Abstract
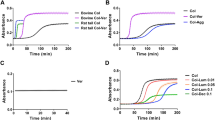
The extracellular matrix (ECM) of the prostate, which is comprised primarily of collagen, becomes increasingly disorganized with age, a property that may influence the development of hyperplasia and cancer. Collageous ECM extracted from the tails of aged mice exhibits many characteristics of collagen in aged tissues, including the prostate. When polymerized into a 3-dimensional (3D) gel, these collagen extracts can serve as models for the study of specific cell-ECM interactions. In the present study, we examined the behaviors of human prostatic epithelial cell lines representing normal prostate epithelial cells (PEC), benign prostatic hyperplasia (BPH-1), and adenocarcinoma (LNCaP) cultured in contact with 3D gels made from collagen extracts of young and aged mice. We found that proliferation of PEC, BPH-1, and LNCaP cells were all increased by culture on aged collagen gels relative to young collagen gels. In examining age-associated differences in the composition of the collagen extracts, we found that aged and young collagen had a similar amount of several collagen-associated ECM components, but aged collagen had a much greater content of the glycosaminoglycan hyaluronan (HA) than young collagen. The addition of HA (of similar size and concentration to that found in aged collagen extracts) to cells placed in young collagen elicited significantly increased proliferation in BPH-1 cells, but not in PEC or LNCaP cells, relative to controls not exposed to HA. Of note, histochemical analyses of human prostatic tissues showed significantly higher expression of HA in BPH and prostate cancer stroma relative to stroma of normal prostate. Collectively, these results suggest that changes in ECM involving increased levels of HA contribute to the growth of prostatic epithelium with aging.




Similar content being viewed by others
References
Afratis N, Gialeli C, Nikitovic D, Tsegenidis T, Karousou E, Theocharis AD, Pavão MS, Tzanakakis GN, Karamanos NK (2012) Glycosaminoglycans: key players in cancer cell biology and treatment. FEBS J 279:1177–1197
Bartling B, Desole M, Rohrbach S, Silber RE, Simm A (2009) Age-associated changes of extracellular matrix collagen impair lung cancer cell migration. FASEB J 23:1510–1520
Begley LA, Kasina S, MacDonald J, Macoska JA (2008) The inflammatory microenvironment of the aging prostate facilitates cellular proliferation and hypertrophy. Cytokine 43:194–199
Bentov I, Damodarasamy M, Plymate S, Reed MJ (2013) B16/F10 tumors in aged 3D collagen in vitro simulate tumor growth and gene expression in aged mice in vivo. In Vitro Cell Dev Biol Anim 49:395–399
Bharadwaj AG, Rector K, Simpson MA (2007) Inducible hyaluronan production reveals differential effects on prostate tumor cell growth and tumor angiogenesis. J Biol Chem 282:20561–20572
Bianchi-Frias D, Vakar-Lopez F, Coleman M, Plymate SR, Reed MJ, Nelson PS (2010) The effects of aging on the molecular and cellular composition of the prostate microenvironment. PLoS One 1:5–10
Bradshaw AD, Baicu CF, Rentz TJ, Van Laer AO, Bonnema DD, Zile MR (2010) Age-dependent alterations in fibrillar collagen content and myocardial diastolic function: role of SPARC in post-synthetic procollagen processing. Am J Physiol Heart Circ Physiol 298:H614–H622
Cukierman E, Pankov R, Stevens DR, Yamada KM (2001) Taking cell-matrix adhesions to the third dimension. Science 294:1708–1712
Damodarasamy M, Johnson RS, Bentov I, MacCoss MJ, Vernon RB, Reed MJ (2014) Hyaluronan enhances wound repair and increases collagen III in aged dermal wounds. Wound Repair Regen (in press)
Damodarasamy M, Vernon RB, Karres N, Chang H, Bianchi-Frias D, Nelson PS, Reed MJ (2010) Collagen extracts derived from young and aged mice demonstrate different structural properties and cellular effects in three-dimensional gels. J Gerontol A Biol Sci Med Sci 65:209–218
David-Raoudi M, Tranchepain F, Deschrevel B, Vincent JC, Bogdanowicz P, Boumediene K, Pujol JP (2008) Differential effects of hyaluronan and its fragments on fibroblasts: relation to wound healing. Wound Repair Regen 16:274–287
