Abstract
Medicinal herbs are nature’s gift to humanity, contributing crucially to the preservation, maintenance and improvement of our health. In order to explore the hepatoprotective potential of prevalent medicinal plants, nine species were selected from different genera based on their ethnomedicinal records in treating different liver-related pathological conditions in South Asia. Besides, the available information was critically analyzed to gain new insights and directions for future investigations towards establishing such natural products as potent hepatoprotective agents or dietary supplements. The hepatoprotective activities of the species have been investigated in a wide variety of in vivo experimental models including carbon tetrachloride-, paracetamol-, iron-, mercuric chloride-, thioacetamide-, cyclophosphamide-, β-d-galactosamine-, cumene hydroperoxide-, α-naphthyl-isothiocyanate-, physical stress- and alcohol-induced hepatotoxicity in rats and mice. All the plants were consistent in their ability to possess hepatoprotective properties. As well, three bioactive isolates namely, schaftoside, echinocystic acid, and eclalbasaponin II were found to have promising hepatoprotective potential. However, extensive comparative studies are warranted in future to establish the relative hepatoprotective potentials of the nine species under discussion. Preparation of poly-herbal formulations from these plants and identification of hepatoprotective phytoconstituents from these plants might open up new avenues in the development of therapeutic hepatoprotective agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver as the largest gland of the body, is significantly contributory to the maintenance and synchronization of vital physiological functions which eventually lead to the preservation of homeostasis (Haque et al. 2017; Khan et al. 2020). It acts as the major physiological site for almost all of these body’s metabolic pathways including the distribution and storage of nutrients and energy, synthesis and regulation of hormones and enzymes, processing of xenobiotics, and neutralization of toxins and pathogens. The liver also serves as an integral component of the digestive system through providing different digestive enzymes at the specific sites as well as the bile juice in duodenum, thus aiding protein and lipid digestion (Kumar et al. 2011). Bile produced in liver is momentarily stored in the gall bladder which later releases it into the duodenum to assist in lipid digestion. Bile salts, which make up majority of the biliary content, acts as detergent and facilitate the solubilization of highly hydrophobic materials including oils, fats, long chain fatty compounds and fat-soluble vitamins, into the highly hydrophilic and acidified digestive content. Moreover, through similar action, bile salts also enable the elimination of cholesterol and other fat-soluble harmful substances such as environmental toxins, carcinogens drugs, xenobiotics, and toxic metabolites (Trauner and Boyer 2003). Besides, majority of the prodrugs, those are given in their inactive forms for minimizing toxicity or enhancing bioavailability, require hepatic enzyme-mediated activation in order to exert their respective therapeutic action (Ortiz de Montellano 2013). Therefore, a healthy liver is crucial for maintaining homeostasis and optimum health. However, liver is susceptible to infection by hundreds of etiological events including microorganisms (hepatitis viruses, yellow fever viruses, cytomegalovirus, Epstein-Barr virus), metabolic problems (obesity related liver disease, hemochromatosis, Wilson’s disease), alcohol, drugs, and chemicals (hepatotoxic substances) as well as different autoimmune diseases (Lavanchy 2009). According to WHO these manifestations contributes to the reduction of working capacities, shortening of life span, and limiting the quality of life, which eventually leads to a high mortality and morbidity rate (Lavanchy 2009; Lok et al. 2001; Waxman and Bulletin 2004). Moreover, oxidative stress has been demonstrated to play a significant role in the etiology and progression of many liver diseases. Oxidative stress signifies an imbalanced oxidative status of cells and tissues as imposed by an over-exposure to free radicals. Many hepatotoxic substances precipitate the formation of powerful free radicals leading to an increased oxidative burden which in turn, may potentially translate into hepatic damage, cirrhosis and hepatitis (Valko et al. 2007; Vrba and Modriansky 2002).
Since ancient days, plant-derived natural products have been used extensively for their medicinal properties, as well as in the form of culinary ingredients and nutritional supplements. Owing to their vast spectrum of dietary values including vitamins, minerals, phenolics, antioxidant and enzymes, plant materials have asserted significant contributions to the medicinal, nutraceutical, and food industries. Eventually, numerous research studies into the hepatoprotective properties have been conducted from different medicinal plants and herbal preparations, for instance, Colocasia esculenta (Chinonyelum et al. 2015a), Spirulina maxima (Alvari et al. 2012), Eclipta alba (Bedi et al. 2016), Boehmeria nivea (Singh et al. 2010a), Cichorium intybus (Sultana et al. 1995), Picrorhiza kurroa (Thyagarajan et al. 2002), Mangifera indica (Hiraganahalli et al. 2012), Litchi chinensis (Sagar et al. 2014). Moreover, recent studies have reported that polyherbal preparation from the aqueous extracts of different plants including Berberis vulgaris L., Cucumis sativus L., Portulaca oleracea L., Rheum palmatum L. showed promising anti-hepatotoxic effects while used as dietary supplement (Sarhadynejad et al. 2016). Another study reported that a polyherbal hepatoprotective formulation (PHF) containing spray-dried aqueous extracts of Andrographis paniculata Nees., Phyllanthus niruri Linn., Phyllanthus emblica Linn., provided promising hepato-protection owing to the combined activities of the plants (Tatiya et al. 2012). Additionally, approximately 170 phytoconstituents isolated from 110 medicinal plants distributed among 55 families have been reported to exhibit hepatoprotective activities. Nearly 600 commercial herbal supplements are also being marketed worldwide with reported hepatoprotective efficacy. In South Asia, more than 93 medicinal herbs are used in various combinations for the preparation of forty polyherbal formulations. Nevertheless, just a limited number of hepatoprotective herbs as well as their dietary formulations are being endorsed into the conventional medicines due to their safety and efficacy profile (Girish and Pradhan 2017; Stickel and Schuppan 2007).
In this comprehensive review, nine ethnomedicinally significant plant species named Colocasia esculenta, Alstonia scholaris, Mangifera indica, Hypericum japonicum, Kalanchoe pinnata, Leucas aspera, Litchi chinensis, Eclipta prostrate and Hybanthus enneaspermus, which are being widely used for their hepatoprotective properties, were reviewed covering their distribution, ethnomedicinal significance, hepatoprotective phytoconstituents, and therapeutic potentials in alleviating oxidative and hepatic stress. Although a significantly larger number of plant species have been attributed with hepatoprotective potentials, the selection was established through considerations of their formulation into advanced formulations and subsequent integration into modern medicinal systems. The collected information were also critically reviewed in order to present insights and recommendations for future studies with the ultimate aim of establishing these plants as possible sources of new hepatoprotective herbal preparations.
Methodology
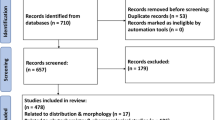
Electronic databases viz. Google Scholar, PubMed, Scopus, ScienceDirect, ACS publications, Willey online library and SpringerLink, were explored extensively using keywords including “South Asian medicinal plants” “Colocasia esculenta”, “Alstonia scholaris”, “Mangifera indica”, “Hypericum japonicum”, “Kalanchoe pinnata”, “Leucas aspera”, “Litchi chinensis”, “Eclipta prostrate”, “Hybanthus enneaspermus”, “traditional uses”, “ethnomedicinal uses”, “bioactive metabolites”, “hepatoprotective activity” and “toxicological study”. Eventually, relevant literatures published prior to October 2020 were collected, curated and critically evaluated in order to extract necessary information. The recognized accepted plant names and their respective synonyms were validated according to The Plant List (2013). The chemical structures of different phytochemicals were illustrated in accordance with PubChem with the help of ChemDraw Ultra 15.0.
Distribution and ethnomedicinal applications
Throughout the history of the Indian subcontinent, records of various ethnomedicinal practices have been abundant which have managed to remain relevant and effective to this day. Different traditional medicinal systems including the Ayurveda, Unani, Homeopathy and Shiddah have attained significant institutional recognitions and are contributing to the healthcare system to an outstanding extent comparable to the modern system of medicine. Moreover, around 40–50 million people from the rural areas of the subcontinent are still primarily dependent on these systems for their healthcare (Mazid et al. 2012). This review has mainly focused on medicinal plants (Fig. 1) which have experienced extensive utilizations under different ethnomedicinal systems of South Asia, especially for their hepatoprotective potentials. However, a majority of them are distributed worldwide and are recognized for their contribution to the regional medicinal systems as well as the culinary cultures. Therefore, the relevant general information of these plants including their accepted scientific names, recognized synonyms, complete taxonomical classifications, geographical distribution patterns and common local names (mainly within the subcontinent) have been summarized in Table 1. Moreover, based on extensive literature review on different parts (leaves, stem, bark, rhizome, roots, flowers and fruits) as well as the phytochemistry of the nine species under discussion, their ethnomedicinal significance have been enumerated in Table 2.
