander SW, Blowey DL, Leeder JS, Kauffman RE (2003) Developmental pharmacology-drug disposition, action, and therapy in infants and children. N Engl J Med 349:1157–1167
Chalkiadis GA, Anderson BJ (2006) Age and size are the major covariates for prediction of levobupivacaine clearance in children. Paediatr Anaesth 16:275–282
Bjorkman S (2006) Prediction of cytochrome p450-mediated hepatic drug clearance in neonates, infants and children : how accurate are available scaling methods? Clin Pharmacokinet 45:1–11
Edginton AN, Schmitt W, Willmann S (2006) Development and evaluation of a generic physiologically based pharmacokinetic model for children. Clin Pharmacokinet 45:1013–1034
Edginton AN, Schmitt W, Voith B, Willmann S (2006) A mechanistic approach for the scaling of clearance in children. Clin Pharmacokinet 45:683–704
Anderson BJ, Holford NH (2008) Mechanism-based concepts of size and maturity in pharmacokinetics. Annu Rev Pharmacol Toxicol 48:303–332
Johnson TN, Rostami-Hodjegan A, Tucker GT (2006) Prediction of the clearance of eleven drugs and associated variability in neonates, infants and children. Clin Pharmacokinet 45:931–956
EMEA (2006) Guideline on the role of pharmacokinetics in the development of medicinal products in the paediatric population. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500003066.pdf
Tod M, Jullien V, Pons G (2008) Facilitation of drug evaluation in children by population methods and modelling. Clin Pharmacokinet 47:231–243
Anderson BJ, Allegaert K, Holford NH (2006) Population clinical pharmacology of children: modelling covariate effects. Eur J Pediatr 165:819–829
Gueorguieva I, Ogungbenro K, Graham G, Glatt S, Aarons L (2007) A program for individual and population optimal design for univariate and multivariate response pharmacokinetic–pharmacodynamic models. Comput Methods Programs Biomed 86:51–61
Hennig S, Waterhouse TH, Bell SC et al (2007) A d-optimal designed population pharmacokinetic study of oral itraconazole in adult cystic fibrosis patients. Br J Clin Pharmacol 63:438–450
Bazzoli C, Retout S, Comets E and Mentré F (2008) INSERM U, Université Paris 7, Paris, France. PFIM 3.0. Available at: http://www.pfim.biostat.fr/Read_me_PFIM3.0.pdf
Bazzoli C, Retout S, Mentré F (2009) Design evaluation and optimisation in multiple response nonlinear mixed effect models: PFIM 3.0. Comput Methods Programs Biomed 98(1):55–65
Mentre F, Mallet A, Baccar D (1997) Optimal design in random-effects regression models. Biometrika 84:429–442
Retout S, Comets E, Samson A, Mentre F (2007) Design in nonlinear mixed effects models: optimization using the Fedorov-Wynn algorithm and power of the Wald test for binary covariates. Stat Med 26:5162–5179
Retout S, Mentre F (2003) Optimization of individual and population designs using Splus J Pharmacokinet Pharmacodyn 30:417–443
Langlois S, Kreeft JH, Chouinard G, Ross-Chouinard A, East S, Ogilvie RI (1987) Midazolam: kinetics and effects on memory, sensorium, and haemodynamics. Br J Clin Pharmacol 23:273–278
Pentikainen PJ, Valisalmi L, Himberg JJ, Crevoisier C (1989) Pharmacokinetics of midazolam following intravenous and oral administration in patients with chronic liver disease and in healthy subjects. J Clin Pharmacol 29:272–277
Sjovall S, Kanto J, Himberg JJ, Hovi-Viander M, Salo M (1983) CSF penetration and pharmacokinetics of midazolam. Eur J Clin Pharmacol 25:247–251
Chhun S, Jullien V, Rey E, Dulac O, Chiron C, Pons G (2009) Population pharmacokinetics of levetiracetam and dosing recommendation in children with epilepsy. Epilepsia 50:1150–1157
