Abstract
Background
Effective strategies should be adopted to reduce care burden (CB) and improve health-related quality of life (HRQoL) in family caregivers (FCGs) of elderly people with Alzheimer's disease (AD). Therefore, the purpose of this study was to determine the impact of empowerment program (EP) on CB and HRQoL of FCGs.
Methods
The present two-group experimental study was conducted on 70 FCGs of the elderly with AD who were selected by convenience sampling and randomly assigned to the empowerment program group (EPG, n = 35) and control group (CG, n = 35). Data collection tools were 12-item Short Form Health Survey and Zarit Burden Interview. The EP was held for 5 weeks, one session of 20 to 30 min each week. Data were collected before, immediately and 3 months after EP and analyzed by SPSS version 25 software at a significance level of 0.05.
Results
The results showed a significant decrease in the mean CB score in FCGs of elderly with AD in EPG before, immediately and 3 months after EP (p < 0.001). The result also revealed that there was a significant increase in the mean HRQoL score in EPG immediately and 3 months after EP (p < 0.001).
Conclusions
According to the results of this study, EP can reduce CB and increase HRQoL in FCGs of elderly with AD. Policymakers and planners active in the field of healthcare for the elderly can benefit from the results of our study to improve the health of FCGs of the elderly with AD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer's disease (AD), a chronic progressive neurodegenerative condition, is associated with cognitive dysfunction, emotional disturbance, and abnormal mental behavior. Although pharmacotherapy can delay the progression of AD, there are still no effective measures in this field, and thus patients gradually lose the ability to perform their daily life activities, work, and social interactions [1]. According to the World Alzheimer Report, it is estimated that 46.8 million people worldwide are suffering from dementia and every year 9.9 million people are added to this statistic [2]. According to Iran Dementia and Alzheimer's Association (IDAA), there is no accurate statistics of AD patients in Iran, and probably 500,000 people in Iran are suffering from this disease. Due to the increase in the elderly population in Iran, it is expected that 25% of the elderly population in the country will become elderly in the next two to three decades, and 8–10% of this population will be affected by this disease due to the relationship between AD and aging [3].
In the elderly with AD, the patient's need for care increases with the progression of the disease, so that the person needs 24-h care in the final stages of the disease [4].
In developing countries, such as Iran, due to insufficient AD services in the community and the dependence of patients on their families in performing daily life activities, more burden is imposed on their family caregivers (FCGs) [5]. FCGs are family members (such as spouses or other family members) who provide unpaid care for an elderly person [6].
Although FCGs may experience emotional rewards and personal growth in the process of caring for their loved ones, many studies have reported the negative impact of the caregiving role on caregivers' physical health, emotional state, and financial stability [7]. In fact, caring for these patients causes changes in the lives of FCGs, including lack of time, reduced emotional feeling, disruption in social life, feeling of losing control over personal life, and physical and mental stress. These factors can be a precursor to all kinds of acute and chronic diseases [8]. Studies have shown that the FCGs of patients with AD are at risk of stress, depression, sleep disorder and physical problems, in other words, they are exposed to care burden (CB) [9], so that the disturbance can be caused in their quality of life (QoL) and even their body physiology. The incapacity, despair, weariness and loneliness experienced by caregivers to AD patients are the invisible parts of the iceberg of this disease [10].
Care burden is a general term used to describe the physical, emotional, social and financial costs of care. The CB is defined as the result of an imbalance between patient's demands and caregiver's resources. Such imbalance is related to the multiplicity of caregiver roles, physical and mental condition, their financial resources and the quality of government care services [11]. A high care burden of FCGs may lead to family isolation, deprivation of social support, disruption of family relationships, insufficient care of the patient, and ultimately leaving the patient [12]. Caring for an elderly person with AD not only leads to a care burden on FCGs, but also affects their QoL and leads to negative health outcomes [13].