Phytochemistry
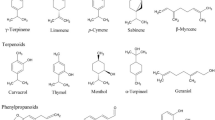
With the blessings of urbanization and modern technology, the crude extracts as employed in the traditional medicinal systems are now being harnessed for exact bioactive molecules contributory to their respective bioactivities. The secondary metabolite pool of the plants not only act as the principal source of these bioactive molecules, but also provide humankind with a continuous stream of significant structural diversity to work with (Saxena et al. 2013). Such molecules, in turn have illustrated significant contribution either directly as the drug molecule or indirectly as the lead compound, in the treatment of a wide variety of diseases. Furthermore, specific classes of compounds have been shown to be consistent in exhibiting specific types of pharmacological potentials viz. hepatoprotective activity of phenolics, flavonoids and tannins (Aneja et al. 2013; Rehman et al. 2015), anti-inflammatory property of flavonoids (Olaokun et al. 2017), antioxidative potential of polyphenols (Zhang et al. 2015), and antiproliferative properties of polyphenols and flavonoids (Saxena et al. 2013). The plants under discussion have been illustrated with a wide variety of secondary metabolites covering major phytochemical classes including alkaloids, flavonoids, glycosides, oils and fats, gums, terpenoids, steroids and vitamins. The major bioactive metabolites isolated from these plants with prominent hepatoprotective potentials include schaftoside, echinocystic acid and eclalbasaponin II (Fig. 2). Moreover, thirteen polyphenolic and flavonoid molecules including catechin, epicatechin, kaempferol, quercetin, quercitrin, isoquercitrin, anthocyanins, procyanidin A2, quercetin-7-O-rhamnoside, pelargonidin-3-O-glucoside, quercetin 3-O-rutinoside-7-O-α-l-rhamnoside, gallic acid and hyperin have been chemically characterized as the major phytoconstituents of different extracts from these plants which have been found to exert noteworthy hepatoprotective activities.
Pharmacological properties
All the nine species selected in this review possess diverse pharmacological potentials including significant hepatoprotective properties with traditional uses. The plants both as whole and individual parts (leaves, stems, roots, rhizomes) have been investigated substantially through in-vitro assays and in-vivo experimentations in order to evaluate the extent of hepatoprotective potential, to ascertain the responsible phytochemicals and to enumerate their apparent pharmacology as well as respective mechanisms. Such information has been elaborated in the following sub-sections and summarized in Table 3.
Colocasia esculenta (L.) Schott
C. esculenta have been recognized as a traditional remedy owing to its hepatoprotective properties which have been further validated through pharmacological studies. The methanol extract of the aerial parts of C. esculenta have been reported to reverse iron-induced hepatotoxicity in Swiss albino mice to a significant extent, indicating potent hepatoprotective property. The extract at a dose of 200 mg/kg body weight, suppressed iron-induced elevated serum concentrations of alanine transaminase (ALT) and aspartate transaminase (AST) by 41.7% and 50.6%, respectively, compared to the standard desirox (20 mg/kg body weight) which suppressed the enzymes by 47.7% and 52.5%, respectively. The extract also potentiated hepatic antioxidants viz. superoxide dismutase (SOD), catalase, glutathione-S-transferase (GST) and reduced glutathione (GSH) by 289.6%, 103.8%, 144.1% and 20.3%, respectively. Furthermore, the hepatoprotective potential of the extract was attributed to its capacity to neutralize iron through chelation and reduction. Interestingly, microscopic examination of mice liver sections stained with hematoxylin and eosin at 400× zoom, showed a significant reduction in hepatocellular necrosis and increase in the number of hepatocyte cells. This, in turn, suggested the possible efficacy of the extract in reversing any metal overload-based hepatotoxicity which should be subjected to future investigation. However, such justification also challenges the hepatoprotective potential of the extract in case of any chemically induced hepatotoxicity (Saikia et al. 2018a, b). Recent in-vivo investigation of the aqueous extract of the leaves in thioacetamide-induced male Wistar rats demonstrated remarkable hepatoprotective activity. The extract at the dose of 250 mg/kg reversed the hepatotoxicity-associated elevation of ALT, AST and alkaline phosphatase (ALP) activities by 33.2%, 47.4% and 20.9%, respectively, compared to the standard silymarin exerting 60%, 64.8% and 21.8% suppressions of the enzymes, respectively, at a dose of 100 mg/kg body weight. The extract also maintained the regular level of serum albumin against hepatotoxic reduction of the same. (Chinonyelum et al. 2015a). Schaftoside available in C. esculenta has been demonstrated to attenuate paracetamol-induced hepatotoxicity in mice at doses of 40, 80 and 160 mg/kg. Intracellular investigation revealed that the compound was capable of activating the farnesoid X receptor (FXR) in hepatocytes which, in turn, potentiated the hepatic antioxidative system and diminished the generation of pro-inflammatory eicosanoids as well as the activation of nuclear factor kappa B (NF-κB) signaling pathway (Guo et al. 2010; Liu et al. 2020a, b). The leaf juice of the plant rich in anthocyanins was evaluated for its hepatoprotective potential through the administration of 5 µl/ml and 10 µl/ml of the extract in in-vitro liver slice method. The extract boosted the activities of ALT and AST in liver while restricting their availability in plasma (Patil et al. 2011). All of these experimental demonstrations are testament to the powerful hepatoprotective activity of the plant as projected by its ethnomedicinal claims. However, further in-depth and more focused investigations following the known hepatotoxicity-associated biochemical pathways, are warranted. Although many bioactive isolates have been reported from this plant, only one compound was characterized with hepatoprotective activity. Eventually, other phytochemicals from the plant should be investigated for their hepatoprotective potentials along with the characterization of their exact pharmacological and biochemical responses. Moreover, any clinical study is yet to be attempted for the assessment of its capacity to maintain optimum liver function in the presence and absence of hepatotoxic inducers. Therefore, this systematic review suggests pharmacokinetics study followed by clinical investigation of its potential for hepatoprotection.
Alstonia scholaris (L.) R. Br.
A. scholaris have been characterized with a diverse range of pharmacological activities including anti-inflammatory, anticoagulant, and antidepressant (Khan et al. 2020), anti-asthmatic (Shang et al. 2010), antibacterial and synergistic (Wang et al. 2016), anti-proliferative (Wang et al. 2017), antidiabetic and antihyperlipidemic (Arulmozhi et al. 2010), anti-arthritic and antioxidant activities (Arulmozhi et al. 2011). Apart from these, prominent hepatoprotective activity has also been demonstrated in favor of this plant in agreement with its ethnomedicinal claims. A study investigated hepatoprotective potential of the methanol extract of A. scholaris in carbon tetrachloride-, β-d-galactosamine- and paracetamol-induced hepatotoxic model in male Wistar rats. The extract at the dose of 300 mg/kg body weight suppressed the hepatotoxicity-induced enhancements of ALT (80.7%, 80.9% and 97.1%, respectively) and AST (77.4%, 33.0% and 82.5%, respectively) plasma levels in all three models. It was evident through histopathological analysis that A. scholaris-administered cells showed minimum inflammatory infiltration and microvascular cell degeneration while also reducing cellular necrosis (Lin et al. 1996a, b, c). Another in-vivo study in carbon tetrachloride-induced Swiss albino mice further reinforced this claim as methanol extract of the stem barks (dose of 200 mg/kg body weight) reduced plasma concentrations of ALT, AST, ALP and bilirubin by 42.2%, 12.3%, 45.7% and 18.3%, respectively, compared to standard silymarin (25 mg/kg body weight) which exhibited 61.7%, 27.2%, 61.4% and 29.6% reductions, respectively. In the pathological examination, the extract-treated liver cells showed a low number of damaged hepatocytes and fatty degeneration (Kumar et al. 2012a). Similarly, the ethanol extract of the fruits of this plant at the dose of 300 mg/kg body weight was demonstrated to suppress plasma concentrations of ALT, AST, ALP and bilirubin in albino rats by margins of 32.6%, 26.1%, 65.5% and 50.8%, respectively (Shankar et al. 2012). Although the hepatoprotective activity of A. scholaris has been substantiated by few studies, any attempt on the identification of the responsible bioactive molecule is yet to be reported. Hence, extensive studies are still needed to assure its hepatoprotective potential in terms of individual phytochemicals. Furthermore, thorough clinical studies are also required to strengthen its traditional application and establish its stature as a suitable hepatoprotective agent.
Mangifera indica L.