Kerbusch T, Wahlby U, Milligan PA, Karlsson MO (2003) Population pharmacokinetic modelling of darifenacin and its hydroxylated metabolite using pooled data, incorporating saturable first-pass metabolism, CYP2D6 genotype and formulation-dependent bioavailability. Br J Clin Pharmacol 56:639–652
Peeters MY, Prins SA, Knibbe CA et al (2006) Pharmacokinetics and pharmacodynamics of midazolam and metabolites in nonventilated infants after craniofacial surgery. Anesthesiology 105:1135–1146
Mulla H, McCormack P, Lawson G, Firmin RK, Upton DR (2003) Pharmacokinetics of midazolam in neonates undergoing extracorporeal membrane oxygenation. Anesthesiology 99:275–282
Beal SL and Sheiner LB, (eds) (1991) NONMEM user’s guide, University of California at San Francisco, NONMEM Pproject Group, San Francisco
Sheiner LB, Beal SL (1981) Some suggestions for measuring predictive performance. J Pharmacokinet Biopharm 9:503–512
Brendel K, Dartois C, Comets E et al (2007) Are population pharmacokinetic and/or pharmacodynamic models adequately evaluated? A survey of the literature from 2002 to 2004. Clin Pharmacokinet 46:221–234
Green B, Duffull SB (2003) Prospective evaluation of a D-optimal designed population pharmacokinetic study. J Pharmacokinet Pharmacodyn 30:145–161
van Rossum LK, Mathot RA, Cransberg K, Vulto AG (2003) Optimal sampling strategies to assess inulin clearance in children by the inulin single-injection method. Clin Chem 49:1170–1179
Turner PK, Iacono LC, Panetta JC et al (2006) Development and validation of limited sampling models for topotecan lactone pharmacokinetic studies in children. Cancer Chemother Pharmacol 57:475–482
Anderson BJ, Allegaert K, Van den Anker JN, Cossey V, Holford NH (2007) Vancomycin pharmacokinetics in preterm neonates and the prediction of adult clearance. Br J Clin Pharmacol 63:75–84
Tod M, Lokiec F, Bidault R, De Bony F, Petitjean O, Aujard Y (2001) Pharmacokinetics of oral acyclovir in neonates and in infants: a population analysis. Antimicrob Agents Chemother 45:150–157
Gorski JC, Hall SD, Jones DR, VandenBranden M, Wrighton SA (1994) Regioselective biotransformation of midazolam by members of the human cytochrome P450 3A (CYP3A) subfamily. Biochem Pharmacol 47:1643–1653
Eap CB, Buclin T, Hustert E et al (2004) Pharmacokinetics of midazolam in CYP3A4- and CYP3A5-genotyped subjects. Eur J Clin Pharmacol 60:231–236
Lepper ER, Baker SD, Permenter M et al (2005) Effect of common CYP3A4 and CYP3A5 variants on the pharmacokinetics of the cytochrome P450 3A phenotyping probe midazolam in cancer patients. Clin Cancer Res 11:7398–7404
Chenel M, Bouzom F, Aarons L, Ogungbenro K (2008) Drug–drug interaction predictions with PBPK models and optimal multiresponse sampling time designs: application to midazolam and a phase I compound. Part 1: comparison of uniresponse and multiresponse designs using PopDes J Pharmacokinet Pharmacodyn 35:635–659
Hyland R, Osborne T, Payne A et al (2009) In vitro and in vivo glucuronidation of midazolam in humans. Br J Clin Pharmacol 67:445–454
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bouillon-Pichault, M., Jullien, V., Bazzoli, C. et al. Pharmacokinetic design optimization in children and estimation of maturation parameters: example of cytochrome P450 3A4. J Pharmacokinet Pharmacodyn 38, 25–40 (2011). https://doi.org/10.1007/s10928-010-9173-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-010-9173-1