While QoL encompasses a broad multidimensional assessment of the individual's intrapersonal system and individual–environmental system, and the individual's perception of the aging process and personal identity, health-related quality of life (HRQoL) focuses on how a person's physical and mental health affects daily life [14]. HRQoL as a multidimensional concept connects multiple aspects of health, such as physical, mental, emotional and social functioning [15]. In recent years, academics have begun to pay attention to the HRQoL of FCGs [1].
Studies have shown that QoL in FCGs of elderly people with AD is lower than that in FCGs of other chronic diseases, such as cancer [16]. Many studies claimed that QoL and CB of FCGs are among the most necessary variables that should be considered in the field of caring for the elderly [17], and that it seems necessary to implement effective strategies to reduce the CB in FCGs of the elderly with AD and change their QoL to prevent the worsening of the condition [7, 18]. Empowerment program (EP) is one of the strategies effectively influencing the FCGs in terms of motivation, psychology, knowledge and attitude toward the care of a sick family member and leading to health promotion [19]. Empowerment is a process capable of promoting perceived self-efficacy, during which people can recognize the real cause of the problem, solve it wisely, and share their knowledge and skills with the healthcare team. The process of sharing information increases perceived self-efficacy, thus leading to the adoption of appropriate behavior [15].
Literature review
Studies have been conducted on the effect of various interventions on CB and HRQoL of FCGs of patients with AD, dementia or other brain disorders, such as stroke. Van der Heide et al. evaluated the effects of an educational intervention on HRQoL among FCGs of people with dementia with Turkish or Moroccan immigrant background using a cluster randomized controlled trial [20]. Yoon and Kim in 2020 studied the effect of empowerment program on self-efficacy, well-being and adaptation of FCGs of people with dementia [21]. Aydin et al. conducted a study in Turkey in 2020 regarding the effect of educational program on QoL and CB for caregivers of patients with AD [22]. Another study investigated the effect of patient care education on CB and QoL of stroke patients' caregivers [23]. Cheng et al. investigated the long-term effects of a combined program of psychological rehabilitation and positive caregiving effects on depressive symptoms, FCGs (primary outcome) and overall CB, care burden role, psychological well-being and positive aspects of caregiving (secondary outcomes) [24]. In another study, Leszko investigated the effectiveness of a psychoeducational and financial intervention to support FCGs of people with AD in Poland [25]. Considering the importance of achieving strategies to reduce CB and improve HRQoL for FCGs of elderly with AD to improve health, the current work aimed to determine the impact of EP on CB and HRQoL in FCGs of elderly with AD. In this regard, the two hypotheses of our study are as follows:
H1: EP can be effective on CB in FCGs of elderly with AD.
H2: EP can be effective on HRQoL in FCGs of elderly with AD.
Methods
Study design and setting
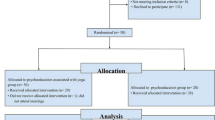
The present experimental study was conducted with two parallel groups in IDAA, and single blind design, so that the participants of the empowerment program group (EPG) and control group (CG) were unaware of the group assignment. CONSORT flow chart of the study is shown in Fig. 1.
Participants and recruitment
The study was conducted on 72 FCGs of elderly people with AD referred to IDAA. Based on the study of Yoon and Kim [21] and considering type I error of 0.05, type II error of 0.10 and test power of 0.90, and including the dropout-rate of 10%, the sample size was estimated at 36 people in each of EPG and CG.
To select FCGs, first, the records of patients with AD who were members of IDAA were reviewed. Among the 128 medical records of patients with AD, 37 were excluded from the study due to ineligibility of FCGs, and five FCGs were unwilling to participate in the study. 91 of the selected FCGs of AD patients were randomly assigned to EPG (n = 46) and CG (n = 45) based on coin toss. In the EPG, three FCGs were excluded due to non-participation in the EP, three due to COVID-19 infection, and three due to incomplete presentation of the instruments. In CG, three FCGs were excluded from the study due to disconnection with IDAA, 3 due to changing the role of the first FCGs, and 3 due to not completing the instruments. In total, 35 FCGs of patients with AD participated in the study in both groups.