From an ethnomedicinal perspective, M. indica is one of the most widely used plant used for its for hepatoprotective properties in the rural areas of South Asian countries (Shah et al. 2010). Extracts of different parts of the plant including stem, leaves, aerial parts, fruits and pulps have been subjected to hepatoprotective investigation against the synthetic compound silymarin (Ediriweera et al. 2017). (Pourahmad et al. 2010) claimed that, the aqueous extract of the fruits was capable of reversing cumene hydroperoxide-induced oxidative stress-mediated hepatotoxicity in male Sprague–Dawley rats. Further biochemical characterization illustrated reduced rates of reactive oxygen species (ROS) generation, lipid peroxidation, hepatocyte lysis and intracellular glutathione depletion. Another in-vivo study investigated the aqueous extract of the stem barks of M. indica for hepatoprotective potential at the doses of 125, 250 and 500 mg/kg body weight in male Wistar rats. The hepatoprotective properties were assessed both in pre-treatment and post-treatment models where the extract was administered before and after the administration of 30% carbon tetrachloride in olive oil, respectively. In pre-treatment model, the extract at the doses of 250 and 500 mg/kg body weight produced comparable effects as the standard ascorbic acid (10 mg/kg) as they prominently suppressed ALT (58.0%, 72.6% and 58.2%, respectively), AST (72.4%, 77.9% and 67.6%, respectively), ALP (62.1%, 57.0% and 37.2%, respectively) and total bilirubin (52.9%, 48.1% and 29.6%, respectively). The extract at both doses as well as the standard also elevated hepatic concentrations of SOD (110.9%, 148.5% and 37.1%, respectively), catalase (107.1%, 162.1% and 23.2%, respectively), GSH (149.6%, 260.8% and 42.4%, respectively) and diminished hepatic concentration of malondialdehyde (MDA) (71.1%, 89.5% and 78.9%%, respectively) significantly. A similar trend was observed in the post-treatment model for both the plasma and hepatic markers (Adeneye et al. 2015). Another paracetamol-induced hepatotoxic study model in male Wistar albino rats demonstrated the hepatoprotective properties of both the ethanol and aqueous extract of the stem barks. Both the extracts at a dose of 200 mg/kg body weight reversed paracetamol-induced elevation of ALT, AST and ALP whereas the hepatic concentrations of antioxidants viz. SOD, catalase and GSH were remarkably improved (Omotayo et al. 2015). Similarly, both the methanol and ethanol extract of M. indica leaves (25 and 50 mg/kg body weight) were reported to suppress plasma ALT and AST and to cause hepatic enhancements of SOD, catalase, GST and glutathione peroxidase (GPx) in mercuric chloride-induced male Swiss albino mice, indicating prominent hepatoprotective capacities (Adewusi and Afolayan 2010; Karuppanan et al. 2014). An in-vivo carbon tetrachloride-induced hepatotoxic model in male Wistar albino rats demonstrated that the acetone extract of the fruit pulp of M. indica at the doses of 250 and 500 mg/kg body weight, was capable of elevating catalase activity and reducing the extent of lipid peroxidation, compared to the standard silymarin (25 mg/kg) (Singh et al. 2010b). The polysaccharide content from the pulp of unripe fruits of M. indica was investigated for its potential anti-hepatotoxic activity against cyclophosphamide-induced liver damage in male albino rats. Compared to the standard silymarin (150 mg/kg body weight), the polysaccharide extract administered at doses of 500 and 1000 mg/kg body weight, significantly diminished plasma concentrations of ALT (40.4%, 44.7% and 47.5%, respectively) and AST (43.0%, 36.3% and 19.4%, respectively). Furthermore, the extract also enhanced hepatic levels of SOD, GST and GSH while diminishing hepatic MDA concentration. Liver tissue sections stained with hematoxylin and eosin were compared with control group tissues. The oral administration of MPS extract improved the hepatic architecture when compared to the control group, apparently indicating the regeneration of liver cells (Fahmy et al. 2016; Vargas-Mendoza et al. 2014). However, the study illustrated enhancement of plasma ALP both in the presence of the standard and the extracts which is quiet contradictory to positive hepatoprotective activity. Any hepatoprotective agent is ought to suppress the plasma ALP level parallel to plasma ALT and AST levels.
Although, several studies have been conducted on the activity of this plant, hepatoprotective properties have been characterized for different extracts only. Therefore, major hepatoprotective isolates need to be identified and elaborative studies need to be performed to find out the cellular mechanism on systemic level.
Hypericum japonicum Thunb.
H. japonicum is distributed throughout the Asia and some parts of Europe. The plant has an extensive history of being utilized for ethnomedicinal purposes. Phytochemical investigations into this plant have afforded a wide variety of bioactive molecules which have been further characterized with prominent pharmacological potentials through appropriate studies. Eventually, the hepatoprotective properties of the plant have also been traced to individual secondary metabolites (Liu et al. 2014a). The hepatoprotective effects of the total aqueous extract of H. japonicum and its different fractions were investigated against carbon tetrachloride-induced hepatitis and α-naphthyl-isothiocyanate-induced cholestasis in Kunming (KM) mice. The study demonstrated that, the total aqueous extract as well as the aqueous fraction at doses of 0.5, 1.5 and 4.5 g/kg body weight suppressed several serum markers in both models following a dose-dependent manner. In carbon tetrachloride-induced hepatotoxicity, the standard biphenyldicarboxylate (200 mg/kg body weight) reduced the plasma concentration of ALT and AST by 69.2% and 29.7%, respectively. Comparably, both the aqueous extract and fraction at the dose of 4.5 g/kg, reduced plasma ALT by 63.0%, 66.7%, respectively and plasma AST by 53.8%, 51.4%, respectively. Similarly, in the α-naphthyl-isothiocyanate-induced cholestatic model, standard Yin-Zhi-Huang oral solution at the dose of 15 ml/kg diminished total bilirubin and ALT levels in plasma by 34.4% and 27.8%, respectively, whereas the aqueous extract and fraction (4.5 g/kg) suppressed total bilirubin by 60.2%, 62.6%, respectively, and plasma ALT by 54.0%, 56.0% respectively (Wang et al. 2008). The ethanol and ethyl acetate extracts of the plant were also demonstrated to suppress d-aminogalactose-induced elevation of ALT and AST at the doses of 0.2, 0.6 and 1.8 g/kg body weight (Su et al. 2016). The total flavonoid extract of the plant was investigated for its hepatoprotective potential against carbon tetrachloride-induced hepatic injury where it potentiated SOD, GSH and MDA in hepatic tissue. Chromatographic analysis into the extract had revealed quercetin, kaempferol, quercitrin, isoquercitrin, hyperin and quercetin-7-O-rhamnoside as the major flavonoid constituents (Liu et al. 2014a; Wang et al. 2009). On a separate study, quercetin and its glycoside rutin (quercetin-rutinoside) were subjected to an in-vivo study involving male BALB/cN mice. Both the compounds were demonstrated to reverse carbon-tetrachloride-induced elevation of serum ALT and AST as well as the hepatotoxic reduction of SOD and GSH levels. Rutin at the dose of 150 mg/kg body weight suppressed serum ALT and AST levels by 87.3% and 93.1%, respectively, and elevated hepatic SOD and GSH levels by 67.9% and 56.8%, respectively. On the other hand, quercetin at the dose of 50 mg/kg body weight enhanced hepatic SOD and GSH levels by 76.5% and 70.3%, respectively, and diminished serum ALT and AST by 25.3% and 50.3%, respectively (Domitrović et al. 2012). Since pharmacokinetic profiling of these phytochemicals has already been established (Wang et al. 2009), clinical studies in the future is definitely warranted in order to evaluate their therapeutic potential.
Kalanchoe pinnata (Lam.) Pers.
The hepatoprotective potentials of the fresh juice and the ethanol extract of K. pinnata leaves were investigated against carbon tetrachloride-induced hepatotoxicity in-vitro and in-vivo. In-vitro assay involving rat hepatocyte culture revealed more prominent hepatoprotective activity in favor of the fresh juice concentrate (10 µL) than the ethanol extract (10 µL) as they suppressed plasma ALT by 52.7%, 29.3%, respectively, and plasma AST by 34.7%, 22.8%, respectively. The similar pattern was reflected by the in-vivo experimentation in Wister albino rats as both the samples (200 mg/kg body weight) suppressed serum concentrations of ALT (68.8%, 60.5%, respectively), AST (25.0%, 14.3%, respectively), ALP (37.7%, 23.8%, respectively) and total bilirubin (52.1%, 24.2%, respectively). Additionally, when subjected to histopathological analysis, extract-treated liver cells of rats intoxicated with carbon tetrachloride appeared to be slightly unclear as in normal hepatocytes. However, compared to the carbon tetrachloride damaged ones, the number of hepatocytes with normal nucleus was much higher (Adewusi and Afolayan 2010; Yadav and Dixit 2003). Methanol extract of K. pinnata leaves along with its ethyl acetate and butanol fractions exhibited potent anti-viral activities in-vitro against hepatitis C virus (HCV) as evident from their IC50 values of 17.2, 9.3 and 7.1 µg/mL, respectively. Further investigation involving isolated secondary metabolites viz. quercetin, gallic acid and quercitrin revealed prominent anti-HCV activities in favor of the first two with IC50 values calculated at 1.5 and 6.1 µg/mL, respectively (Aoki et al. 2014) Further in-vivo investigations are necessary so as to ascertain their efficacy in the treatment of hepatitis C. Moreover, with more than 100 compounds isolated from the plant, prospective pharmacological studies of the isolated compounds can provide supportive evidence to confirm exact therapeutic efficacy hereafter for next step clinical investigation.
