Abstract
Background
Studies have shown that Black patients are more likely to experience complications following breast reconstruction compared to other racial groups. Most of these studies have been conducted on patient populations focusing on either autologous or implant-based reconstruction without possible predictive indicators for complication disparities for all types of reconstruction procedures. The aim of this study is to elucidate disparities among patient demographics by identifying predictors of complications and postoperative outcomes among different racial/ethnic patients undergoing breast reconstruction utilizing multi-state, multi-institution, and national level data.
Methods
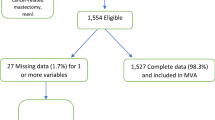
Patients in the Optum Clinformatics Data Mart that underwent all billable forms of breast reconstruction were identified via CPT codes. Demographics, medical history, and postoperative outcome data were collected by querying relevant reports of CPT, ICD-9, and ICD-10 codes. Outcomes analysis was limited to the 90-day global postoperative period. A multivariable logistic-regression analysis was performed to ascertain the effects of age, patient reported ethnicity, coexisting conditions, and reconstruction type on the likelihood of any common postoperative complication occurring. Linearity of the continuous variables with respect to the logit of the dependent variable was confirmed. Odds ratios and corresponding 95% confidence intervals were calculated.
Results
From over 86 million longitudinal patient records, our study population included 104,714 encounters for 57,468 patients who had undergone breast reconstruction between January 2003 and June 2019. Black race (relative to White), autologous reconstruction, hypertension, type II diabetes mellitus, and tobacco use were independent predictors of increased likelihood of complication. Specifically, the odds ratios for complication occurrence for Black, Hispanic, and Asian ethnicity (relative to White) were 1.09, 1.03, and 0.77, respectively. Black patients had an overall breast reconstruction complication rate of 20.4%, while the corresponding rate for White, Hispanic, and Asian patients were 17.0%, 17.9%, and 13.2%, respectively.
Conclusion
Our analysis of a national-level database shows that Black patients undergoing implant-based or autologous reconstruction have increased risk of complications, likely due to multifactorial components that play a role in the care of this patient population. While higher rates of comorbidities have been cited as a possible cause, providers must consider racial influences involving cultural context, historical mistrust in medicine, and physician/health institution factors that may drive this disparity of outcomes among our patients.

Similar content being viewed by others
Data Availability
Data/materials are not available publicly, but can be shared if requested and permitted by Stanford PHI Offices.
Code Availability
Code is not available publicly but can be shared if requested and approved by Stanford PHI offices.
References
Rahib L, Wehner MR, Matrisian LM, Nead KT. Estimated projection of US cancer incidence and death to 2040. JAMA Netw Open. 2021;4(4):e214708. https://doi.org/10.1001/jamanetworkopen.2021.4708.
Howes BH, Watson DI, Xu C, Fosh B, Canepa M, Dean NR. Quality of life following total mastectomy with and without reconstruction versus breast-conserving surgery for breast cancer: a case-controlled cohort study. J Plast Reconstr Aesthet Surg. 2016;69(9):1184–91. https://doi.org/10.1016/j.bjps.2016.06.004.
Sisco M, Du H, Warner JP, Howard MA, Winchester DP, Yao K. Have we expanded the equitable delivery of postmastectomy breast reconstruction in the new millennium? Evidence from the national cancer data base. J Am Coll Surg. 2012;215(5):658–66. https://doi.org/10.1016/j.jamcollsurg.2012.07.008.
Blankensteijn LL, Sparenberg S, Crystal DT, Ibrahim AMS, Lee BT, Lin SJ. Racial disparities in outcomes of reconstructive breast surgery: an analysis of 51,362 patients from the ACS-NSQIP. J Reconstr Microsurg. 2020;36(8):592–9. https://doi.org/10.1055/s-0040-1713174.
Mets EJ, Chouairi FK, Gabrick KS, Avraham T, Alperovich M. Persistent disparities in breast cancer surgical outcomes among hispanic and African American patients. Eur J Surg Oncol. 2019;45(4):584–90. https://doi.org/10.1016/j.ejso.2019.01.016.
