Abstract
Purpose of Review
Wildfire smoke is associated with human health, becoming an increasing public health concern. However, a comprehensive synthesis of the current evidence on the health impacts of ambient wildfire smoke on children and adolescents, an exceptionally vulnerable population, is lacking. We conduct a systematic review of peer-reviewed epidemiological studies on the association between wildfire smoke and health of children and adolescents.
Recent Findings
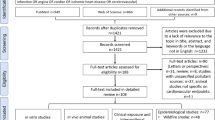
We searched for studies available in MEDLINE, EMBASE, and Scopus from database inception up to October 11, 2022. Of 4926 studies initially identified, 59 studies from 14 countries were ultimately eligible. Over 33.3% of the studies were conducted in the USA, and two focused on multi-countries. The exposure assessment of wildfire smoke was heterogenous, with wildfire-specific particulate matters with diameters ≤ 2.5 µm (PM2.5, 22.0%) and all-source (22.0%) PM2.5 during wildfire period most frequently used. Over half of studies (50.6%) focused on respiratory-related morbidities/mortalities. Wildfire smoke exposure was consistently associated with enhanced risks of adverse health outcomes in children/adolescents. Meta-analysis results presented a pooled relative risk (RR) of 1.04 (95% confidence interval [CI], 0.96-1.12) for all-cause respiratory morbidity, 1.11 (95% Ci: 0.93-1.32) for asthma, 0.93 (95% CI, 0.85–1.03) for bronchitis, and 1.13 (95% CI, 1.05–1.23) for upper respiratory infection, whilst − 21.71 g for birth weight (95% CI, − 32.92 to − 10.50) per 10 µg/m3 increment in wildfire-specific PM2.5/all-source PM2.5 during wildfire event.
Summary
The majority of studies found that wildfire smoke was associated with multiple adverse health outcomes among children and adolescents, with respiratory morbidities of significant concern. In-utero exposure to wildfire smoke may increase the risk of adverse birth outcomes and have long-term impacts on height. Higher maternal baseline exposure to wildfire smoke and poor family-level baseline birthweight respectively elevated risks in preterm birth and low birth weight associated with wildfire smoke. More studies in low- and middle-income countries and focusing on extremely young children are needed. Despite technological progress, wildfire smoke exposure measurements remain uncertain, demanding improved methodologies to have more precise assessment of wildfire smoke levels and thus quantify the corresponding health impacts and guide public mitigation actions.



Similar content being viewed by others
Data Availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
References
Xu R, Yu P, Abramson MJ, Johnston FH, Samet JM, Bell ML, Haines A, Ebi KL, Li S, Guo Y. Wildfires, global climate change, and human health. N Engl J Med. 2020;383:2173–81.
Kim YH, Warren SH, Krantz QT, King C, Jaskot R, Preston WT, George BJ, Hays MD, Landis MS, Higuchi M. Mutagenicity and lung toxicity of smoldering vs. flaming emissions from various biomass fuels: implications for health effects from wildland fires. Environ Health Perspect. 2018;126:017011.
Gao Y, Huang W, Yu P, Xu R, Yang Z, Gasevic D, Ye T, Guo Y, Li S. Long-term impacts of non-occupational wildfire exposure on human health: a systematic review. Environ Pollut. 2023;121041.
Ye T, Yu P, Wen B, Yang Z, Huang W, Guo Y, Abramson MJ, Li S. Greenspace and health outcomes in children and adolescents: a systematic review. Environ Pollut. 2022;314: 120193.
Henry S, Ospina MB, Dennett L, Hicks A. Assessing the risk of respiratory-related healthcare visits associated with wildfire smoke exposure in children 0–18 years old: a systematic review. Int J Environ Res Public Health. 2021;18:8799.
Arriagada NB, Horsley JA, Palmer AJ, Morgan GG, Tham R, Johnston FH. Association between fire smoke fine particulate matter and asthma-related outcomes: systematic review and meta-analysis. Environ Res. 2019;179: 108777.
