Abstract
Purpose
The purpose of this study was to determine whether treatment outcomes vary according to the design of the mandibular repositioning appliance (MRA). Two titratable MRA's were compared. The designs differ in advancement hardware and configuration of acrylic both in bulk and interocclusal contact.
Materials and methods
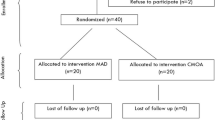
The primary treatment outcome was the Respiratory Disturbance Index (RDI). Other outcomes that were compared included Sleep Apnea Quality of Life Index (SAQLI), Epworth Sleepiness Scale, oxygen saturation, and subjective feedback regarding experiences with the appliances. Twenty-four subjects were recruited from consecutive referrals for MRA therapy following diagnosis of obstructive sleep apnea (OSA) by polysomnography. Subjects were randomly assigned to a treatment arm of the crossover study. Each subject underwent an initial sleep study with a type III home monitor to establish a baseline RDI. Subjects were then treated with one of the two MRAs determined by random assignment. The MRA self-titration phase was monitored until a treatment position was determined, and the home sleep study was repeated. After a 2-week period without any OSA treatment, subjects received the second MRA and the self-titration treatment protocol was repeated. At completion of treatment with each appliance, subjects answered questionnaires and underwent a sleep study with the type III monitor. The outcome data for each appliance were compared using analysis of variance.
Results
Eighteen subjects completed the treatment protocol. There were no significant statistical differences in treatment outcomes between the two appliances. There was a statistically significant (p ≤ 0.05) preference for a MRA design with minimal coverage of teeth and palate. The subjects' appliance selection was consistent with a corresponding reduction in SAQLI score for the selected appliance.
Conclusion
Although no statistically significant difference was observed between the two appliances in the outcomes measured, there was a trend toward greater improvement with the appliance with less acrylic resin bulk and less interocclusal contact. MRA selection should favor titratable, unobtrusive designs with appropriate construction to promote acceptance and adherence to MRA therapy.
Similar content being viewed by others
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. New Engl J Med 328(17):1230–1235
Kushida CA, Morgenthaler TI, Littner MR, Alessi CA, Bailey D, Coleman J Jr, Friedman L, Hirshkowitz M, Kapen S, Kramer M, Lee-Chiong T, Owens J, Pancer JP (2006) Practice parameters for the treatment of snoring and obstructive sleep apnea with oral appliances: an update for 2005. Sleep 29:240–243
D’Alessandro R, Magelli C, Gamberini G, Bacchelli S, Cristina E, Magnani B, Lugaresi E (1990) Snoring every night as a risk factor for myocardial infarction: a case–control study. BMJ 300:1557–1558
Partinen M, Guilleminault C (1990) Daytime sleepiness and vascular morbidity at seven-year follow-up in obstructive sleep apnea patients. Chest 97:27–32
Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Javier Nieto F, O’Connor GT, Boland LL, Schwartz JE, Samet JM (2001) Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med 163:19–25
Shamsuzzaman AS, Gersh BJ, Somers VK (2003) Obstructive sleep apnea: implications for cardiac and vascular disease. JAMA 290:1906–1914
Young T, Peppard P (2000) Sleep-disordered breathing and cardiovascular disease: epidemiologic evidence for a relationship. Sleep 23:S122–S126
Ferguson KA, Ono T, Lowe AA, al-Majed S, Love LL, Fleetham JA (1997) A short-term controlled trial of an adjustable oral appliance for the treatment of mild to moderate obstructive sleep apnoea. Thorax 52:362–368
Hiyama S, Tsuiki S, Ono T, Kuroda T, Ohyama K (2003) Effects of mandibular advancement on supine airway size in normal subjects during sleep. Sleep 26:440–445
Skinner MA, Robertson CJ, Kingshott RN, Jones DR, Taylor DR (2002) The efficacy of a mandibular advancement splint in relation to cephalometric variables. Sleep Breath 6:115–124
Fransson AM, Svenson BA, Isacsson G (2002) The effect of posture and a mandibular protruding device on pharyngeal dimensions: a cephalometric study. Sleep Breath 6:55–68
Tegelberg A, Walker-Engstrom ML, Vestling O, Wilhelmsson B (2003) Two different degrees of mandibular advancement with a dental appliance in treatment of patients with mild to moderate obstructive sleep apnea. Acta Odontol Scand 61:356–362
Walker-Engstrom ML, Ringqvist I, Vestling O, Wilhelmsson B, Tegelberg A (2003) A prospective randomized study comparing two different degrees of mandibular advancement with a dental appliance in treatment of severe obstructive sleep apnea. Sleep Breath 7:119–130
Pancer J, Al-Faifi S, Al-Faifi M, Hoffstein V (1999) Evaluation of variable mandibular advancement appliance for treatment of snoring and sleep apnea. Chest 116:1511–1518