Butler PD, Morris MP, Momoh AO. Persistent disparities in postmastectomy breast reconstruction and strategies for mitigation. Ann Surg Oncol. 2021;28(11):6099–108. https://doi.org/10.1245/s10434-021-10487-z.
Sarver MM, Rames JD, Ren Y, et al. Racial and ethnic disparities in surgical outcomes after postmastectomy breast reconstruction. J Am Coll Surg. 2022;234(5):760–71. https://doi.org/10.1097/XCS.0000000000000143.
Kamali P, Zettervall SL, Wu W, et al. Differences in the reporting of racial and socioeconomic disparities among three large national databases for breast reconstruction. Plast Reconstr Surg. 2017;139(4):795–807. https://doi.org/10.1097/PRS.0000000000003207.
Grippaudo FR, Renzi L, Costantino B, Longo B, Santanelli F. Late unilateral hematoma after breast reconstruction with implants: case report and literature review. Aesthet Surg J. 2013;33(6):830–4. https://doi.org/10.1177/1090820X13496249.
Thorarinsson A, Fröjd V, Kölby L, Lidén M, Elander A, Mark H. Patient determinants as independent risk factors for postoperative complications of breast reconstruction. Gland Surg. 2017;6(4):355–67. https://doi.org/10.21037/gs.2017.04.04.
Marinescu SA, Bejinariu CG, Şapte E, Marinaş MC, Giuglea C. Complications related to breast reconstruction after mastectomy using multiple surgical techniques - a national and international comparative analysis. Rom J Morphol Embryol. 2019;60(1):87–93.
Major M, Devulapalli C, Bello RJ, et al. The effect of timing on breast reconstruction outcomes in diabetic women. Plast Reconstr Surg Glob Open. 2016;4(10):e1090. https://doi.org/10.1097/GOX.0000000000001090. (Published 2016 Oct 25).
Martin MS, Kebede S, Saad OA, Baker NF, Losken A. Impact of socioeconomic status on breast reconstruction outcomes. Ann Plast Surg. 2022;88(5 Suppl 5):S481–4. https://doi.org/10.1097/SAP.0000000000003124.
Butler PD, Nelson JA, Fischer JP, et al. African-American women have equivalent outcomes following autologous free flap breast reconstruction despite greater preoperative risk factors. Am J Surg. 2015;209(4):589–96. https://doi.org/10.1016/j.amjsurg.2014.11.002.
Berlin NL, Momoh AO, Qi J, et al. Racial and ethnic variations in one-year clinical and patient-reported outcomes following breast reconstruction. Am J Surg. 2017;214(2):312–7. https://doi.org/10.1016/j.amjsurg.2017.02.009.
Butler PD, Nelson JA, Fischer JP, et al. Racial and age disparities persist in immediate breast reconstruction: an updated analysis of 48,564 patients from the 2005 to 2011 American College of Surgeons National Surgery Quality Improvement Program data sets. Am J Surg. 2016;212(1):96–101. https://doi.org/10.1016/j.amjsurg.2015.08.025.
Oskar S, Nelson JA, Hicks MEV, et al. The impact of race on perioperative and patient-reported outcomes following autologous breast reconstruction. Plast Reconstr Surg. 2022;149(1):15–27. https://doi.org/10.1097/PRS.0000000000008633.
Tseng JF, Kronowitz SJ, Sun CC, et al. The effect of ethnicity on immediate reconstruction rates after mastectomy for breast cancer. Cancer. 2004;101(7):1514–23. https://doi.org/10.1002/cncr.20529.
Rubin LR, Chavez J, Alderman A, Pusic AL. “Use what God has given me”: difference and disparity in breast reconstruction. Psychol Health. 2013;28(10):1099–120. https://doi.org/10.1080/08870446.2013.782404.
von Glinski M, Holler N, Kümmel S, et al. Autologous vs. implant-based breast reconstruction after skin- and nipple-sparing mastectomy-a deeper insight considering surgical and patient-reported outcomes. Front Surg. 2022;9:903734. https://doi.org/10.3389/fsurg.2022.903734. (Published 2022 Sep 5).