Amjad S, Chojecki D, Osornio-Vargas A, Ospina MB. Wildfire exposure during pregnancy and the risk of adverse birth outcomes: a systematic review. Environ Int. 2021;156: 106644.
Holm SM, Miller MD, Balmes JR. Health effects of wildfire smoke in children and public health tools: a narrative review. J Expo Sci Environ Epidemiol. 2021;31:1–20.
PICO Portal. Transforming research findings into decision-ready evidence with ease. PICO Portal. 2023.
Palmer TM, Sutton AJ, Peters JL, Moreno SG. Contour-enhanced funnel plots for meta-analysis. STATA J. 2008;8:242–54.
Vandenbroucke J. Bias in meta-analysis detected by a simple, graphical test. Experts’ views are still needed. BMJ: Brit Med J. 1998;316:469.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Kondo MC, De Roos AJ, White LS, Heilman WE, Mockrin MH, Gross-Davis CA, Burstyn I. Meta-analysis of heterogeneity in the effects of wildfire smoke exposure on respiratory health in North America. Int J Environ Res Public Health. 2019;16:960.
Cimino AM, Boyles AL, Thayer KA, Perry MJ. Effects of neonicotinoid pesticide exposure on human health: a systematic review. Environ Health Perspect. 2017;125:155–62.
Woodruff TJ, Sutton P. The Navigation Guide systematic review methodology: a rigorous and transparent method for translating environmental health science into better health outcomes. Environ Health Perspects. 2014;122:1007–14.
C.D.o. Forestry, F. Protection. Top 20 largest California wildfires, CAL FIRE Sacramento, CA, USA. 2020.
Singh P, Dey S. Crop burning and forest fires: long-term effect on adolescent height in India. Resour Energy Econ. 2021;65: 101244.
Mott JA, Mannino DM, Alverson CJ, Kiyu A, Hashim J, Lee T, Falter K, Redd SC. Cardiorespiratory hospitalizations associated with smoke exposure during the 1997 Southeast Asian forest fires. Int J Hyg Environ Health. 2005;208:75–85.
Pinaev S. The influence of solar radiation and forest fire smoke on sporadic fluctuations of neoplasm incidence in children. RAD Conference Proceedings. 2020. pp 69–71.
Schumpert JC, Noonan CW, Sylvester J, Vanek D, Ward T, Holian A. Patterns of asthma symptoms and perceptions of harm from seasonal atmospheric events in rural Western Montana. Int J Occup Environ Health. 2006;12:52–8.
Reid E, Jerrett M, Tager IB, Petersen ML, Mann JK, Balmes JR. Differential respiratory health effects from the 2008 northern California wildfires: a spatiotemporal approach. Environ Res. 2016;150:227–35.
Haikerwal A, Akram M, Sim MR, Meyer M, Abramson MJ, Dennekamp M. Fine particulate matter (PM2.5) exposure during a prolonged wildfire period and emergency department visits for asthma. Respirology. 2016;21:88–94.
Yao J, Eyamie J, Henderson SB. Evaluation of a spatially resolved forest fire smoke model for population-based epidemiologic exposure assessment. J Expo Sci Environ Epidemiol. 2016;26:233–40.
Resnick A, Woods B, Krapfl H, Toth B. Health outcomes associated with smoke exposure in Albuquerque, New Mexico, during the 2011 Wallow fire. J Public Health Manag Pract: JPHMP. 2015;21(Suppl 2):S55-61.
Andrade Filho VS, Artaxo P, Hacon S, Carmo CN, Cirino G. Aerosols from biomass burning and respiratory diseases in children, Manaus, Northern Brazil. Rev Saude Publica. 2013;47:239–47.
Howard C, Rose C, Dodd W, Kohle K, Scott C, Scott P, Cunsolo A, Orbinski J. SOS! Summer of Smoke: a retrospective cohort study examining the cardiorespiratory impacts of a severe and prolonged wildfire season in Canada’s high subarctic. BMJ Open. 2021;11:e037029.