The inclusion criteria were a history of being a FCG for an elderly person with AD, age range of 18–55 years, caring for an elderly person with AD for at least 6 months, full listening-speaking ability, and literacy. Exclusion criteria were the death of the elderly patient, getting involved with another disease during the study, transferring the elderly to a nursing home, not participating in at least half of the educational classes, and incomplete study tools.
Outcome measurements
The outcomes of this study included changes in CB and HRQoL of FCGs of elderly with AD, measured in three stages including baseline (before EP), follow-up 1 (immediately after EP) and follow-up 2 (3 months after EP).
Measures
Demographic information questionnaire
The demographic information questionnaire contained six items regarding the demographic profile of the elderly with AD, including age, gender, marital status, educational level, income adequacy, and underlying diseases, and contained seven items about the demographic profile of FCGs of elderly with AD participating in the study including age, gender, educational level, marital status, income adequacy, duration of care for the elderly with AD and underlying disease.
12-item short form health survey
The 12-item Short Form Health Survey (SF-12) was used to measure HRQoL. The SF-12 consists of 12 questions and measures HRQoL in two mental and physical subscales. The minimum score obtained from this survey is 12 and the maximum is 48. The higher score, the higher HRQoL [26]. In this article, HRQoL results are reported as a set of both subscales and total. The validity and reliability of this instrument in Persian has already been confirmed [27].
Zarit Burden Interview
The 22-item Zarit Burden Interview (ZBI) was used to measure CB. This tool was developed by Zarit et al. among American FCGs of elderly people with dementia [28]. This tool measures mental stress caused by caregiving. Each item is rated on a 5-point Likert scale from never (score zero) to nearly always (score 4). The total scores of the questionnaire items vary between 0 and 88, and the higher score, the higher care burden [29]. This tool has been validated by Bagherbeik Tabrizi et al. in Persian and for a sample of FCGs for patients with AD [4].
In the current study, the validity of SF-12 and ZBI was examined using content validity by 10 faculty members of the Faculty of Nursing and Midwifery of the University of Medical Sciences and 5 FCGs of the elderly with AD, and any word ambiguity was resolved. Reliability was determined using the test–retest reliability method and Cronbach's alpha coefficient. To determine the test–retest reliability of SF-12 and ZBI, both instruments were completed twice with an interval of 2 weeks by 10 FCGs of elderly people with AD outside the study, and intraclass correlation was calculated, which was obtained for both tools, 0.91 and 0.89, respectively. Cronbach's alpha coefficient was calculated after completing the instruments by 20 FCGs of elderly people with AD outside the study, which were obtained as 0.89 and 0.90, respectively. Considering that the reliability above 0.7 is accepted [30], in this sense both instruments were approved.
Empowerment program
In this study, the EP was set based on the one developed and implemented by Yoon and Kim for FCGs of elderly people with dementia [21]. Content validity of EP was checked and confirmed by two faculty members of the Faculty of Nursing and Midwifery and one member of IDAA. The purpose of EP was to increase the knowledge and improve the performance of FCGs in patient care and to improve physical, mental and spiritual health along with the ability to make decisions and solve problems. After selecting the participants and allocating them in EPG and CG, necessary arrangements were made regarding the time and place of holding EP with FCGs selected for EPG. The program sessions were given in groups of 7–10 people. Prior to the EP, the grouping of FCGs for how and when to implement the EP was set with participation. The program was implemented in 5 weeks as a 20–30-min session every week (Table 1). Training was held for the FCGs of EPG face-to-face, discussion and exchange of opinions and using educational media such as video projector and PowerPoint in the training room located in IDAA.
Data analysis
Data were analyzed using SPSS version 25 software. Chi-square test and Mann–Whitney U test were used to compare demographic variables of EPG and CG. The normality of data distribution was checked using the Kolmogorov–Smirnov test. Inter-group comparisons for CB and HRQoL in different phases of the study were performed by independent t test, repeated measures ANOVA, Mann–Whitney U test and Friedman's test. Dependent t test and Wilcoxon signed-rank test were used for pairwise comparison of different stages of the study in terms of CB and HRQoL. A significance level of less than 0.05 was considered significant.
