Abstract
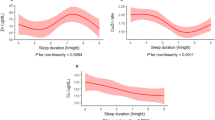
This study aimed to evaluate the association between blood ethylene oxide (HbEtO) levels and short sleep duration (SSD). Data of 3438 participants aged 20 years or older in this study were collected from the National Health and Nutrition Examination Survey (NHANES). The ethylene oxide (EtO) biomarker (HbEtO) was quantified in blood using a high-performance liquid chromatography-tandem mass spectrometry (HPLC-MS/MS) method. SSD was defined as sleep time equal to or less than 6 h. The analyses utilized weighted logistic regression models and restricted cubic spline. There was a significant non-linear relationship between HbEtO levels and the risk of SSD (P for-nonlinearity = 0.035). After the full adjustment for confounders, compared with the lowest quantile, the odds ratios (ORs) with 95% confidence intervals (CIs) of SSD across the quantiles of ethylene oxide levels were 1.54(1.09–2.18), 1.15(0.87–1.53), and 1.80(1.11–2.92), respectively (P for trend < 0.05). In subgroup analysis, people who were female, who were non-Hispanic Black, who never engaged in physical activity, who consumed alcohol ≤ 14 g/day, who were normal weight or obese had a significantly higher risk of SSD when they had highest quartiles of HbEtO levels than those had lowest (p < 0.05). Our study indicated that HbEtO levels, an indicator for EtO exposure, were associated with SSD in general adult populations.


Similar content being viewed by others
Availability of data and materials
The data utilized to support the findings are available from the corresponding authors upon request.
References
Ai S, Zhang J, Zhao G, Wang N, Li G, So HC, Liu Y, Chau SW, Chen J, Tan X, Jia F, Tang X, Shi J, Lu L, Wing YK (2021) Causal associations of short and long sleep durations with 12 cardiovascular diseases: linear and nonlinear Mendelian randomization analyses in UK Biobank. Eur Heart J 42:3349–3357
Atrooz F, Salim S (2020) Sleep deprivation, oxidative stress and inflammation. Adv Protein Chem Struct Biol 119:309–336
Bacaro V, Ballesio A, Cerolini S, Vacca M, Poggiogalle E, Donini LM, Lucidi F, Lombardo C (2020) Sleep duration and obesity in adulthood: An updated systematic review and meta-analysis. Obes Res Clin Pract 14:301–309
Bixler E (2009) Sleep and society: an epidemiological perspective. Sleep Med 10(Suppl 1):S3–S6
Boyle EB, Viet SM, Wright DJ, Merrill LS, Alwis KU, Blount BC, Mortensen ME, Moye J Jr, Dellarco M (2016) Assessment of exposure to VOCs among pregnant women in the National Children's Study. Int J Environ Res Public Health 13:376
Cappuccio FP, D'Elia L, Strazzullo P, Miller MA (2010) Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 33:585–592
Cheang I, Zhu X, Zhu Q, Li M, Liao S, Zuo Z, Yao W, Zhou Y, Zhang H, Li X (2022) Inverse association between blood ethylene oxide levels and obesity in the general population: NHANES 2013-2016. Front Endocrinol (Lausanne) 13:926971
Cunningham TJ, Ford ES, Chapman DP, Liu Y, Croft JB (2015) Independent and joint associations of race/ethnicity and educational attainment with sleep-related symptoms in a population-based US sample. Prev Med 77:99–105
de Sousa DE, de Carli MN, Fernandes RC, Trindade DB, Laviano A, Pichard C, Pimentel GD (2020) Are depression and anxiety disorders associated with adductor pollicis muscle thickness, sleep duration, and protein intake in cancer patients? Exp Gerontol 130:110803
Desquilbet L, Mariotti F (2010) Dose-response analyses using restricted cubic spline functions in public health research. Stat Med 29:1037–1057
Estrin WJ, Bowler RM, Lash A, Becker CE (1990) Neurotoxicological evaluation of hospital sterilizer workers exposed to ethylene oxide. J Toxicol Clin Toxicol 28:1–20
Fatima Y, Doi SA, Mamun AA (2016) Sleep quality and obesity in young subjects: a meta-analysis. Obes Rev 17:1154-1166
Filser JG (1992) The closed chamber technique--uptake, endogenous production, excretion, steady-state kinetics and rates of metabolism of gases and vapors. Arch Toxicol 66:1–10