Alman BL, Pfister G, Hao H, Stowell J, Hu X, Liu Y, Strickland MJ. The association of wildfire smoke with respiratory and cardiovascular emergency department visits in Colorado in 2012: a case crossover study. Environ Health. 2016;15:64.
Delfino RJ, Brummel S, Wu J, Stern H, Ostro B, Lipsett M, Winer A, Street DH, Zhang L, Tjoa T, Gillen DL. The relationship of respiratory and cardiovascular hospital admissions to the southern California wildfires of 2003. Occup Environ Med. 2009;66:189–97.
Johnston FH, Webby RJ, Pilotto LS, Bailie RS, Parry DL, Halpin SJ. Vegetation fires, particulate air pollution and asthma: a panel study in the Australian monsoon tropics. Int J Environ Health Res. 2006;16:391–404.
Requia WJ, Amini H, Mukherjee R, Gold DR, Schwartz JD. Health impacts of wildfire-related air pollution in Brazil: a nationwide study of more than 2 million hospital admissions between 2008 and 2018. Nat Commun. 2021;12:6555.
Awasthi A, Singh N, Mittal S, Gupta PK, Agarwal R. Effects of agriculture crop residue burning on children and young on PFTs in North West India. Sci Total Environ. 2010;408:4440–5.
Shirangi A, Lin T, Iva’nova I, Yun G, Williamson GJ, Franklin P, Jian L, Burch R, Dewan A, Santos B, Eaton N, Xiao J. Exposure to fine particulate matter (PM2.5) during landscape fire events and the risk of cardiorespiratory emergency department attendances: a time-series study in Perth, Western Australia. J Epidemiol Commun Health. 2022;76:809–18.
Mahsin MD, Cabaj J, Saini V. Respiratory and cardiovascular condition-related physician visits associated with wildfire smoke exposure in Calgary, Canada, in 2015: a population-based study. Int J Epidemiol. 2022;51:166–78.
Lee T-S, Falter K, Meyer P, Mott J, Gwynn C. Risk factors associated with clinic visits during the 1999 forest fires near the Hoopa Valley Indian Reservation, California, USA. Int J Environ Health Res. 2009;19:315–27.
Kunzli N, Avol E, Wu J, Gauderman WJ, Rappaport E, Millstein J, Bennion J, McConnell R, Gilliland FD, Berhane K, Lurmann F, Winer A, Peters JM. Health effects of the 2003 Southern California wildfires on children. Am J Respir Crit Care Med. 2006;174:1221–8.
Uttajug A, Ueda K, Oyoshi K, Honda A, Takano H. Association between PM10 from vegetation fire events and hospital visits by children in upper northern Thailand. Sci Total Environ. 2021;764: 142923.
Henderson SB, Brauer M, Macnab YC, Kennedy SM. Three measures of forest fire smoke exposure and their associations with respiratory and cardiovascular health outcomes in a population-based cohort. Environ Health Perspect. 2011;119:1266–71.
Hutchinson JA, Vargo J, Milet M, French NHF, Billmire M, Johnson J, Hoshiko S. The San Diego 2007 wildfires and Medi-Cal emergency department presentations, inpatient hospitalizations, and outpatient visits: an observational study of smoke exposure periods and a bidirectional case-crossover analysis. PLoS Med. 2018;15: e1002601.
Hein L, Spadaro JV, Ostro B, Hammer M, Sumarga E, Salmayenti R, Boer R, Tata H, Atmoko D, Castañeda J-P. The health impacts of Indonesian peatland fires. Environ Health. 2022;21:1–16.
Heaney A, Stowell JD, Liu JC, Basu R, Marlier M, Kinney P. Impacts of fine particulate matter from wildfire smoke on respiratory and cardiovascular health in California, GeoHealth. 2022;e2021GH000578.
Li J, Guan T, Guo Q, Geng G, Wang H, Guo F, Li J, Xue T. Exposure to landscape fire smoke reduced birthweight in low-and middle-income countries: findings from a siblings-matched case-control study. Elife. 2021;10:e69298.