Pedreira R, Tevlin R, Griffin M, Wan D, Momeni A. Investigating the severity of complications following mastectomy and prepectoral implant-based versus autologous reconstruction. Plast Reconstr Surg. 2023;151(2):200e-206e. https://doi.org/10.1097/PRS.0000000000009827
Wang HY, Ali RS, Chen SC, Chao TC, Cheng MH. One-stage immediate breast reconstruction with implant following skin-sparing mastectomy in Asian patients. Ann Plast Surg. 2008;60(4):362–6. https://doi.org/10.1097/SAP.0b013e318063ef70.
Connors SK, Goodman MS, Myckatyn T, Margenthaler J, Gehlert S. Racial disparities in breast reconstruction at a comprehensive cancer center. J Racial Ethn Health Disparities. 2022;9(6):2323–33. https://doi.org/10.1007/s40615-021-01169-3.
Offodile AC 2nd, Tsai TC, Wenger JB, Guo L. Racial disparities in the type of postmastectomy reconstruction chosen. J Surg Res. 2015;195(1):368–76. https://doi.org/10.1016/j.jss.2015.01.013.
Bickell NA, Wang JJ, Oluwole S, et al. Missed opportunities: racial disparities in adjuvant breast cancer treatment. J Clin Oncol. 2006;24(9):1357–62. https://doi.org/10.1200/JCO.2005.04.5799.
Wilkins EG, Alderman AK. Breast reconstruction practices in North America: current trends and future priorities. Semin Plast Surg. 2004;18(2):149–55. https://doi.org/10.1055/s-2004-829049.
American Cancer Society. Women’s Health and Cancer Rights Act. 2019. Accessed 17 Apr 2023. https://www.cancer.org/womens-health-and-cancer-rights-act.html
Center for Medicaid and Medicare Services. Women’s Health and Cancer Rights Act (WHCRA). CMS. 2022. Accessed 17 Apr 2023. https://www.cms.gov/CCIIO/Programs-and-Initiatives/Other-Insurance-Protections/whcra_factsheet.
Shippee TP, Kozhimannil KB, Rowan K, Virnig BA. Health insurance coverage and racial disparities in breast reconstruction after mastectomy. Womens Health Issues. 2014;24(3):e261–9. https://doi.org/10.1016/j.whi.2014.03.001.
Dehal A, Abbas A, Johna S. Racial disparities in clinical presentation, surgical treatment and in-hospital outcomes of women with breast cancer: analysis of nationwide inpatient sample database. Breast Cancer Res Treat. 2013;139(2):561–9. https://doi.org/10.1007/s10549-013-2567-1.
Ashing K, Rosales M, Lai L, Hurria A. Occurrence of comorbidities among African-American and Latina breast cancer survivors. J Cancer Surviv. 2014;8(2):312–8. https://doi.org/10.1007/s11764-014-0342-x.
Lee KT, Hong SH, Jeon BJ, Pyon JK, Mun GH, Bang SI. Predictors for prolonged drainage following tissue expander-based breast reconstruction. Plast Reconstr Surg. 2019;144(1):9e–17e. https://doi.org/10.1097/PRS.0000000000005697.
Alderman AK, Wilkins EG, Kim HM, Lowery JC. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2002;109(7):2265–74. https://doi.org/10.1097/00006534-200206000-00015.
Selber JC, Kurichi JE, Vega SJ, Sonnad SS, Serletti JM. Risk factors and complications in free TRAM flap breast reconstruction. Ann Plast Surg. 2006;56(5):492–7. https://doi.org/10.1097/01.sap.0000210180.72721.4a.
Gill PS, Hunt JP, Guerra AB, et al. A 10-year retrospective review of 758 DIEP flaps for breast reconstruction. Plast Reconstr Surg. 2004;113(4):1153–60. https://doi.org/10.1097/01.prs.0000110328.47206.50.
Fischer JP, Nelson JA, Serletti JM, Wu LC. Peri-operative risk factors associated with early tissue expander (TE) loss following immediate breast reconstruction (IBR): a review of 9305 patients from the 2005–2010 ACS-NSQIP datasets. J Plast Reconstr Aesthet Surg. 2013;66(11):1504–12. https://doi.org/10.1016/j.bjps.2013.06.030.