Ford ES, Cunningham TJ, Croft JB (2015) Trends in self-reported sleep duration among US adults from 1985 to 2012. Sleep 38:829–832
Gesteiro E, Aparicio-Ugarriza R, Garcia-Centeno MDC, Escobar-Toledo D, Manas A, Perez-Gomez J, Gusi N, Gomez-Cabello A, Ara I, Casajus JA, Vicente-Rodriguez G, Gonzalez-Gross M (2022) Self-reported sleeping time effects on physical performance and body composition among spanish older adults: EXERNET-Elder 3.0 study. Gerontol Geriatr Med 8:23337214221125359
Ghosh M, Godderis L (2016) Genotoxicity of ethylene oxide: A review of micronucleus assay results in human population. Mutat Res Rev Mutat Res 770:84–91
Grandner MA, Patel NP, Gehrman PR, Xie D, Sha D, Weaver T, Gooneratne N (2010) Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med 11:470–478
Grandner MA, Petrov ME, Rattanaumpawan P, Jackson N, Platt A, Patel NP (2013) Sleep symptoms, race/ethnicity, and socioeconomic position. J Clin Sleep Med 9(897-905):905A–905D
Guo J, Wan Z, Cui G, Pan A, Liu G (2021) Association of exposure to ethylene oxide with risk of diabetes mellitus: results from NHANES 2013-2016. Environ Sci Pollut Res Int 28:68551–68559
Heinze G, Schemper M (2001) A solution to the problem of monotone likelihood in Cox regression. Biometrics 57:114–119
Hu N, Ma Y, He J, Zhu L, Cao S (2020) Alcohol consumption and incidence of sleep disorder: A systematic review and meta-analysis of cohort studies. Drug Alcohol Depend 217:108259
Irwin MR, Olmstead R, Carroll JE (2016) Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry 80:40–52
Irwin MR (2019) Sleep and inflammation: partners in sickness and in health. Nat Rev Immunol 19:702–715
Itani O, Jike M, Watanabe N, Kaneita Y (2017) Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med 32:246–256
Jain RB (2020) Associations between observed concentrations of ethylene oxide in whole blood and smoking, exposure to environmental tobacco smoke, and cancers including breast cancer: data for US children, adolescents, and adults. Environ Sci Pollut Res Int 27:20912–20919
Jinot J, Fritz JM, Vulimiri SV, Keshava N (2017) Carcinogenicity of ethylene oxide: key findings and scientific issues. Toxicol Mech Methods 1
Johnson KA, Gordon CJ, Chapman JL, Hoyos CM, Marshall NS, Miller CB, Grunstein RR (2021) The association of insomnia disorder characterised by objective short sleep duration with hypertension, diabetes and body mass index: a systematic review and meta-analysis. Sleep Med Rev 59:101456
Kirman CR, Li AA, Sheehan PJ, Bus JS, Lewis RC, Hays SM (2021) Ethylene oxide review: characterization of total exposure via endogenous and exogenous pathways and their implications to risk assessment and risk management. J Toxicol Environ Health B Crit Rev 24:1–29
Lee SWH, Ng KY, Chin WK (2017) The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: a systematic review and meta-analysis. Sleep Med Rev 31:91–101
Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB (2016) Prevalence of healthy sleep duration among adults--United States, 2014. MMWR Morb Mortal Wkly Rep 65:137–141
Lizonczyk I, Josko-Ochojska J (2021) Relationship between overweight, obesity and sleep disorders in adolescents from selected cities of Upper Silesia, Poland. Ann Agric Environ Med 28:193–197
Lu H, Yang Q, Tian F, Lyu Y, He H, Xin X, Zheng X (2021) A Meta-Analysis of a Cohort Study on the Association between Sleep Duration and Type 2 Diabetes Mellitus. J Diabetes Res 2021:8861038
Lumley T (2014) survey: Analysis of Complex Survey Samples. J Stat Softw 09
Lynch DW, Lewis TR, Moorman WJ, Burg JR, Groth DH, Khan A, Ackerman LJ, Cockrell BY (1984) Carcinogenic and toxicologic effects of inhaled ethylene oxide and propylene oxide in F344 rats. Toxicol Appl Pharmacol 76:69–84
Marsh GM, Keeton KA, Riordan AS, Best EA, Benson SM (2019) Ethylene oxide and risk of lympho-hematopoietic cancer and breast cancer: a systematic literature review and meta-analysis. Int Arch Occup Environ Health 92:919–939