Tinling MA, West JJ, Cascio WE, Kilaru V, Rappold AG. Repeating cardiopulmonary health effects in rural North Carolina population during a second large peat wildfire. Environ Health. 2016;15:1–12.
Ye T, Guo Y, Chen G, Yue X, Xu R, de Sousa Zanotti Stagliorio Coelho M, Saldiva PHN, Zhao Q, Li S. Risk and burden of hospital admissions associated with wildfire-related PM2.5 in Brazil, 2000–15: a nationwide time-series study. Lancet Planet Health. 2021;5:e599–e607.
Xue T, Geng G, Li J, Han Y, Guo Q, Kelly FJ, Wooster MJ, Wang H, Jiangtulu B, Duan X, Wang B, Zhu T. Associations between exposure to landscape fire smoke and child mortality in low-income and middle-income countries: a matched case-control study. Lancet Planet Health. 2021;5:e588–98.
Stowell JD, Geng G, Saikawa E, Chang HH, Fu J, Yang C-E, Zhu Q, Liu Y, Strickland MJ. Associations of wildfire smoke PM2.5 exposure with cardiorespiratory events in Colorado 2011–2014. Environ Int. 2019;133:105151.
Abdo M, Ward I, O'Dell K, Ford B, Pierce JR, Fischer EV, Crooks JL. Impact of wildfire smoke on adverse pregnancy outcomes in Colorado, 2007–2015. Int J Environ Res Public Health. 2019;16.
Li J, Xue T, Tong M, Guan T, Liu H, Li P, Li J, Zhu T. Gestational exposure to landscape fire increases under-5 child death via reducing birthweight: a risk assessment based on mediation analysis in low- and middle-income countries. Ecotoxicol Environ Safety. 2022;240: 113673.
Mccoy SJ, Zhao X. Wildfire and infant health: a geospatial approach to estimating the health impacts of wildfire smoke exposure. Appl Econ Lett. 2021;28:32–7.
Aguilera R, Corringham T, Gershunov A, Leibel S, Benmarhnia T. Fine particles in wildfire smoke and pediatric respiratory health in California. Pediatrics. 2021;147.
Lipner EM, O’Dell K, Brey SJ, Ford B, Pierce JR, Fischer EV, Crooks JL. The associations between clinical respiratory outcomes and ambient wildfire smoke exposure among pediatric asthma patients at National Jewish Health, 2012–2015. GeoHealth. 2019;3:146–59.
Barbosa JV, Nunes RAO, Alvim-Ferraz MCM, Martins FG, Sousa SIV. Health and economic burden of the 2017 Portuguese Extreme wildland fires on children. Int J Environ Res Public Health. 2022;19:593.
Machado-Silva F, Libonati R, de Lima TFM, Peixoto RB, de Almeida Franca JR, Magalhães MdAFM, Santos FLM, Rodrigues JA, DaCamara CC. Drought and fires influence the respiratory diseases hospitalizations in the Amazon. Ecol Ind. 2020;109:105817.
Leibel S, Nguyen M, Brick W, Parker J, Ilango S, Aguilera R, Gershunov A, Benmarhnia T. Increase in pediatric respiratory visits associated with santa ana wind-driven wildfire smoke and PM2.5 levels in San Diego County. Ann Am Thorac Soc. 2020;17:313–20.
Requia WJ, Kill E, Papatheodorou S, Koutrakis P, Schwartz JD. Prenatal exposure to wildfire-related air pollution and birth defects in Brazil. J Expo Sci Environ Epidemiol. 2022;32:596–603.
Requia WJ, Papatheodorou S, Koutrakis P, Mukherjee R, Roig HL. Increased preterm birth following maternal wildfire smoke exposure in Brazil. Int J Hyg Environ Health. 2022;240: 113901.
Johnston FH, Purdie S, Jalaludin B, Martin KL, Henderson SB, Morgan GG. Air pollution events from forest fires and emergency department attendances in Sydney, Australia 1996–2007: a case-crossover analysis. Environ Health. 2014;13:1–9.