Leucas aspera (Willd.) Link
L. aspera, commonly known as ‘Thumbai’ is extensively utilized by the ethnomedicinal healers of Himalayans regions of Southeast Asia for providing hepato-protection. Alongside other biological activities, its hepatoprotective potential has also been explored scientifically (Prajapati et al. 2010). The possible effect of the aqueous extract of L. aspera was investigated against d-galactosamine-induced hepatotoxicity in female Wistar albino rats. The extract at the dose of 400 mg/kg body weight suppressed pathological elevation of ALT, AST, ALP and total bilirubin by 35.5%, 60.9%, 54.5% and 50.0%, respectively, compared to the standard silymarin (100 mg/kg) which diminished the same markers by 40.4%, 68.2%, 62.5% and 61.9%, respectively. Furthermore, the extract as well as the standard also potentiated hepatic antioxidative enzymes including SOD (256.0%, 238.8%, respectively), catalase (152.9%, 134.6%, respectively) and GPx (102.2%, 80.4%, respectively) while diminishing the rate of hepatic lipid peroxidation (50.4%, 46.0%, respectively) (Banu et al. 2012). Another study revealed the hepatoprotective properties of the methanol extract of the plant in carbon tetrachloride-induced male Wistar rats as the extract at a dose of 100 and 200 mg/kg reduced plasma concentrations of ALT, AST and ALP significantly. The extract at both doses also effectuated comparable level of enhancements as the standard silymarin (50 mg/kg) to the levels of hepatic antioxidants including SOD (21.4%, 82.0% and 65.5%, respectively), catalase (26.7%, 91.7% and 69.0%, respectively), GST (300.0%, 485.7% and 328.6%, respectively), GSH (259.1%, 384.1% and 356.8%, respectively) and GPx (65.2%, 140.5% and 78.9%, respectively). When compared to the carbon tetrachloride-treated group, the pre-treatment animals administered with plant sample and reference drug showed promising protection from carbon tetrachloride-induced liver damage as evident from the prevalence of improved hepatic architectural pattern (Latha et al. 2012). The hydroalcoholic (70:30) extract of the leaves of L. aspera was investigated for potential hepatoprotective activity in lead acetate induced-male Wistar albino rats. After 21 days of daily extract administration (400 mg/kg body weight), significant reductions of plasma ALT, AST and ALP concentrations by 27.4%, 20.9% and 9.3%, respectively, was indicative of noteworthy anti-hepatotoxic activity (Thenmozhi et al. 2013). Since any pharmacological study is yet to be illustrated involving the isolated phytochemicals, future in-vivo and in-vitro investigations are strongly recommended using fractions and bioactive isolates. Furthermore, detailed biomolecular characterizations are also necessary to ascertain the particular mechanism of action.
Litchi chinensis Sonn.
L. chinensis is a popular plant of the South Asian region whose leaves, fruits and seeds have experienced extensive traditional applications against a wide variety of pathological conditions including hepatotoxicity. Concentrate of the fresh juice of fruit pulps of two varieties of the plant named Chakapat and Gimjeng were evaluated for their potential hepatoprotective effects against carbon tetrachloride-induced liver damage in male Sprague–Dawley rats at the doses of 100 and 500 mg/kg body weight. The concentrates were also characterized with the presence of ascorbic acid, trans-cinnamic acid and pelargonidin-3-O-glucoside as the major phytochemical constituents. Earlier investigation revealed that polyphenolic compounds of litchi leaf augment kidney and heart functions in 2K1C rats (Mamun et al. 2020). However, following the carbon tetrachloride administration both the concentrates were able to reverse hepatotoxic elevation of plasma ALT, AST and ALP levels as well as the rate of hepatic lipid peroxidation to significant extents as compared to the standard silymarin (100 mg/kg). According to histopathological analysis, animals’ pretreatment with plant extract resulted in lesser extent of pathological damage in their livers. In carbon tetrachloride-intoxicated rats, histopathologic changes included centrilobular damage, including Kupffer cell hyperplasia. Moreover, elevated level of serum hepatic markers, extent of apoptosis, and centrilobular damage in rat livers as caused by carbon tetrachloride, were significantly restored by pretreatment with plant extract (Bhoopat et al. 2011). Another study demonstrated that the phenolic extract of the fruit pulp of L. chinensis was capable of exerting prominent dose-dependent (50, 100 and 200 mg/kg body weight) hepato-protection against physical stress-induced liver damage in male Kunming mice. The extract at the dose of 200 mg/kg enhanced the hepatic activities of SOD, catalase, GSH and GPx by 19.0%, 6.0%, 107.2% and 18.5%, respectively. The extract also significantly diminished plasma ALT and AST levels indicating potent hepatoprotective properties. Eventually, chromatographic investigation into the phenolic extract with the help of HPLC revealed quercetin 3-O-rutinoside-7-O-α-l-rhamnoside, rutin and (−)-epicatechin as the major bioactive components. The microscopic examination of animal mitochondria demonstrated that nearly all the mitochondria became blue-green in color in the normal control group animals. The restraint-stressed group had significantly fewer blue-green mitochondria than the usual control group. After pretreatment with lychee pulp extract, the number of blue-green mitochondria which dropped in response to restraint stress, was partially and dose-dependently restored (Su et al. 2016). As mentioned earlier, both quercetin and rutin have been individually characterized with prominent hepatoprotective potential in-vivo. Animals pretreated with the bioactive compound rutin at different doses were examined for histopathological changes. The doses of 50 mg/kg showed a markedly reduced size of the hepatic necrotic areas. Notably, at the higher dose (150 mg/kg), there was a complete reversal of carbon tetrachloride-induced hepatocellular damage (Domitrović et al. 2012). A recent study illustrated that the methanol extract of L. chinensis fruit pulp improved in-vitro cellular viability of BNL hepatocytes to a greater extent than standard silymarin. Furthermore, bioactivity-guided phytochemical investigation into the extract afforded epicatechin and procyanidin A2 as the major polyphenolic constituents. The hepatoprotective effect of the extract was also replicated in-vivo in carbon tetrachloride-induced male ICR mice at the doses of 20, 100 and 200 mg/kg body weight. At the end of 3rd week of administration, the extract at the dose of 100 mg/kg diminished plasma levels of ALT and AST by 78.5% and 77.6%, respectively. However, the effect was found to be abrupt, inconsistent and even reversed in some cases for the dose of 200 mg/kg and at the end 6th week, thus limiting the efficacy of the extract within certain dose and time period. During histopathological examinations performed at × 40 zoom, the number of lipid droplet holes or voids was reduced in the high-level LPE group compared to all other groups. In all treatment groups, the hexagonal portal area generated by aligning hepatocyte edges were preserved. The LPE group with the higher doses had fewer eosinophilic infiltrations than the other groups. The portal vein area of the intermediate and high-level LPE groups had less macro steatosis than the other groups (Chen et al. 2017a, b). Another study demonstrated a similar pattern of hepatoprotective potential in favor of the aqueous extract of the its flowers as the extract was capable of reversing high calorie diet-induced elevation of plasma ALT, AST and hepatic cytokines (viz. tumor necrosis factor-α, interleukin-1β and interleukin-6) as well as plasma concentrations of triacylglycerol and cholesterol in male Wistar rats (Park et al. 2007; Wu et al. 2013). Future pharmacological studies and pharmacokinetic profiling are necessary for the major bioactive molecules including epicatechin, procyanidin A2 and pelargonidin-3-O-glucoside, available in the fruit pulp of L. chinensis as well as the major phytoconstituents of the flower extract viz. gentistic acid, catechin, epicatechin and proanthocyanidins, in order to ascertain their individual potential as hepatoprotective agents.
Eclipta prostrata (L.) L.