Pitsis AJ, Darendeliler MA, Gotsopoulos H, Petocz P, Cistulli PA (2002) Effect of vertical dimension on efficacy of oral appliance therapy in obstructive sleep apnea. Am J RespirCrit Care Med 166:860–864
Hans MG, Nelson S, Luks VG, Lorkovich P, Baek SJ (1997) Comparison of two dental devices for treatment of obstructive sleep apnea syndrome (OSAS). Am J Orthod Dentofacial Orthop 111:562–570
Ferguson KA, Cartwright R, Rogers R, Schmidt-Nowara W (2006) Oral appliances for snoring and obstructive sleep apnea: a review. Sleep 29:244–262
Kryger MH, Roth T, Dement WC (eds) (2005) Principles and practice of sleep medicine, 4th edn. Elsevier/Saunders, Philadelphia
Lim J, Lasserson TJ, Fleetham J, Wright J (2006) Oral appliances for obstructive sleep apnoea. Cochrane Database Syst Rev
Schmidt-Nowara W, Lowe A, Wiegand L, Cartwright R, Perez-Guerra F, Menn S (1995) Oral appliances for the treatment of snoring and obstructive sleep apnea: a review. Sleep 18:501–510
Bloch KE, Iseli A, Zhang JN, Xie X, Kaplan V, Stoeckli PW, Russi EW (2000) A randomized, controlled crossover trial of two oral appliances for sleep apnea treatment. Am J Respir Crit Care Med 162:246–251
Eckhart JE (1998) Comparisons of oral devices for snoring. J Calif Dent Assoc 26:611–623
Lawton HM, Battagel JM, Kotecha B (2005) A comparison of the Twin Block and Herbst mandibular advancement splints in the treatment of patients with obstructive sleep apnoea: a prospective study. Eur J Orthod 27:82–90
Luks V, Lorkovich P, Hans M, Nelson S (1996) Comparing three dental devices for treatment of OSAS. J Dent Res 75(Special Issue):19
Rose E, Staats R, Virchow C, Jonas IE (2002) A comparative study of two mandibular advancement appliances for the treatment of obstructive sleep apnoea. Eur J Orthod 24:191–198
Gauthier L, Laberge L, Beaudry M, Laforte M, Rompré PH, Lavigne GJ (2009) Efficacy of two mandibular advancement appliances in the management of snoring and mild-moderate sleep apnea: a crossover randomized study. Sleep Med 10:329–336
Gauthier L, Laberge L, Beaudry M, Laforte M, Rompré PH, Lavigne GJ (2011) Mandibular advancement appliances remain effective in lowering respiratory disturbance index for 2.5–4.5 years. Sleep Med 12:844–849
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep 14:540–545
Flemons WW, Reimer MA (1998) Development of a disease-specific health-related quality of life questionnaire for sleep apnea. Am J Respir Crit Care Med 158:494–503
Flemons WW, Reimer MA (2002) Measurement properties of the Calgary sleep apnea quality of life index. Am J Respir Crit Care Med 165:159–164
Lacasse Y, Godbout C, Series F (2002) Independent validation of the Sleep Apnoea Quality of Life Index. Thorax 57:483–488
Lowe AA (1999) Titratable oral appliances for the treatment of snoring and obstructive sleep apnea. J Can Dent Assoc 65:571–574
Ferber R, Millman R, Coppola M, Fleetham J, Murray CF, Iber C, McCall V, Nino-Murcia G, Pressman M, Sanders M, Strohl K, Votteri B, Williams A (1994) Portable recording in the assessment of obstructive sleep apnea. ASDA standards of practice. Sleep 17(4):378–392
Flemons WW, Littner MR, Rowley JA, Gay P, Anderson WM, Hudgel DW, McEvoy RD, Loube DI (2003) Home diagnosis of sleep apnea: a systematic review of the literature. An evidence review cosponsored by the American Academy of Sleep Medicine, the American College of Chest Physicians, and the American Thoracic Society. Chest 124:1543–1579
Vasquez J-C, Tsai W, Flemons WW, Masuda A, Brant R, Hajduk E, Whitelaw WA, Remmers JE (2000) Automated analysis of digital oximetry in the diagnosis of obstructive sleep apnoea. Thorax 55:302–307
Issa FG, Morrison D, Hadjuk E, Iyer A, Feroah T, Remmers JE (1993) Digital monitoring of sleep-disordered breathing using snoring sound and arterial oxygen saturation. Am Rev Respir Dis 148:1023–1029
Vazquez JC, Tsai WH, Flemons WW, Masuda A, Brant R, Hajduk E, Whitelaw WA, Remmers JE (2000) Automated analysis of digital oximetry in the diagnosis of obstructive sleep apnoea. Thorax 55:302–307
Epstein LJ, Kristo D, Strollo PJ, Friedman N, Malhotra A, Patil SP, Ramar K, Rogers R, Schwab RJ, Weaver EM, Weinstein MD (2009) Clinical guidelines for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 5:263–276
McLornan PM (2009) Evaluation of obstructive sleep apnea patients' oral appliance titration protocols [thesis]. [San Antonio, TX]: University of Texas Health Science Center at San Antonio. Pp.117-120
Winer BJ (1971) Statistical principles in experimental design. McGraw-Hill, New York, p 797
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bishop, B., Verrett, R. & Girvan, T. A randomized crossover study comparing two mandibular repositioning appliances for treatment of obstructive sleep apnea. Sleep Breath 18, 125–131 (2014). https://doi.org/10.1007/s11325-013-0859-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-013-0859-7