Spira JAO, Borges EL, Silva PAB, Abreu MNS, Guedes ACM, Pires-Júnior JF. Factors associated with complex surgical wounds in breast and abdomen: a case-control observational study. Rev Lat Am Enfermagem. 2018;26:e3052. https://doi.org/10.1590/1518-8345.2274.3052.
Markides KS, Coreil J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep. 1986;101(3):253–65.
Azin A, Tahmasebi H, Brar A, et al. Racial, ethnic and socioeconomic disparities in diagnosis, treatment, and survival of patients with breast cancer. Am J Surg. 2023;225(1):154–61. https://doi.org/10.1016/j.amjsurg.2022.07.003.
Turra CM, Elo IT. The impact of salmon bias on the hispanic mortality advantage: new evidence from social security data. Popul Res Policy Rev. 2008;27(5):515–30. https://doi.org/10.1007/s11113-008-9087-4.
Warner ET, Tamimi RM, Hughes ME, et al. Racial and ethnic differences in breast cancer survival: mediating effect of tumor characteristics and sociodemographic and treatment factors. J Clin Oncol. 2015;33(20):2254–61. https://doi.org/10.1200/JCO.2014.57.1349.
Amey CH, Miller MK, Albrecht SL. The role of race and residence in determining stage at diagnosis of breast cancer. J Rural Health. 1997;13(2):99–108. https://doi.org/10.1111/j.1748-0361.1997.tb00939.x.
Bennett KG, Qi J, Kim HM, Hamill JB, Pusic AL, Wilkins EG. Comparison of 2-year complication rates among common techniques for postmastectomy breast reconstruction. JAMA Surg. 2018;153(10):901–8. https://doi.org/10.1001/jamasurg.2018.1687.
Siotos C, Azizi A, Assam L, et al. Breast reconstruction for medicaid beneficiaries: a systematic review of the current evidence. J Plast Surg Hand Surg. 2020;54(2):77–82. https://doi.org/10.1080/2000656X.2019.1688167.
Goldenberg AR, Willcox LM, Abolghasemi DM, et al. Did Medicaid expansion mitigate disparities in post-mastectomy reconstruction rates? Am Surg. 2022;88(5):846–51. https://doi.org/10.1177/00031348211060452.
Offodile AC 2nd, Muldoon LD, Gani F, Canner JK, Jacobs LK. The site of care matters: an examination of the relationship between high Medicaid burden hospitals and the use, cost, and complications of immediate breast reconstruction after mastectomy. Cancer. 2018;124(2):346–55. https://doi.org/10.1002/cncr.31046.
Vieira BL, Lanier ST, Mlodinow AS, et al. A multi-institutional analysis of insurance status as a predictor of morbidity following breast reconstruction. Plast Reconstr Surg Glob Open. 2014;2(11):e255. https://doi.org/10.1097/GOX.0000000000000207.
Aggarwal R, Gondi S, Wadhera RK. Comparison of Medicare advantage vs traditional medicare for health care access, affordability, and use of preventive services among adults with low income. JAMA Netw Open. 2022;5(6):e2215227. https://doi.org/10.1001/jamanetworkopen.2022.15227.
Ochieng N, Biniek JF. Beneficiary experience, affordability, utilization, and quality in medicare advantage and traditional medicare: a review of the literature. Kaiser Family Foundation. Published Sep 16, 2022. Accessed Apr 2023. https://www.kff.org/medicare/report/beneficiary-experience-affordability-utilization-and-quality-in-medicare-advantage-and-traditional-medicare-a-review-of-the-literature/view/report/
Acknowledgements
Data for this project were accessed using the Stanford Center for Population Health Sciences Data Core. The PHS Data Core is supported by a National Institutes of Health National Center for Advancing Translational Science Clinical and Translational Science Award (UL1 TR001085) and from internal Stanford funding. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
KT and TJ are lead authors, project management, idea formation, editing, analysis, and writing. MR, SF, JC, DS, and YN helped with manuscript writing, paper direction, and editing. JS assisted with more data analysis and study formation. RN is the corresponding author, and PI is the mentor of the projects.
Corresponding author
Ethics declarations
Ethics Approval
N/A.