E. prostrata is an important ethnomedicine mainly used in the Uttar Pradesh of India and few other South Asian countries for treating different diseases, especially a wide range of bacterial infection and liver damage (Khan and Khan 2008). Carbon tetrachloride-, paracetamol- and d-galactosamine-induced hepatotoxic model in male ICR mice was treated with the aqueous extract of the plant at a dose of 300 mg/kg body weight and the hepatoprotective potentials were evaluated based on plasma ALT and AST levels as well as subsequent histopathological changes. Although significant levels of ALT and AST suppressions were achieved in the carbon tetrachloride- and d-galactosamine-induced mice, the same was not observed for the paracetamol-induced model. As seen in the microscopic images, post-treatment of carbon tetrachloride-intoxicated mice with E. prostrata greatly reduced the severity of the histopathological lesions (sub massive centrilobular necrosis, ballooning degeneration, and cellular infiltration in the liver) (Lin et al. 1996a, b, c). Thus, further biochemical analyses are necessary in order to identify the exact underlying mechanisms leading to the hepatoprotective activities. Another study investigated the ethanol extract of E. prostrata leaves for its hepatoprotective potential in alcohol induced-male Wistar albino rats. The extract at the dose of 200 mg/kg body weight elevated the concentrations of hepatic antioxidants namely SOD, catalase, GSH and GPx by 124.7%, 51.7%, 111.0% and 113.7%, respectively, compared to the standard silymarin (2.5 mg/kg) which enhanced the same markers by 28.5%, 31.2%, 77.9% and 72.3%, respectively. The extract as well as the standard was also reported to increase plasma concentrations of vitamin E (128.1% and 56.1%, respectively) and vitamin C (118.5% and 66.2%, respectively) which are the first line of antioxidative defense of the body (Arun and Balasubramanian 2011; Lin et al. 1996a, b, c). This, in turn, was suggestive of the fact that the hepatoprotective property of the extract could be attributed to its capacity to act as antioxidants itself in neutralizing the toxic metabolites. A later in-vitro study identified bioactive triterpenoids from the methanol extract of the aerial parts of E. prostrata named echinocystic acid and eclalbasaponin I–III and V, which were then evaluated for their potential anti-fibrotic activities in rat hepatic stellate cells (HSCs) containing solution. Echinocystic acid and eclalbasaponin II was reported to exert prominent time- and dose-dependent antiproliferative effects over the T6 cell line which was further linked to their potential to suppress hepatic fibrosis in vivo (Lee et al. 2008a; Rathore et al. 2014a, b). However, such in-vivo studies in appropriate animal models are warranted in future to ascertain their hepatoprotective potential in biological systems. Moreover, biochemical characterization of respective plasma and hepatic markers are also required for the illustration of underlying mechanisms.
Hybanthus enneaspermus (L.) F. Muell.
Hepatoprotective properties of the ethanol extract of H. enneaspermus leaves was demonstrated against paracetamol-induced hepatotoxicity model in adult male albino rats. The extract at the dose of 200 mg/kg body weight diminished plasma concentrations of ALT, AST and ALP by 23.1%, 13.2% and 17.7%, respectively. Furthermore, the extract also potentiated hepatic antioxidative enzymes named SOD, catalase, GST, GPx and glutathione reductase (GR) to extents of 24.4%, 52.7%, 41.1%, 6.7% and 155.8%, respectively, while decreasing hepatic lipid peroxidation by 19.5%. In paracetamol-treated mice, histological examinations revealed significant necrosis with the loss of nuclei. In the experimental animals treated with plant extract, all of these alterations were reduced dramatically as normal hepatic architecture, normal hepatic central vein, regular hepatocytes with nuclei, and sinusoidal gaps were observed predominantly (Bhanu et al. 2011). In another study, aqueous extract of H. enneaspermus at the doses of 200 and 400 mg/kg body weight was investigated for potential hepatoprotective activities against carbon tetrachloride-induced male Wistar rats through both pre-treatment and post-treatment models. In the later model, the extract at both doses as well as the standard silymarin (100 mg/kg) suppressed plasma levels of ALT (70.3%, 78.7% and 84.9%, respectively), AST (43.5%, 56.6% and 68.9%, respectively), ALP (39.5%, 54.7% and 61.0%, respectively) and total bilirubin (45.8%, 79.2% and 79.2%, respectively) significantly. The hepatoprotective potential of the extracts followed a similar pattern in the pre-treatment model as well. Furthermore, in histological investigation, carbon tetrachloride-treated rat liver sections showed massive changes throughout the lobules, including fatty accumulations, cellular distensibility, and necrosis, as well as dilation of Disse spaces with focal disruption of the sinusoidal endothelium, inflammatory incursions of the portal triads, and distortion of the central venules. Animals treated with an aqueous extract of H. enneaspermus and the control showed lower hepatic vacuolation and better maintenance of normal liver architecture, as well as moderate hepatocyte plate disorganizations and smaller dilations of interstitial spaces. In the hepatic lobules of the treated animals, periportal inflammatory infiltrates were infrequent or absent (Vuda et al. 2012a, b). In order to validate and reinforce these initial findings, more in-vivo studies involving the extract, their subsequent fractions as well as isolated phytochemicals are required. In addition, extensive molecular experimentation on diverse hepatocytic cell lines is also warranted to affirm the exact mechanism of action.
Safety and toxicity
Although a large number of pharmacological investigations have enumerated the hepatoprotective potentials of the nine selective plants, safety profiling and relevant toxicological investigations have not been conducted for all these species extensively. A study investigated the acute toxicity of Colocasia esculenta aqueous extract in female Wistar rats. The extract at the maximum dose of 4000 mg/kg body weight maintained normal levels of plasma markers viz. ALT, AST, creatinine, cholesterol and triglycerides indicating an absence of toxicity. However, in the sub-acute toxicity study, the extract at the dose of 800 mg/kg enhanced hepatic AST in female while diminishing the same in male rats at the end of twenty days. Moreover, the extract also suppressed platelet count in female rats only, therefore limiting the continuous administration of the extract at larger doses (Nzebang et al. 2018). Methanol extract of the leaves and stems of Alstonia scholaris administered in female Sprague Dawley rats at the maximum dose of 2000 mg/kg body weight demonstrated the absence of any observable toxicity rendering a safer profile in favor of the extract. In sub-acute toxicity test, both male and female rats exhibited signs of toxicities in the form of lethargy, diminished motor reflexes, heavy breathing and fur loss after continuous administration of the extract at the doses of 500 and 1000 mg/kg body weight for at least 14 days straight. The toxicity was also translated at organ level as the weight of lungs decreased in both male and female whereas weight of liver diminished only in male (Bello et al. 2016). A 90 days long oral toxicity study of Mamgifera indica involving repeated doses of 2000 mg/kg body weight revealed that the experimental mice did not show any adverse effect or death (Reddeman et al. 2019). Correspondingly, another study reported that the administration of the aqueous extract of stem bark were found to exert no adverse or lethal reactions in Sprague Dawley rats at the doses of 2000 mg/kg. The extract was also found to be non-irritant towards skin, ocular and renal mucosa following single dose administration in rabbits (Garrido et al. 2009). Although the aforementioned study revealed relative safety for three species under limited doses, these data are very still insufficient in terms of establishing absolute safety for all these plants. Thus, further comprehensive toxicological studies are warranted taking into account all plants fractions and their active bioactive metabolites.
Conclusion and future prospects
Herbal medicines have the potential to offer an effective mean towards the treatment of liver diseases. The present comprehensive review was focused on nine selective South Asian herbs which have extensive traditional applications based on their hepatoprotective potentials. The effects of these plants at cellular levels which lead to their hepatoprotective effects have been converged and depicted in Fig. 3 and the effects of herbal medicines in the treatment of hepatotoxicity have been illustrated in Fig. 4. The primary obstacle towards the utilization of these plants in the preparation of hepatoprotective formulations can be referred to the unavailability of sufficient safety reports at acute, sub-acute and chronic levels. Therefore, toxicological studies into these plants in terms of cellular, hepatic and hematological markers are necessary on an extensive scale. Secondarily, a relative evaluation of these plants should be attempted in identical experimental animal model addressing individual plant-based as well as poly-herbal formulations. Although hepatoprotective properties of different plant extracts have been illustrated at biochemical level, the information is still insufficient as single or multiple relevant markers are yet to be explored in some of the plants. A comparative investigation should allow for the evaluation of their hepatoprotective properties based on all relevant markers and might also lead to the designing of a more efficient poly-herbal formulation with the presence of individual plants in relatively minor quantities where individual plant-associated toxicities could be minimized completely. Finally, identification of bioactive molecules from these plants must be undertaken in future followed by pharmacological evaluation of the promising molecules for hepatoprotective activities. The availability of modern hepatoprotective drugs with realistic clinical utility is still very limited and identification of new molecules with similar potentials will surely advocate the process of novel drug discovery as well as development.