Results
Baseline information of participants
The results of the study showed that the mean age of elderly with AD was 74.8 ± 5.8 years in EPG and 73.6 ± 2.6 years in CG and the mean age of FCGs for elderly with AD was 47.4 ± 5.9 in EPG and 45.7 ± 5.7 in CG. Other demographic information is given in Table 2. There was no significant difference between EPG and CG in terms of all the demographic variables related to the elderly with AD and their FCGs (Table 2).
CB changes in EPG and CG
The results of Table 3 and Fig. 2 showed no significant difference in the mean CB score between EPG and CG at the baseline, but the significant difference in this parameter during follow-up 1 and follow-up 2 between the two groups (p < 0.001). In the intra-group comparison, the results of the repeated measures ANOVA test showed that the mean CB score for FCGs in EPG from baseline to follow-up 2 was associated with a significant decrease, while this variable in CG had a significant increase (p < 0.001). The results of the Wilcoxon test for pairwise comparisons between study stages in EPG also showed that there was a significant difference between the mean CB scores at the baseline stage with follow-up 1 and follow-up 2, as well as between follow-up 1 and follow-up 2 (p < 0.001), with the difference that the difference in the mean CB scores was negative and decreasing in EPG and positive and increasing in CG (Table 4).
HRQoL changes in EPG and CG
The results of the Mann–Whitney test in Table 4 and Fig. 2 showed that there was no significant difference in the mean HRQoL score between EPG and CG at the baseline, but this score was significantly different between the two groups during follow-up 1 and follow-up 2 (p < 0.001). In the intra-group comparison, the Friedman's test results showed that the mean HRQoL score for FCGs in EPG from baseline to follow-up 2 was associated with a significant increase, while this variable decreased significantly in CG (p < 0.001). The results of the dependent t test for pairwise comparisons between the stages of the study showed that, in both EPG and CG, there was a significant difference in the mean HRQoL score for FCGs between baseline and both follow-up 1 and follow-up 2, as well as between follow-up 1 and follow-up 2 (p < 0.001), with the difference that the mean difference in HRQoL scores was positive and increasing in EPG and negative and decreasing in CG (Table 4).
Absolute changes of CB and HRQoL
Linear mixed model was used to evaluate the absolute changes of CB and HRQoL from baseline to follow-up 2 by controlling demographic variables of FCGs, including age, gender, marital status, educational level, occupation, income adequacy and family relationship with an elderly person with AD (Table 5). The results from the first part of the linear mixed model revealed that the CB score after EP implementation in EPG was significantly lower than CG by 7.361 units (p < 0.001, 95% CI = – 9.027 to – 5.696). Although the decrease in CB score in follow-up 1 was insignificant, it was reduced by 5.014 units in follow-up 2 compared to baseline (p < 0.001, 95% CI = – 7.054 to – 20,974).
The second part of the results from the linear model showed that the HRQoL score after the implementation of EP in EPG was significantly higher than CG by 5.611 units (p < 0.001, 95% CI = 4.765–6.457), so that it increased by 2.417 units in follow-up 1 (p < 0.001, 95% CI = 1.381–3.452) and by 4.167 units in follow-up 2 (p < 0.001, 95% CI = 3.131–5.202).
Discussion
The results of our study revealed that EP was effective in reducing CB and increasing HRQoL among FCGs of the elderly with AD, thus confirming both study hypotheses.