Merianos AL, Mahabee-Gittens EM, Choi K (2021) Tobacco smoke exposure and inadequate sleep among U.S. school-aged children. Sleep Med 86:99–105
Minghelli B (2022) Sleep disorders in higher education students: Modifiable and non-modifiable risk factors. North Clin Istanb 9:215–222
Ohnishi A, Murai Y (1993) Polyneuropathy due to ethylene oxide, propylene oxide, and butylene oxide. Environ Res 60:242–247
Olaguer EP, Robinson A, Kilmer S, Haywood J, Lehner D (2019) Ethylene oxide exposure attribution and emissions quantification based on ambient air measurements near a sterilization facility. Int J Environ Res Public Health 17
Silva A, Dos Santos MJ, Goes Gitai DL, de Miranda Coelho JAP, de Andrade TG (2020) Depression and anxiety symptoms correlate with diurnal preference, sleep habits, and Per3 VNTR polymorphism (rs57875989) in a non-clinical sample. J Affect Disord 277:260–270
Steenland K, Stayner L, Deddens J (2004) Mortality analyses in a cohort of 18 235 ethylene oxide exposed workers: follow up extended from 1987 to 1998. Occup Environ Med 61:2–7
Tzeng IS (2021) To handle the inflation of odds ratios in a retrospective study with a profile penalized log-likelihood approach. J Clin Lab Anal 35:e23849
Urbiztondo M, Ramirez A, Hueso JL, Santamaria J, Ruiz-Salvador AR, Hamad S (2022) Unravelling the key factors in the chlorine-promoted epoxidation of ethylene over a silver-copper oxide nanocatalyst. Nanoscale 14:7332–7340
Wang G, Zhang J, Lam SP, Li SX, Jiang Y, Sun W, Chan NY, Kong APS, Zhang Y, Li S, Li AM, Jiang F, Shen X, Wing YK (2019) Ten-year secular trends in sleep/wake patterns in Shanghai and Hong Kong school-aged children: A Tale of Two Cities. J Clin Sleep Med 15:1495–1502
Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Dinges DF, Gangwisch J, Grandner MA, Kushida C, Malhotra RK, Martin JL, Patel SR, Quan SF, Tasali E (2015) Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 38:843–844
Wu N, Cao W, Wang Y, Liu X (2022) Association between blood ethylene oxide levels and the prevalence of hypertension. Environ Sci Pollut Res Int 29:76937–76943
Xie J, Li Y, Zhang Y, Vgontzas AN, Basta M, Chen B, Xu C, Tang X (2021) Sleep duration and metabolic syndrome: an updated systematic review and meta-analysis. Sleep Med Rev 59:101451
Zeng G, Zhang Q, Wang X, Wu KH (2021) Association between blood ethylene oxide levels and the risk of cardiovascular diseases in the general population. Environ Sci Pollut Res Int 28:64921–64928
Zhang J, Zhang J, Wu H, Wang R (2022a) Sleep duration and risk of hyperlipidemia: a systematic review and meta-analysis of prospective studies. Sleep Breath 26:997–1010
Zhang MM, Ma Y, Du LT, Wang K, Li Z, Zhu W, Sun YH, Lu L, Bao YP, Li SX (2022b) Sleep disorders and non-sleep circadian disorders predict depression: A systematic review and meta-analysis of longitudinal studies. Neurosci Biobehav Rev 134:104532
Zhu X, Kong X, Chen M, Shi S, Cheang I, Zhu Q, Lu X, Yue X, Tang Y, Liao S, Zhou Y, Zhang H, Yao W, Li X (2022) Blood ethylene oxide, systemic inflammation, and serum lipid profiles: Results from NHANES 2013-2016. Chemosphere 299:134336
Funding
This work was supported by the Natural Science Basic Research Program of Shaanxi (2020JQ-952). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
LH conceived and designed the study. QW extracted and analyzed data. LH and QW wrote the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All data used in this study were accessed from NHANES, a continuous program performed by the National Center for Health Statistics.
Consent to participate
Not applicable.
Consent to publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Han, L., Wang, Q. Association between hemoglobin adducts of ethylene oxide levels and the risk of short sleep duration in the general population: an analysis based on the National Health and Nutrition Examination Survey. Environ Sci Pollut Res 30, 76761–76768 (2023). https://doi.org/10.1007/s11356-023-27734-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-023-27734-3