Brew BK, Donnolley N, Henry A, Dahlen H, Jalaludin B, Chambers GM. Double jeopardy-pregnancy and birth during a catastrophic bushfire event followed by a pandemic lockdown, a natural experiment. Environ Res. 2022;214: 113752.
Requia WJ, Amini H, Adams MD, Schwartz JD. Birth weight following pregnancy wildfire smoke exposure in more than 1.5 million newborns in Brazil: a nationwide case-control study. Lancet Reg Health Am. 2022;11:100229.
Ciciretti R, Barraza F, De la Barrera F, Urquieta L, Cortes S. Relationship between wildfire smoke and children’s respiratory health in the metropolitan cities of Central-Chile. Atmosphere. 2022;13:58.
Doubleday A, Schulte J, Sheppard L, Kadlec M, Dhammapala R, Fox J, Busch Isaksen T. Mortality associated with wildfire smoke exposure in Washington state, 2006–2017: a case-crossover study. Environ Health. 2020;19:4.
Sahani M, Zainon NA, Mahiyuddin WRW, Latif MT, Hod R, Khan MF, Tahir NM, Chan C-C. A case-crossover analysis of forest fire haze events and mortality in Malaysia. Atmos Environ. 2014;96:257–65.
Sastry N. Forest fires, air pollution, and mortality in southeast Asia. Demography. 2002;39:1–23.
Vicedo-Cabrera AM, Esplugues A, Iniguez C, Estarlich M, Ballester F. Health effects of the 2012 Valencia (Spain) wildfires on children in a cohort study. Environ Geochem Health. 2016;38:703–12.
Mirabelli MC, Kunzli N, Avol E, Gilliland FD, Gauderman WJ, McConnell R, Peters JM. Respiratory symptoms following wildfire smoke exposure: airway size as a susceptibility factor. Epidemiology. 2009;20:451–9.
Rosales-Rueda M, Triyana M. The persistent effects of early-life exposure to air pollution evidence from the indonesian forest fires. J Human Resour. 2019;54:1037–80.
Jayachandran S. Air quality and early-life mortality evidence from Indonesia’s wildfires. J Human Resour. 2009;44:916–54.
Marsh BJ, Kolodzie K, Robinowitz D, Jacobson A, Ferschl M. Wildfire smoke exposure is associated with adverse respiratory events under general anesthesia in at-risk pediatric patients. Anesthesiology. 2022.
Del Pozo Cruz B, Hartwig TB, Sanders T, Noetel M, Parker P, Antczak D, Lee J, Lubans DR, Bauman A, Cerin E, Lonsdale C. The effects of the Australian bushfires on physical activity in children. Environ Int. 2021;146:106214.
Phung VLH, Ueda K, Sahani M, Seposo XT, Wan Mahiyuddin WR, Honda A, Takano H. Investigation of association between smoke haze and under-five mortality in Malaysia, accounting for time lag, duration and intensity. Int J Epidemiol. 2022;51:155–65.
Heft-Neal S, Driscoll A, Yang W, Shaw G, Burke M. Associations between wildfire smoke exposure during pregnancy and risk of preterm birth in California. Environ Res. 2022;203: 111872.
Campanharo WA, Morello T, Christofoletti MA, Anderson LO. Hospitalization due to fire-induced pollution in the Brazilian Legal Amazon from 2005 to 2018. Remote Sens. 2021;14:69.
Ignotti E, Valente JG, Longo KM, Freitas SR, de Souza Hacon S, Netto PA. Impact on human health of particulate matter emitted from burnings in the Brazilian Amazon region. Rev Saude Publica. 2010;44:121–30.
Pratt JR, Gan RW, Ford B, Brey S, Pierce JR, Fischer EV, Magzamen S. A national burden assessment of estimated pediatric asthma emergency department visits that may be attributed to elevated ozone levels associated with the presence of smoke. Environ Monit Assess. 2019;191:269.