Concerning the first hypothesis, the findings showed that the coherent and multifaceted EP with the aim of empowering FCGs of the elderly with AD in the dimensions of patient care, physical, mental and spiritual self-care and strengthening the decision-making power could lead to the reduction of CB in FCGs of the elderly with AD. Other studies have also reported similar obtains. Bagherbeik Tabrizi et al. reported that the cognitive–behavioral intervention could reduce CB in FCGs of elderly with AD [4]. Pahlavanzadeh et al. also studied the impact of a family education program on the CB of FCGs of elderly with dementia disorders, which used educational content on how to care for patients and control their behaviors. Their data indicated a decrease in CB following the implementation of the education program focused on the care of the patient with dementia [31]. The educational content implemented by Pahlavanzadeh et al. focused more on the details of the patient care, while the EP content was more comprehensive in the present study and emphasized FCGS's self-care. In a clinical trial, Terracciano et al. demonstrated that the implementation of an education program for FCGs of people with dementia based on self-care, emotional control and emotional distress was able to reduce CB and improve mental health of FCGs [32]. Given that the content of the EP in the present study also focused on self-care and spiritual care, it can be claimed that the results of Terracciano et al. are in line with the results of our study.
Concerning the second hypothesis, the results showed that the coherent and multifaceted EP with the aim of empowering FCGs of the elderly with AD in the dimensions of patient care, physical, mental and spiritual self-care and strengthening the decision-making power could improve the HRQoL of FCGs of the elderly with AD. Similarly, Yang et al. showed that a comprehensive intervention focusing on the elderly with AD and their FCGs could improve the QoL of FCGs [33]. Yoon and Kim found that the EP significantly increased the welfare of FCGs of elderly with dementia [21]. Kuzu and Aydın also determined that the educational program emphasizing how to care for the elderly with chronic obstructive pulmonary disease could increase the QoL of their FCGs [34].
Our work is a valuable study in the sense that it focused on a vulnerable group of society, i.e., the FCGs of the elderly with AD, and was able to determine the effect of a comprehensive, multilateral intervention on two important their health-related variables, i.e., CB and HRQoL. Some of the limitations of this study were need to accuracy in answering the questions and in completing the questionnaire by participants as well as the influence of numerous individual, family and social factors on HRQL and CB that were out of control by the researcher.
Conclusions
The results obtained from the present study demonstrated that the empowerment program was able to reduce care burden and increase HRQoL for the FCGs of elderly with Alzheimer's disease. Accordingly, healthcare providers can benefit from this EP as a low-cost and practical strategy for improving the physical and mental health of the FCGs of elderly with AD in the environments and centers they are present or return. We also suggest that nursing planners and managers apply this EP with the content emphasized in this study as one of the indicators of unit performance evaluation and employee accreditation. Another suggestion is to conduct a study regarding the effect of EP on CB and HRQoL of FCGs of elderly people with other chronic diseases, such as stroke. Although this study was conducted in Iran, its results can be generalized to other countries.
References
Liao X, Huang Y, Zhang Z et al (2020) Factors associated with health-related quality of life among family caregivers of people with Alzheimer’s disease. Psychogeriatrics 20:398–405. https://doi.org/10.1111/psyg.12528
Viñas-Diez V, Turró-Garriga O, Portellano-Ortiz C et al (2017) Kinship and cohabitation in relation to caregiver burden in the context of Alzheimer’s disease: a 24-month longitudinal study. Int J Geriatr Psychiatry 32:e72–e82. https://doi.org/10.1002/gps.4656