Change history
27 July 2022
Missing Open Access funding information has been added in the Funding Note
Abbreviations
- ACS:
-
American Chemistry Society
- ALP:
-
Alkaline phosphatase
- AAT:
-
Alpha-1 antitrypsin
- ALT:
-
Alanine transaminase
- AST:
-
Aspartate transaminase
- CYP450:
-
Cytochromes P450
- CAT:
-
Catalase
- FXR:
-
Farnesoid × receptor
- GSH:
-
Reduced glutathione
- GPx:
-
Glutathione peroxidase
- GST:
-
Glutathione-S-transferase
- HSCs:
-
Hepatic stellate cells
- HPLC:
-
High-performance liquid chromatography
- HepaRG:
-
Hepatic stem cell line
- HepG2:
-
Human liver cancer cell line
- HCV:
-
Hepatitis C virus
- ICR:
-
Institute of Cancer Research
- LD50 :
-
Lethal dose
- LC–MS:
-
Liquid chromatography–mass spectrometry
- KM:
-
Kunming
- LPO:
-
Lipid peroxidation
- LDH:
-
Lactate dehydrogenase
- MS:
-
Mass spectroscopy
- MDA:
-
Malondialdehyde
- ROS:
-
Reactive oxygen species
- SOD:
-
Superoxide dismutase
- TG:
-
Triglyceride
- TBARS:
-
Thiobarbituric acid reactive substances
- TB:
-
Tuberculosis
- WHO:
-
World Health Organization
References
Adewusi EA, Afolayan AJ (2010) A review of natural products with hepatoprotective activity. J Med Plants Res 4(13):1318–1334
Alvari A, Ahmad FJ, Abdin M (2012) Contemporary overview on clinical trials and future prospects of hepato-protective herbal medicines. Rev Recent Clin Trials 7(3):214–223
Aneja S, Vats M, Aggarwal S, Sardana S (2013) Phytochemistry and hepatoprotective activity of aqueous extract of Amaranthus tricolor Linn. roots. J Ayurv Integr Med 4(4):211
Annapandian VM, Rajagopal SS (2017) Phytochemical evaluation and in vitro antioxidant activity of various solvent extracts of Leucas aspera (Willd.) Link leaves. Free Radic Antioxid 7(2):166–171
Aoki C, Hartati SRI, Santi MR, Firdaus R, Hanafi M, Kardono LB, Hotta H (2014) Isolation and identification of substances with anti-hepatitis C virus activities from Kalanchoe pinnata. Int J Pharmacy Pharmaceut Sci 6(2):211–215
Arulmozhi S, Mazumder PM, Lohidasan S, Thakurdesai P (2010) Antidiabetic and antihyperlipidemic activity of leaves of Alstonia scholaris Linn. R. Br. Eur J Integr Med 2(1):23–32
Arulmozhi S, Mazumder PM, Sathiyanarayanan L, Ashok P (2011) Anti-arthritic and antioxidant activity of leaves of Alstonia scholaris Linn. R. Br. Eur J Integr Med 3(2):e83–e90
Arun K, Balasubramanian U (2011) Comparative study on hepatoprotective activity of Phyllanthus amarus and Eclipta prostrata against alcohol induced in albino rats. Int J Environ Sci 2(1):361–379
Baliga MSJC (2012) Review of the phytochemical, pharmacological and toxicological properties of Alstonia scholaris Linn. R. Br. (Saptaparna). Chin J Integr Med. https://doi.org/10.1007/s11655-011-0947-0
Banu S, Bhaskar B, Balasekar P (2012) Hepatoprotective and antioxidant activity of Leucas aspera against d-galactosamine induced liver damage in rats. Pharmaceut Biol 50(12):1592–1595
Bedi O, Bijjem KRV, Kumar P, Gauttam V (2016) Herbal induced hepatoprotection and hepatotoxicity: a critical review. Indian J Physiol Pharmacol 60(1):6–21
Bello I, Bakkouri AS, Tabana YM, Al-Hindi B, Al-Mansoub MA, Mahmud R, Asmawi M (2016) Acute and sub-acute toxicity evaluation of the methanolic extract of Alstonia scholaris stem bark. Med Sci 4(1):4
Bhanu SH, Meena B, Pallavi CJIJP, Sci P (2011) Suppression of paracetamol toxicity by antitoxidant principles of Hybanthus enneaspermus (L.) F. Muell Mice Blood Liver 4:90–94
Bhoopat L, Srichairatanakool S, Kanjanapothi D, Taesotikul T, Thananchai H, Bhoopat T (2011) Hepatoprotective effects of lychee (Litchi chinensis Sonn.): a combination of antioxidant and anti-apoptotic activities. J Ethnopharmacol 136(1):55–66
Biswas SK, Chowdhury A, Das J, Hosen SZ, Uddin R, Rahaman MS (2011) Literature review on pharmacological potentials of Kalanchoe pinnata (Crassulaceae). Afr J Pharm Pharmacol 5(10):1258–1262
Chen LG, Chang CW, Tsay JG, Weng BBC (2017) Hepatoprotective effects of litchi (Litchi chinensis) procyanidin A2 on carbon tetrachloride-induced liver injury in ICR mice. Exp Therap Med 13(6):2839–2847
Chen LG, Chang CW, Tsay JG, Weng BBC (2017a) Hepatoprotective effects of litchi (Litchi chinensis) procyanidin A2 on carbon tetrachloride-induced liver injury in ICR mice. Exp Ther Med 13(6):2839–2847
Chinonyelum AN, Uwadiegwu AP, Nwachukwu OC, Emmanuel O (2015) Evaluation of hepatoprotective activity of Colocasia esculenta (L. Schott) leaves on thioacetamide-induced hepatotoxicity in rats. Pak J Pharmaceut Sci 28(6 Suppl):2237–2241
Chinonyelum AN, Uwadiegwu AP, Nwachukwu OC, Emmanuel O (2015) Evaluation of hepatoprotective activity of Colocasia esculenta (L. Schott) leaves on thioacetamide-induced hepatotoxicity in rats. Pak J Pharmaceut Sci 28(6 Suppl):2237–2241
Domitrović R, Jakovac H, Vasiljev Marchesi V, Vladimir-Knežević S, Cvijanović O, Tadić Ž, Rahelić D (2012) Differential hepatoprotective mechanisms of rutin and quercetin in CCl4-intoxicated BALB/cN mice. Acta Pharmacol Sin 33(10):1260–1270
Doughari J, Manzara S (2008) In vitro antibacterial activity of crude leaf extracts of Mangifera indica Linn. Afr J Microbiol Res 2(4):67–72
Du Q, Chan LY, Gilding EK, Henriques ST, Condon ND, Ravipati AS, Craik DJ (2020) Discovery and mechanistic studies of cytotoxic cyclotides from the medicinal herb Hybanthus enneaspermus. J Biol Chem 295(32):10911–10925
Ediriweera MK, Tennekoon KH, Samarakoon SR (2017) A review on ethnopharmacological applications, pharmacological activities, and bioactive compounds of Mangifera indica (mango). Evid-Based Complement Altern Med. https://doi.org/10.1155/2017/6949835
Enjamoori VK, Nampalli A, Vasudha B, Gangarapu K, Boggula N (2019) A review on Leucas aspera for phytopharmacological studies. INNOSC Theranost Pharmacol Sci 2(1):3–7
Fahmy SR, Amien AI, Abd-Elgleel FM, Elaskalany SM (2016) Antihepatotoxic efficacy of Mangifera indica L. polysaccharides against cyclophosphamide in rats. Chemico-Biol Interact 244:113–120
Feng L, Zhai YY, Xu J, Yao WF, Cao YD, Cheng FF, Zhang L (2019) A review on traditional uses, phytochemistry and pharmacology of Eclipta prostrata (L.) L. J Ethnopharmacol 245:112109
Garrido G, Rodeiro I, Hernández I, García G, Pérez G, Merino N, Delgado R (2009) In vivo acute toxicological studies of an antioxidant extract from Mangifera indica L. (Vimang). Drug Chem Toxicol 32(1):53–58
Girish C, Pradhan S (2017) Herbal drugs on the liver. Liver pathophysiology. Elsevier, Amsterdam, pp 605–620
Guha B, Arman M, Nazmul Islam M, Mohammad Tareq S, Masudur Rahman M, Alam Sakib S, Alqahtani AM (2020) Unveiling pharmacological studies provide new insights on Mangifera longipes and Quercus gomeziana. Saudi J Biol Sci. https://doi.org/10.1016/j.sjbs.2020.09.037
Guo J, Friedman SL (2010) Toll-like receptor 4 signaling in liver injury and hepatic fibrogenesis. Fibrogenesis Tissue Repair 3(1):1–19
Haque MA, Jantan I, Bukhari SNA (2017) Tinospora species: an overview of their modulating effects on the immune system. J Ethnopharmacol 207:67–85
Hiraganahalli BD, Chinampudur VC, Dethe S, Mundkinajeddu D, Pandre MK, Balachandran J, Agarwal A (2012) Hepatoprotective and antioxidant activity of standardized herbal extracts. Pharmacogn Mag 8(30):116
Ibrahim SR, Mohamed GA (2015a) Litchi chinensis: medicinal uses, phytochemistry, and pharmacology. J Ethnopharmacol 174:492–513
Ibrahim SR, Mohamed GA (2015) Litchi chinensis: medicinal uses, phytochemistry, and pharmacology. J Ethnopharmacol 174:492–513
Jaiswal S, Chawla R, Sawhney S (2014) Kalanchoe pinnata—a promising source of natural antioxidants. Eur J Med Plants. 4:1210–1222