De Klerk DP (1983) The glycosaminoglycans of normal and hyperplastic prostate. Prostate 4:73–81
Ershler WB, Stewart JA, Hacker P, Moore AL, Tindle BH (1984) B16 murine melanoma and aging: slower growth and longer survival in old mice. J Natl Cancer Inst 72:161–164
Ghazi K, Deng-Pichon U, Warnet JM, Rat P (2012) Hyaluronan fragments improve wound healing on in vitro cutaneous model through P2X7 purinoreceptor basal activation: role of molecular weight. PLoS One 7:e48351
Goldberg RL, Toole BP (1987) Hyaluronate inhibition of cell proliferation. Arthritis Rheum 30:769–778
Goulas A, Hatzichristou DG, Karakiulakis G, Mirtsou-Fidani V, Kalinderis A, Papakonstantinou E (2000) Benign hyperplasia of the human prostate is associated with tissue enrichment in chondroitin sulphate of wide size distribution. Prostate 44:104–110
Grönberg H, Damber JE, Jonsson H, Lenner P (1994) Patient age as a prognostic factor in prostate cancer. J Urol 152:892–895
Haas TL, Davis SJ, Madri JA (1998) Three-dimensional type I collagen lattices induce coordinate expression of matrix metalloproteinases MT1-MMP and MMP-2 in microvascular endothelial cells. J Biol Chem 273:3604–3610
Harrison DE, Archer JR (1978) Measurement of changes in mouse tail collagen with age: temperature dependence and procedural details. Exp Gerontol 3:75–82
Hayward SW, Dahiya R, Cunha GR, Bartek J, Deshpande N, Narayan P (1995) Establishment and characterization of an immortalized but non-transformed human prostate epithelial cell line: BPH-1. In Vitro Cell Dev Biol Anim 31:14–24
Horoszewicz JS, Leong SS, Chu TM, Wajsman ZL, Friedman M, Papsidero L, Kim U, Chai LS, Kakati S, Arya SK, Sandberg AA (1980) The LNCaP cell line—a new model for studies on human prostatic carcinoma. Prog Clin Biol Res 37:115–132
Iozzo RV, Sanderson RD (2011) Proteoglycans in cancer biology, tumour microenvironment and angiogenesis. J Cell Mol Med 5:1013–1031
Jarvelainen H, Sainio A, Koulu M, Wight TN, Penttinen R (2009) Extracellular matrix molecules: potential targets in pharmacotherapy. Pharmacol Rev 61:198–223
Jiang ST, Liao KK, Liao MC, Tang MJ (2000) Age effect of type I collagen on morphogenesis of Madin-Darby canine kidney cells. Kidney Int 57:1539–1548
Kovar JL, Johnson MA, Volcheck WM, Chen J, Simpson MA (2006) Hyaluronidase expression induces prostate tumor metastasis in an orthotopic mouse model. Am J Pathol 169:1415–1426
Lee GY, Kenny PA, Lee EH, Bissell MJ (2007) Three-dimensional culture models of normal and malignant breast epithelial cells. Nat Methods 4:359–365
Leventhal KR, Yu H, Kass L, Lakins JN, Egeblad M, Erler JT, Fong SF, Csiszar K, Giaccia A, Weninger W, Yamauchi M, Gasser DL, Weaver VM (2009) Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell 139:891–906
Lokeshwar VB, Lokeshwar BL, Pham HT, Block NL (1996) Association of elevated levels of hyaluronidase, a matrix-degrading enzyme, with prostate cancer progression. Cancer Res 56:651–657
Lokeshwar VB, Rubinowicz D, Schroeder GL, Forgacs E, Minna JD, Block NL, Nadji M, Lokeshwar BL (2001) Stromal and epithelial expression of tumor markers hyaluronic acid and HYAL1 hyaluronidase in prostate cancer. J Biol Chem 276:11922–11932
Maharjan A, Pilling D, Gomer RH (2011) High and low molecular weight hyaluronic acid differentially regulate human fibrocyte differentiation. PLoS One 6:e26078
Miron-Mendoza M, Seemann J, Grinnell F (2010) The differential regulation of cell motile activity through matrix stiffness and porosity in three dimensional collagen matrices. Biomaterials 31:6425–6435
Misra S, Toole BP, Ghatak S (2006) Hyaluronan constitutively regulates activation of multiple receptor tyrosine kinases in epithelial and carcinoma cells. J Biol Chem 281:34936–34941
Ng MR, Brugge JS (2009) A stiff blow from the stroma: collagen crosslinking drives tumor progression. Cancer Cell 16:455–457
Orgel JP, San Antonio JD, Antipova O (2011) Molecular and structural mapping of collagen fibril interactions. Connect Tissue Res 52:2–17