Ravari A, Mirzaei T, Salamizadeh A et al (2017) Effect of the spiritual care training on anxiety reduction in home caregivers of the elderly with Alzheimer disease. Koomesh 19:467–474
Bagherbeik Tabrizi L, Navab E, Farokhnezhad AP et al (2015) Effect of cognitive-behavioral intervention on burden of family caregivers of patients with Alzheimer’s disease. HAYAT 21:94–102
Abdollahpour I, Nedjat S, Salimi Y (2018) Positive aspects of caregiving and caregiver burden: a study of caregivers of patients with dementia. J Geriatr Psychiatry Neurol 31:34–38. https://doi.org/10.1177/0891988717743590
Bailes CO, Kelley CM, Parker NM (2016) Caregiver burden and perceived health competence when caring for family members diagnosed with Alzheimer’s disease and related dementia. J Am Assoc Nurse Pract 28:534–540. https://doi.org/10.1002/2327-6924.12355
Lee M, Ryoo JH, Crowder J et al (2020) A systematic review and meta-analysis on effective interventions for health-related quality of life among caregivers of people with dementia. J Adv Nurs 76:475–489. https://doi.org/10.1111/jan.14262
Shafizadeh A, Mirzaee A, Heravi-Karimooi M et al (2020) Relationship between caregiver burden and demographic characteristics in caregivers of alzheimer’s elderly. J Nurs Educ 9:65–73
Lamotte G, Shah RC, Lazarov O et al (2017) Exercise training for persons with Alzheimer’s disease and caregivers: a review of dyadic exercise interventions. J Mot Behav 49:365–377. https://doi.org/10.1080/00222895.2016.1241739
Koca E, Taşkapilioğlu Ö, Bakar M (2017) Caregiver burden in different stages of Alzheimer’s disease. Noro Psikiyatr Ars 54:82–86. https://doi.org/10.5152/npa.2017.11304
Sinha P, Desai N, Prakash O et al (2017) Caregiver burden in Alzheimer-type dementia and psychosis: A comparative study from India. Asian J Psychiatr 26:86–91. https://doi.org/10.5152/npa.2017.11304
Jafari-Diziche S, Izadi-Avanji F-S, Atoof F et al (2021) Effect of family-centered empowerment model on the care burden of the caregivers of older adults with heart failure. JCCNC 7:275–84. https://doi.org/10.32598/JCCNC.7.4.305.3
Montgomery W, Goren A, Kahle-Wrobleski K et al (2018) Alzheimer’s disease severity and its association with patient and caregiver quality of life in Japan: results of a community-based survey. BMC Geriatr 18:141. https://doi.org/10.1186/s12877-018-0831-2
Fagerström C, Elmståhl S, Wranker LS (2020) Analyzing the situation of older family caregivers with a focus on health-related quality of life and pain: a cross-sectional cohort study. Health Qual Life Outcomes 18:79. https://doi.org/10.1186/s12955-020-01321-3.PMC7082916
Zafari Nobari S, Vasli P, Hosseini M et al (2021) Improving health-related quality of life and adherence to health-promoting behaviors among coronary artery bypass graft patients: a non-randomized controlled trial study. Qual Life Res 30:769–780. https://doi.org/10.1007/s11136-020-02675-3
Hazzan AA, Shannon H, Ploeg J et al (2016) The association between caregiver well-being and care provided to persons with Alzheimer’s disease and related disorders. BMC Res Notes 9:344. https://doi.org/10.1002/2327-6924.12355
Dehghani Y, Omranifard V, Babamiri M (2016) The effectiveness of communication skills training on caregiving burden and quality of life among family caregivers of elderly with dementia. J Res Behav Sci 14:161–167
Kawaharada R, Sugimoto T, Matsuda N et al (2019) Impact of loss of independence in basic activities of daily living on caregiver burden in patients with Alzheimer’s disease: A retrospective cohort study. Geriatr Gerontol Int 9:1243–1247. https://doi.org/10.1111/ggi.13803
Rahgoi A, Sojoodi T, Khoshknab MF et al (2019) Effects of empowerment program on the burden of care in mothers of children with phenylketonuria. Iran J Child Neurol 13:53
van der Heide I, van Wezel N, Blom M et al (2021) Effects of an educational intervention on health-related quality of life among family caregivers of people with dementia with a Turkish or Moroccan immigrant background: Insights from a cluster randomised controlled trial. Patient Educ Couns 104:1168–1175. https://doi.org/10.1016/j.pec.2020.10.029