Karuppanan M, Krishnan M, Padarthi P, Namasivayam E (2014) Hepatoprotective and antioxidant effect of Mangifera indica leaf extracts against mercuric chloride-induced liver toxicity in mice. Euroas J Hepato-gastroenterol 4(1):18
Khan AV, Khan AA (2008) Ethnomedicinal uses of Eclipta prostrta Linn. Indian J Tradit Knowl
Khan MF, Kader FB, Arman M, Ahmed S, Lyzu C, Sakib SA, Venneri T (2020) Pharmacological insights and prediction of lead bioactive isolates of Dita bark through experimental and computer-aided mechanism. Biomed Pharmacother 131:110774
Kumar CH, Ramesh A, Kumar JS, Ishaq BM (2011) A review on hepatoprotective activity of medicinal plants. Int J Pharmaceut Sci Res 2(3):501
Kumar A, Khan MA, Saxena A, Singh RB, Zaman K, Husain A (2012) Hepatoprotective activity of methanolic extract of stem bark of Alstonia scholaris (L.) R. Br. AJPTR 2(2):545–555
Kumar A, Khan MA, Saxena A, Singh RB, Zaman K, Husain AJA (2012) Hepatoprotective activity of methanolic extract of stem bark of Alstonia scholaris (L.) R. Br. AJPTR 2(2):545–555
Latha MS, Latha B, Oommen SK, Rajalekshmi R (2012) Hepatoprotective and antioxidant effects methanolic extract of Leucas aspera against carbon tetra chloride induced oxidative damage in rats. Int J Adv Pharm Res 4:1331–1337
Lavanchy D (2009) The global burden of hepatitis C. Liver Int 29:74–81
Lee WJEL (1999) Taro (colocasia Esculenta) 1999(1):4
Lee MK, Ha NR, Yang H, Sung SH, Kim GH, Kim YC (2008a) Antiproliferative activity of triterpenoids from Eclipta prostrata on hepatic stellate cells. Phytomedicine 15(9):775–780
Lee MK, Ha NR, Yang H, Sung SH, Kim GH, Kim YC (2008) Antiproliferative activity of triterpenoids from Eclipta prostrata on hepatic stellate cells. Phytomedicine 15(9):775–780
Lin SC, Lin CC, Lin YH, Supriyatna S, Pan SL (1996) The protective effect of Alstonia scholaris R Br on hepatotoxin-induced acute liver damage. Am J Chin Med 24(02):153–164
Lin SC, Yao CJ, Lin CC, Lin YH (1996) Hepatoprotective activity of Taiwan folk medicine: Eclipta prostrata Linn. against various hepatotoxins induced acute hepatotoxicity. Phytother Res 10(6):483–490
Lin SC, Yao CJ, Lin CC, Lin YH (1996) Hepatoprotective activity of Taiwan folk medicine: Eclipta prostrata Linn. against various hepatotoxins induced acute hepatotoxicity. Phytother Res 10(6):483–490
Liu L-S, Liu M-H, He J-Y (2014) Hypericum japonicum Thunb. ex Murray: phytochemistry, pharmacology, quality control and pharmacokinetics of an important herbal medicine. Molecules 19(8):10733–10754
Liu LS, Liu MH, He JY (2014) Hypericum japonicum Thunb. ex Murray: phytochemistry, pharmacology, quality control and pharmacokinetics of an important herbal medicine. Molecules 19(8):10733–10754
Liu M, Zhang G, Song M, Wang J, Shen C, Chen Z, Liu C (2020) Activation of farnesoid X receptor by schaftoside ameliorates acetaminophen-induced hepatotoxicity by modulating oxidative stress and inflammation. Antioxid Redox Signal 33(2):87–116
Liu M, Zhang G, Song M, Wang J, Shen C, Chen Z, Lin C (2020a). Activation of FXR by schaftoside ameliorates APAP-induced hepatotoxicity by modulating oxidative stress and inflammation. Antioxid Redox Signal
Lok AS, Heathcote EJ, Hoofnagle JH (2001) Management of hepatitis B: 2000—summary of a workshop. Gastroenterology 120(7):1828–1853
Mamun F, Rahman MM, Zamila M, Subhan N, Hossain H, Raquibul Hasan SM, Haque MA (2020) Polyphenolic compounds of litchi leaf augment kidney and heart functions in 2K1C rats. J Funct Foods 64:103662. https://doi.org/10.1016/j.jff.2019.103662
Mazid M, Khan TA, Mohammad F (2012) Medicinal plants of rural India: a review of use by Indian folks. Indo Glob J Pharmaceut Sci 2(3):286–304
Meena AK, Nitika G, Jaspreet N, Meena RP, Rao MM (2011) Review on ethanobotany, phytochemical and pharmacological profile of Alstonia scholaris. Int Res J Pharm 2(1):49–54
Nzebang DCN, Njila MIN, Bend EF, Oundoum PCO, Koloko BL, Zangueu CB, Lembè DM (2018) Evaluation of the toxicity of Colocasia esculenta (Aracaceae): preliminary study of leaves infected by Phytophthora colocasiae on wistar albinos rats. Biomed Pharmacother 99:1009–1013
Olaokun OO, Mkolo NM, Mogale MA, King PH (2017) Phytochemical screening, antioxidant, anti-inflammatory and glucose utilization activities of three South African plants used traditionally to treat diseases. Biol Med (Aligarh) 9(412):2
Omotayo MA, Ogundare OC, Oluwafunmilayo A, Longe SA (2015) Hepatoprotective effect of Mangifera-indica stem bark extracts on paracetamol-induced oxidative stress in albino rats. Eur Sci J 11(24)
Ortiz de Montellano PR (2013) Cytochrome P450-activated prodrugs. Future Med Chem 5(2):213–228
Park J-G, Cheon H-J, Kim Y-S, Kang S-S, Choi J-S, Lee S-M (2007) Hepatoprotective activities of daidzin, daidzein, genistein and puerarin in primary cultured rat hepatocytes. Yakhak Hoeji 51(2):115–125
Patel D, Kumar R, Sairam K, Hemalatha S (2013) Hybanthus enneaspermus (L.) F. Muell: a concise report on its phytopharmacological aspects. Chin J Nat Med 11(3):199–206
Patil BR, Ageely HM (2011) Antihepatotoxic activity of Colocasia esculenta leaf juice. Int J Adv Biotechnol Res 2(2):296–304
Pattewar SV (2012) Kalanchoe pinnata: phytochemical and pharmacological profile. Int J Pharm Sci Res 3(4):993
Phatak RS, Hendre AS (2014) Total antioxidant capacity (TAC) of fresh leaves of Kalanchoe pinnata. J Pharmacogn Phytochem 2(5):32–35
Pourahmad J, Eskandari MR, Shakibaei R, Kamalinejad M (2010) A search for hepatoprotective activity of fruit extract of Mangifera indica L. against oxidative stress cytotoxicity. Plant Foods Hum Nutr 65(1):83–89
Prajapati MS, Patel JB, Modi K, Shah MB (2010) Leucas aspera: a review. Pharmacogn Rev 4(7):85
Quazi Majaz A, Tatiya A, Khurshid M, Nazim S, Siraj S (2011) The miracle plant (Kalanchoe pinnata): a phytochemical and pharmacological review. Int J Res Ayurveda Pharm 2(5):1478–1482
Rahman A, Hossain MM, Islam A (2014a) Taxonomy and medicinal uses of angiosperm weeds in the wheat field of Rajshahi, Bangladesh. Front Biol Life Sci 2(1):8–11
Rahman A, Hossain MM, Islam AJF, Sciences L (2014b) Taxonomy and medicinal uses of angiosperm weeds in the wheat field of Rajshahi. Bangladesh 2(1):8–11
Rajakumar G, Gomathi T, Abdul Rahuman A, Thiruvengadam M, Mydhili G, Kim S-H, Chung I-M (2016) Biosynthesis and biomedical applications of gold nanoparticles using Eclipta prostrata leaf extract. Appl Sci 6(8):222
Rajsekhar P, Bharani RA, Angel KJ, Ramachandran M, Rajsekhar SPV (2016) Hybanthus enneaspermus (L.) F. Muell: a phytopharmacological review on herbal medicine. J Chem Pharm Res 8(1):351–355
Rajsekhar PB, Bharani RA, Angel KJ, Ramachandran M, Rajsekhar SPV (2016) Hybanthus enneaspermus (L.) F. Muell: a phytopharmacological review on herbal medicine. J Chem Pharmaceut Res 8(1):351–355
Rashmi D, Raghu N, Gopenath T, Palanisamy P, Bakthavatchalam P, Karthikeyan M, Basalingappa K (2018) Taro (Colocasia esculenta): an overview. J Med Plants Stud 6(4):156–161
Rathore P, Rao SP, Roy A, Satapathy T, Singh V, Jain P (2014a) Hepatoprotective activity of isolated herbal compounds. Res J Pharmacy Technol 7(2):229–234
Rathore P, Rao SP, Roy A, Satapathy T, Singh V, Jain P (2014) Hepatoprotective activity of isolated herbal compounds. Res J Pharmacy Technol 7(2):229–234
Reddeman RA, Glávits R, Endres JR, Clewell AE, Hirka G, Vértesi A, Szakonyiné IP (2019) A toxicological evaluation of mango leaf extract (Mangifera indica) containing 60% mangiferin. J Toxicol. https://doi.org/10.1155/2019/4763015
Rehman JU, Aktar N, Khan MY, Ahmad K, Ahmad M, Sultana S, Asif HM (2015) Phytochemical screening and hepatoprotective effect of Alhagi maurorum boiss (Leguminosae) against paracetamol-induced hepatotoxicity in rabbits. Trop J Pharmaceut Res 14(6):1029–1034