Petrie RJ, Gavara N, Chadwick RS, Yamada KM (2012) Nonpolarized signaling reveals two distinct modes of 3D cell migration. J Cell Biol 197:439–455
Provenzano PP, Inman DR, Eliceiri KW, Knittel JG, Yan L, Rueden CT, White JG, Keely PJ (2008) Collagen density promotes mammary tumor initiation and progression. BMC Med 6:11–22
Pullen M, Thomas K, Wu H, Nambi P (2001) Stimulation of hyaluronan synthetase by platelet-derived growth factor bb in human prostate smooth muscle cells. Pharmacology 62:103–106
Reed MJ, Damodarasamy M, Chan CK, Johnson MN, Wight TN, Vernon RB (2013) Cleavage of hyaluronan is impaired in aged dermal wounds. Matrix Biol 32:45–51
Roughley PJ, Lamplugh L, Lee ER, Matsumoto K, Yamaguchi Y (2011) The role of hyaluronan produced by Has2 gene expression in development of the spine. Spine 36:E914–E920
Saad M, Abdel-Rahim M, Abol-Enein H, Ghoneim MA (2008) Concomitant pathology in the prostate in cystoprostatectomy specimens: a prospective study and review. BJU Int 102:1544–1550
Sadoun E, Reed MJ (2003) Impaired angiogenesis in aging is associated with alterations in vessel density, matrix composition, inflammatory response, and growth factor expression. J Histochem Cytochem 51:1119–1130
Sakr SW, Potter-Perigo S, Kinsella MG, Johnson PY, Braun KR, Goueffic Y, Rosenfeld ME, Wight TN (2008) Hyaluronan accumulation is elevated in cultures of low density lipoprotein receptor-deficient cells and is altered by manipulation of cell cholesterol content. J Biol Chem 283:36195–36204
Shi ZD, Wang H, Tarbell JM (2011) Heparan sulfate proteoglycans mediate interstitial flow mechanotransduction regulating MMP-13 expression and cell motility via FAK-ERK in 3D collagen. PLoS One 6:15956
Simpson MA, Lokeshwar VB (2008) Hyaluronan and hyaluronidase in genitourinary tumors. Front Biosci 13:5664–5680
Sprenger CC, Plymate SR, Reed MJ (2010) Aging-related alterations in the extracellular matrix modulate the microenvironment and influence tumor progression. Int J Cancer 127:2739–2748
Stern R, Maibach HI (2008) Hyaluronan in skin: aspects of aging and its pharmacologic modulation. Clin Dermatol 26:106–122
Tian X, Azpurua J, Hine C, Vaidya A, Myakishev-Rempel M, Ablaeva J, Mao Z, Nevo E, Gorbunova V, Seluanov A (2013) High-molecular-mass hyaluronan mediates the cancer resistance of the naked mole rat. Nature 499:346–349
Toole BP (2004) Hyaluronan: from extracellular glue to pericellular cue. Nat Rev Cancer 4:528–539
Underhill CB (1993) Hyaluronan is inversely correlated with the expression of CD44 in the dermal condensation of the embryonic hair follicle. J Invest Dermatol 101:820–826
Vernon RB, Sage EH (1999) A novel quantitative model for study of endothelial cell migration and sprout formation within three-dimensional collagen matrices. Microvasc Res 57:118–133
Wilkinson TS, Potter-Perigo S, Tsoi C, Altman LC, Wight TN (2004) Pro- and anti-inflammatory factors cooperate to control hyaluronan synthesis in lung fibroblasts. Am J Respir Cell Mol Biol 31:92–99
Wu CC, Ding SJ, Wang YH, Tang MJ, Chang HC (2005) Mechanical properties of collagen gels derived from rats of different ages. J Biomater Sci Polym Ed 16:1261–1275
Acknowledgments
The authors wish to thank Drs. Daniella Bianchi-Frias, Cynthia Sprenger, and Amy Bradshaw for helpful discussions, and Virginia M. Green, PhD, for editorial review of the manuscript.
Conflict of interest
The authors have no conflicts of interest to declare.
Contract/grant sponsor
R21 AG033391 NIA/NIH (M.J.R.); R01 EB012558, NIBIB/NIH (R.B.V./T.N.W)
Author information
Authors and Affiliations
Corresponding author
Additional information
Editor: T. Okamoto
Rights and permissions
About this article
Cite this article
Damodarasamy, M., Vernon, R.B., Chan, C.K. et al. Hyaluronan in aged collagen matrix increases prostate epithelial cell proliferation. In Vitro Cell.Dev.Biol.-Animal 51, 50–58 (2015). https://doi.org/10.1007/s11626-014-9800-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11626-014-9800-z