Yoon HK, Kim GS (2020) An empowerment program for family caregivers of people with dementia. Public Health Nurs 37:222–233. https://doi.org/10.1111/phn.12690
Aydin HT, Tel H, Guler N et al (2020) Effect of an educational program on care burden and quality of life for caregivers of patients diagnosed with Alzheimer’s disease. J Health Med Nurs 75:43–47. https://doi.org/10.7176/JHMN/75-06
Hekmatpou D, Baghban EM, Dehkordi LM (2019) The effect of patient care education on burden of care and the quality of life of caregivers of stroke patients. J Multidiscip Healthc 12:211. https://doi.org/10.2147/JMDH.S196903
Cheng S-T, Mak EP, Kwok T et al (2020) Benefit-finding intervention delivered individually to Alzheimer family caregivers: longer-term outcomes of a randomized double-blind controlled trial. J Gerontol: Series B 75:1884–1893. https://doi.org/10.1093/geronb/gbz118
Leszko M (2019) The effectiveness of psychoeducational and financial intervention to support caregivers of individuals with Alzheimer’s disease in Poland. Innov Aging. https://doi.org/10.1093/geroni/igz026
Montazeri A, Vahdaninia M, Mousavi SJ et al (2011) The 12-item medical outcomes study short form health survey version 2.0 (SF-12v2): a population-based validation study from Tehran, Iran. Health Qual Life Outcomes 9:12
Montazeri A, Vahdaninia M, Mousavi SJ et al (2009) The Iranian version of 12-item Short Form Health Survey (SF-12): factor structure, internal consistency and construct validity. BMC Public Health 9:1–10. https://doi.org/10.1186/1471-2458-9-341
Zarit SH, Todd PA, Zarit JM (1986) Subjective burden of husbands and wives as caregivers: a longitudinal study. Gerontologist 26:260–266. https://doi.org/10.1093/geront/26.3.260
Yu Y, Liu Z-w, Li T-x et al (2020) A comparison of psychometric properties of two common measures of caregiving burden: the family burden interview schedule (FBIS-24) and the Zarit caregiver burden interview (ZBI-22). Health Qual Life Outcomes 18:1–9. https://doi.org/10.1186/s12955-020-01335-x
Vasli P (2018) Translation, cross-cultural adaptation, and psychometric testing of perception of family-centered care measurement questionnaires in the hospitalized children in Iran. J Pediatr Nurs 43:e26–e34. https://doi.org/10.1016/j.pedn.2018.08.004
Pahlavanzadeh S, Heidari FG, Maghsudi J et al (2010) The effects of family education program on the caregiver burden of families of elderly with dementia disorders. Iran J Nurs Midwifery Res 15:102
Terracciano A, Artese A, Yeh J et al (2020) Effectiveness of powerful tools for caregivers on caregiver burden and on care recipient behavioral and psychological symptoms of dementia: A randomized controlled trial. J Am Med Dir Assoc 21:1121–7.e1. https://doi.org/10.1016/j.jamda.2019.11.011
Yang L, Xuan C, Yu C et al (2022) Effects of comprehensive intervention on life quality among the elderly with Alzheimer Disease and their caregivers based on mixed models. Nurs Open 9:1412–1422. https://doi.org/10.1002/nop2.917
Kuzu F, Aydın HT (2022) Effects of education on care burden and quality of life to caregivers of patients with COPD. Turk Thorac J. https://doi.org/10.5152/TurkThoracJ.2022.21002
Acknowledgements
The authors hereby express their gratitude to the officials of Iran Dementia and Alzheimer's Association and all the family caregivers of the elderly with Alzheimer's disease, who participated in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors have no conflicts of interest to disclose.
Ethical statements
All the measures taken in this study were approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran (code no. IR.SBMU.PHARMACY.REC.1399.359) in agreement with the ethical standards of the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was also obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yazdanmanesh, M., Esmaeili, R., Nasiri, M. et al. Relieving care burden and promoting health-related quality of life for family caregivers of elderly people with Alzheimer’s disease via an empowerment program. Aging Clin Exp Res 35, 73–83 (2023). https://doi.org/10.1007/s40520-022-02277-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-022-02277-8