Sagar R, Bhaiji A, Toppo FA, Rath B, Sahoo HB (2014) A comprehensive review on herbal drugs for hepatoprotection of 21st Century. Int J Nutr Pharmacol Neurol Dis 4(4):191
Saikia A, Das M, Saikia Q (2018a) Hepatoprotective potential of the methanolic extract of Colocasia esculenta on iron overload induced mice. Med Plants-Int J Phytomed Relat Ind 10(3):243–251
Saikia A, Das M, Saikia Q (2018) Hepatoprotective potential of the methanolic extract of Colocasia esculenta on iron overload induced mice. Med Plants-Int J Phytomed Relat Ind 10(3):243–251
Samaga PV, Rai VR (2016a) Diversity and bioactive potential of endophytic fungi from Nothapodytes foetida, Hypericum mysorense and Hypericum japonicum collected from Western Ghats of India. Ann Microbiol 66(1):229–244
Samaga PV, Rai VR (2016) Diversity and bioactive potential of endophytic fungi from Nothapodytes foetida, Hypericum mysorense and Hypericum japonicum collected from Western Ghats of India. Ann Microbiol 66(1):229–244
Sarhadynejad Z, Sharififar F, Pardakhty A, Nematollahi M-H, Sattaie-Mokhtari S, Mandegary A (2016) Pharmacological safety evaluation of a traditional herbal medicine “Zereshk-e-Saghir” and assessment of its hepatoprotective effects on carbon tetrachloride induced hepatic damage in rats. J Ethnopharmacol 190:387–395
Saxena M, Saxena J, Nema R, Singh D, Gupta A (2013) Phytochemistry of medicinal plants. J Pharmacogn Phytochem 1(6):168–182
Shah K, Patel M, Patel R, Parmar P (2010) Mangifera indica (mango). Pharmacogn Rev 4(7):42
Shang J-H, Cai X-H, Zhao Y-L, Feng T, Luo X-D (2010) Pharmacological evaluation of Alstonia scholaris: anti-tussive, anti-asthmatic and expectorant activities. J Ethnopharmacol 129(3):293–298
Shankar KR, Rao AL, Kalyani L (2012) Hepatoprotective activity of Alstonia scholaris fruits against carbon tetrachloride-induced hepatotoxicity in rats. Asian J. Pharmaceut Res Health Care 4(1):28–32
Singh J, Bagla A, Pahal V (2010) Hepatoprotective activity of herbal extracts in carbon tetrachloride intoxicated albino rats by measuring anti-oxidant enzymes. Int J PharmTech Res 2(3):2112–2115
Singh J, Bagla A, Pahal V (2010a) Hepatoprotective activity of herbal extracts in carbon tetrachloride intoxicated albino rats by measuring anti-oxidant enzymes. Int J PharmTech Res 2(3):2112–2115
Soni R, Agrawal S (2017) Litchi chinensis: taxonomy, botany and its cultivars. Lychee disease management. Springer, Berlin, pp 191–215
Stickel F, Schuppan D (2007) Herbal medicine in the treatment of liver diseases. Dig Liver Dis 39(4):293–304
Sultana S, Perwaiz S, Iqbal M, Athar M (1995) Crude extracts of hepatoprotective plants, Solanum nigrum and Cichorium intybus inhibit free radical-mediated DNA damage. J Ethnopharmacol 45(3):189–192
Su D, Zhang R, Zhang C, Huang F, Xiao J, Deng Y, Zhang M (2016) Phenolic-rich lychee (Litchi chinensis Sonn.) pulp extracts offer hepatoprotection against restraint stress-induced liver injury in mice by modulating mitochondrial dysfunction. Food Funct 7(1):508–515
Tatiya AU, Surana SJ, Sutar MP, Gamit NH (2012) Hepatoprotective effect of poly herbal formulation against various hepatotoxic agents in rats. Pharmacogn Res 4(1):50
Thenmozhi M, Dhanalakshmi M, Devi KM, Sushila K, Thenmozhi S (2013) Evaluation of hepatoprotective activity of Leucas aspera hydroalcoholic leaf extract during exposure to lead acetate in male albino Wistar rats. Asian J Pharm Clin Res 6(1):78–81
Thyagarajan S, Jayaram S, Gopalakrishnan V, Hari R, Jeyakumar P, Sripathi M (2002) Herbal medicines for liver diseases in India. J Gastroenterol Hepatol 17:S370–S376
Trauner M, Boyer JL (2003) Bile salt transporters: molecular characterization, function, and regulation. Physiol Rev 83(2):633–671
Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J (2007) Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol 39(1):44–84
Vargas-Mendoza N, Madrigal-Santillán E, Morales-González Á, Esquivel-Soto J, Esquivel-Chirino C (2014) Hepatoprotective effect of silymarin. World J Hepatol 6(3):144
Vrba J, Modriansky M (2002) Oxidative burst of Kupffer cells: target for liver injury treatment. Biomed Pap-Palacky Univ Olomouc 146(2):15–20
Vuda M, D’Souza R, Upadhya S, Kumar V, Rao N, Kumar V, Mungli P (2012a) Hepatoprotective and antioxidant activity of aqueous extract of Hybanthus enneaspermus against CCl4-induced liver injury in rats. Exp Toxicol Pathol 64(7–8):855–859
Vuda M, D’Souza R, Upadhya S, Kumar V, Rao N, Kumar V, Mungli P (2012) Hepatoprotective and antioxidant activity of aqueous extract of Hybanthus enneaspermus against CCl4-induced liver injury in rats. Exp Toxicol Pathol 64(7–8):855–859
Wang J-K, Higa S (1983) Taro, a review of Colocasia esculenta and its potentials. University of Hawaii Press, Honolulu
Wang N, Li P, Wang Y, Peng W, Wu Z, Tan S, Su W (2008) Hepatoprotective effect of Hypericum japonicum extract and its fractions. J Ethnopharmacol 116(1):1–6
Wang N, Wang Y, Li P, Peng W, Xie T, Feng Y, Su W (2009) The bioavailability of hepatoprotective flavoniods in Hypericum japonicum extract. J Bioanal Biomed 1:033–038
Wang C-M, Chen H-T, Wu Z-Y, Jhan Y-L, Shyu C-L, Chou C-H (2016) Antibacterial and synergistic activity of pentacyclic triterpenoids isolated from Alstonia scholaris. Molecules 21(2):139
Wang C-M, Tsai S-J, Jhan Y-L, Yeh K-L, Chou C-H (2017) Anti-proliferative activity of triterpenoids and sterols isolated from Alstonia scholaris against non-small-cell lung carcinoma cells. Molecules 22(12):2119
Wauthoz N, Balde A, Balde ES, Van Damme M, Duez P (2007) Ethnopharmacology of Mangifera indica L. bark and pharmacological studies of its main C-glucosylxanthone, mangiferin. Int J Biomed Pharmaceut Sci 1(2):112–119
Waxman A (2004) WHO global strategy on diet, physical activity and health. Food Nutr Bull 25(3):292–302
Wu Y-HS, Chiu C-H, Yang D-J, Lin Y-L, Tseng J-K, Chen Y-C (2013) Inhibitory effects of litchi (Litchi chinensis Sonn.) flower-water extracts on lipase activity and diet-induced obesity. J Funct Foods 5(2):923–929
Yadav NP, Dixit VK (2003) Hepatoprotective activity of leaves of Kalanchoe pinnata Pers. J Ethnopharmacol 86(2–3):197–202
Zhang W-D, Fu P, Liu R-H, Li T-Z, Li H-L, Zhang W, Chen H-S (2007) A new bisxanthone from Hypericum japonicum. Fitoterapia 78(1):74–75
Zhang YQ, Huang MQ, Li H, Xu W, Chu KD, Zheng HY, Sha M, Chen LD (2012) Hepatoprotective and antioxidant activity of the total flavonoids extraction from Hypericum japonicum by response surface methodology. Latin Am J Pharm 31:1270–8
Zhang YJ, Gan RY, Li S, Zhou Y, Li AN, Xu DP, Li HB (2015) Antioxidant phytochemicals for the prevention and treatment of chronic diseases. Molecules 20(12):21138–21156
Zhang R, Ji Y, Zhang X, Kennelly EJ, Long C (2020) Ethnopharmacology of Hypericum species in China: a comprehensive review on ethnobotany, phytochemistry and pharmacology. J Ethnopharmacol 254:112686
Acknowledgements
The authors would like to thank the Department of Pharmacy, International Islamic University Chittagong for necessary supports.
Funding
Open access funding provided by Università degli Studi di Napoli Federico II within the CRUI-CARE Agreement. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Arman, M., Chowdhury, K.A.A., Bari, M.S. et al. Hepatoprotective potential of selected medicinally important herbs: evidence from ethnomedicinal, toxicological and pharmacological evaluations. Phytochem Rev 21, 1863–1886 (2022). https://doi.org/10.1007/s11101-022-09812-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11101-022-09812-5