Fadadu RP, Grimes B, Jewell NP, Vargo J, Young AT, Abuabara K, Balmes JR, Wei ML. Association of wildfire air pollution and health care use for atopic dermatitis and itch. JAMA Dermatol. 2021;157:658–66.
Johnston FH, Purdie S, Jalaludin B, Martin KL, Henderson SB, Morgan GG. Air pollution events from forest fires and emergency department attendances in Sydney, Australia 1996–2007: a case-crossover analysis. Environ Health. 2014;13:105.
Hahn M, Kuiper G, O'Dell K, Fischer E, Magzamen S. Wildfire smoke is associated with an increased risk of cardiorespiratory emergency department visits in Alaska. GeoHealth. 2021;5:e2020GH000349.
Zhang Y, Ye T, Yu P, Xu R, Chen G, Yu W, Song J, Guo Y, Li S. Preterm birth and term low birth weight associated with wildfire-specific PM2.5: a cohort study in New South Wales, Australia during 2016–2019. Environ Int. 2023:107879.
Abdo M, Ward I, O’Dell K, Ford B, Pierce JR, Fischer EV, Crooks JL. Impact of wildfire smoke on adverse pregnancy outcomes in Colorado, 2007–2015. Int J Environ Res Public Health. 2019;16:3720.
Liu RA, Wei Y, Qiu X, Kosheleva A, Schwartz JD. Short term exposure to air pollution and mortality in the US: a double negative control analysis. Environ Health. 2022;21:1–12.
Bloetzer C, Bovet P, Suris J-C, Simeoni U, Paradis G, Chiolero A. Screening for cardiovascular disease risk factors beginning in childhood. Public Health Rev. 2015;36:9.
Doubleday A, Schulte J, Sheppard L, Kadlec M, Dhammapala R, Fox J, Busch Isaksen T. Mortality associated with wildfire smoke exposure in Washington state, 2006–2017: a case-crossover study. Environ Health. 2020;19:1–10.
Morgan G, Sheppeard V, Khalaj B, Ayyar A, Lincoln D, Jalaludin B, Beard J, Corbett S, Lumley T. Effects of bushfire smoke on daily mortality and hospital admissions in Sydney, Australia. Epidemiology (Cambridge, Mass). 2010;21:47–55.
Acknowledgements
The editors would like to thank Ruth Etzel for handling the review of this manuscript.
Funding
TY and WH are supported by China Scholarship Council funds (TY: 201906320051; WH: 202006380055). RX is supported by Monash Faculty of Medicine Nursing and Health Science (FMNHS) Bridging Postdoctoral Fellowships 2022 and VicHealth Postdoctoral Research Fellowships 2022. YG is supported by Career Development Fellowship (GNT1163693) and Leader Fellowship (GNT2008813) of the Australian National Health and Medical Research Council. SL is supported by an Emerging Leader Fellowship (GNT2009866) of the Australian National Health and Medical Research Council. This study is supported by Australian Research Council (DP210102076), and Australian National Health & Medical Research Council (APP2000581). YZ is supported by NHMRC e-Asia Joint Research Program Grant (GNT2000581).
Author information
Authors and Affiliations
Contributions
S.L. and Y.G. developed the review premise. Y.Z. and T.Y. reviewed all identified abstracts and reviewed all identified articles in consultation with S.L. and Y.G.. Y.Z. and T.Y. completed the data extraction. Y.Z. and T.Y. appraised the study quality of included articles and checked. Y.Z. performed the meta-analysis. YZ prepared the figures and tables and draft the manuscript. T.Y., W.H., P.Y., G.C., R.X., J.S., Y.G. and S.L. contributed to the reviewing and editing of the paper. All authors approved the final version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Y., Tingting, Y., Huang, W. et al. Health Impacts of Wildfire Smoke on Children and Adolescents: A Systematic Review and Meta-analysis. Curr Envir Health Rpt 11, 46–60 (2024). https://doi.org/10.1007/s40572-023-00420-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-023-00420-9