Consent to Participate
N/A.
Consent for Publication
N/A.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
CPT codes used to identify patients in the Clinformatics® Database undergoing breast reconstruction, fat grafting, and complications requiring surgical intervention
Procedure | CPT |
|---|---|
Implant-based breast reconstruction | 19,357, 11,970, 19,340, 19,342 |
Autologous breast reconstruction | 19,361, 19,364, 19,367, 19,368, 19,369 |
Fat grafting | 15,771, 15,772, 15,769, 20,926 |
Incision and drainage, deep abscess or hematoma, soft tissues of neck, or rhorax | 21,501 |
Image-guided fluid collection drainage by catheter (e.g., abscess, hematoma, seroma, lymphoma, and cyst) | 10,030 |
Incision and drainage of hematoma, seroma, or fluid collection | 10,140 |
Incision drainage of complex wound infection | 10,180 |
Secondary closure of surgical wound or dehiscence | 13,160 |
Tissue debridement | 11,042, 11,045 |
Muscle debridement | 11,043 |
Bone debridement | 11,044 |
Appendix 2
ICD-9 and ICD-10 codes used to identify patients in the Clinformatics® Database experiencing complications as a result of the index procedure
Diagnosis | ICD-9 | ICD-10 |
|---|---|---|
Hematoma or hemorrhage | 99,812 | M7981, R58, T792XXD, T792XXXS, T792XXA, L7602, L7622 |
Seroma | 99,813 | L7634, M7098, T792XXD, T792XXS, T792XXA |
Deep vein thrombosis (DVT) or other vascular complication | 4510, 4511, 45,111, 45,119, 4512, 45,181, 45,189, 4519, 4531, 4532, 4534, 45,341, 45,342, 45,350, 45,351, 45,352, 4536, 4538, 45,389, 4539, 99,779, 9972 | T81718D, T81718S, T81718A, T8172XD, T8172XS, T8172XA I80201, I80202, I80203, I80221, I80222, I80223, I80229, I80231, I80232 I80233, I80239, I80241, I80242, I80243, I80251, I80252, I80253, I80291 I80292, I80293, I80299, I80209, I80249, I80259, I808, I82401, I82402 I82403, I82409, I82431, I82432, I82433, I824Y1, I824Y2, I824Y3, I82439 I824Y9, I82441, I82442, I82443, I82451, I82452, I82453, I82461, I82462 I82463, I82491, I82492, I82493, I824Z1, I824Z2, I824Z3, I82449, I82459 I82469, I82499, I824Z9, I8010, I8011, I8012, I8013, I82411, I82412 I82413, I82419, I80211, I80212, I80213, I80219, I82421, I82422, I82423 I82429, I82621, I82622, I82A11, I82A12, I82A13, I82A19, I82B11, I82B12 I82B13, I82B19, I82C11, I82C12, I82C13, I82C19 |
Breast reconstruction deformity and wound dehiscence | 8750, 8751, 8790, 8791, 9983, 99832x | T8130XD, T8130XS, T8130XA, T8132XD, T8132XS, T8132XA, T8131XD, T8131XS T8131XA, T8183XD, T8183XS, T8183XA, T8189XD, T8189XS, T8189XA, T8133A, T8133D, T8133S, S21002A, S21001A |
Postoperative infection | 9985, 99,850–99,859 | T8140XA, T8140XD, T8140XS, T8141XA, T8141XD, T8141XS, T8142XA, T8142XD, T8142XS, T8143XA, T8143XD, T8143XS, T8144XA, T8144XD, T8144XS, T8149XA, T8149XD, T8149XS, N611, T86822 |
Fat necrosis | 6113, 56,782 | N641, K654 |
Tissue necrosis | 99,883 | T8189XA |
Nonspecified complication of surgical care | 61,189 | T888XXD, T888XXS, T888XXA, N6489 |
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Johnstone, T., Thawanyarat, K., Rowley, M. et al. Racial Disparities in Postoperative Breast Reconstruction Outcomes: A National Analysis. J. Racial and Ethnic Health Disparities 11, 1199–1210 (2024). https://doi.org/10.1007/s40615-023-01599-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-023-01599-1