Key summary points
To investigate potential relationships between orthostatic hypotension (OH) and negative health outcomes and mortality, through an umbrella review with integrated meta-analyses.
AbstractSection FindingsOrthostatic hypotension is significantly associated with several negative outcomes in older people, but a suggestive evidence is available only for higher risk of coronary heart disease congestive heart failure, stroke, falls dementia, and all-cause mortality.
AbstractSection MessageOrthostatic hypotension seems to be significantly associated with several negative health outcomes in older people, even if only associations with coronary heart disease, congestive heart failure, stroke, falls, dementia, and all-cause mortality are supported by suggestive evidence.
Abstract
Purpose
Orthostatic hypotension (OH) is associated with older age and many negative clinical outcomes in geriatric practice. We aimed to capture the breadth of outcomes that have been associated with the presence of OH and systematically assess the quality, strength and credibility of these associations using an umbrella review with integrated meta-analyses.
Methods
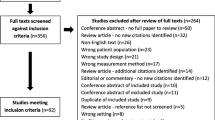
We systematically searched several major databases from their commencements through to 16th May 2019 for meta-analyses of observational studies of OH and any health-related outcome. We used these metrics to categorize the strength of evidence of significant outcomes (p < 0.05) from class I (convincing) to class IV (weak), according to the pre-established criteria.
Results
From 975 abstracts, seven meta-analyses of 12 outcomes were included. For each outcome, the median number of studies was four, and the median number of participants was 46,493, with a median of 3630 incident cases. There was suggestive (class III) evidence that OH was associated with significantly higher risk of coronary heart disease (HR = 1.32, 95% CI 1.12–1.56), stroke (HR = 1.22, 95% CI 1.08–1.38), congestive heart failure (HR = 1.30, 95% CI 1.09–1.55), all-cause mortality (RR = 1.50, 95% CI 1.24–1.81), falls (OR = 1.84, 95% CI 1.39–2.44), and dementia (HR = 1.22, 95% CI 1.11–1.35).
Conclusion
The current evidence base indicates that OH is significantly associated with a range of adverse cardiovascular, cognitive, and mortality outcomes in older people, although the strength of this evidence remains only suggestive. Further research in larger samples and with lower risk of bias is required to build a fuller picture of the impact of OH on health.

Similar content being viewed by others
References
American Autonomic Society, The American Academy of Neurology (1996) Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. The Consensus Committee of the American Autonomic Society and the American Academy of Neurology. Neurology 46:1470
Low PA (2008) Prevalence of orthostatic hypotension. Clin Auton Res 18:8–13
Soysal P, Aydin AE, Okudur SK, Isik AT (2016) When should orthostatic blood pressure changes be evaluated in elderly: 1st, 3rd or 5th minute? Arch Gerontol Geriatr 65:199–203
Aydin AE, Soysal P, Isik AT (2017) Which is preferable for orthostatic hypotension diagnosis in older adults: active standing test or head-up tilt table test? Clin Interv Aging 12:207
Low PA, Tomalia VA (2015) Orthostatic hypotension: mechanisms, causes, management. J Clin Neurol 11:220–226
Verwoert GC, Mattace-Raso FU, Hofman A, Heeringa J, Stricker BH, Breteler MM, Witteman JC (2008) Orthostatic hypotension and risk of cardiovascular disease in elderly people: the Rotterdam study. J Am Geriatr Soc 56:1816–1820
Atkins D, Hanusa B, Sefcik T, Kapoor W (1991) Syncope and orthostatic hypotension. Am J Med 91:179–185
Yap PLK, Niti M, Yap KB, Ng TP (2008) Orthostatic hypotension, hypotension and cognitive status: early comorbid markers of primary dementia? Dement Geriatr Cogn Disord 26:239
Gupta V, Lipsitz LA (2007) Orthostatic hypotension in the elderly: diagnosis and treatment. Am J Med 120:841–847
Schneider L, Sloane RB, Staples FR, Bender M (1986) Pretreatment orthostatic hypotension as a predictor of response to nortriptyline in geriatric depression. J Clin Psychopharmacol 6:172–176
Chen L, Xu Y, Chen X, Lee W-J, Chen L-K (2019) Association between orthostatic hypotension and frailty in hospitalized older patients: a geriatric syndrome more than a cardiovascular condition. J Nutr Health Aging 23:318–322
Ioannidis JP (2009) Integration of evidence from multiple meta-analyses: a primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. CMAJ 181:488–493
Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, Davies P, Kleijnen J, Churchill R (2016) ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol 69:225–234
Avelino-Silva TJ, Jaluul O (2017) Malnutrition in hospitalized older patients: management strategies to improve patient care and clinical outcomes. Int J Gerontol 11:56–61
Stroud M, Duncan H, Nightingale J (2003) Guidelines for enteral feeding in adult hospital patients. Gut 52:vii1
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Veronese N, Notarnicola M, Osella A et al (2018) Menopause does not affect fatty liver severity in women: a population study in a Mediterranean area. Endocr Metabol Immune Disord Drug Targets 18(5):513–521. https://doi.org/10.2174/1871530318666180423101755
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Carvalho AF, Kohler CA, Brunoni AR, Miskowiak KW, Herrmann N, Lanctot KL, Hyphantis TN, Quevedo J, Fernandes BS, Berk M (2016) Bias in peripheral depression biomarkers. Psychother Psychosom 85:81–90
Ioannidis JP, Trikalinos TA (2007) An exploratory test for an excess of significant findings. Clin Trials 4:245–253
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P (2015) Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Health Care 13:132–140
Belbasis L, Savvidou MD, Kanu C, Evangelou E, Tzoulaki I (2016) Birth weight in relation to health and disease in later life: an umbrella review of systematic reviews and meta-analyses. BMC Med 14:147
Bellou V, Belbasis L, Tzoulaki I, Evangelou E, Ioannidis JP (2016) Environmental risk factors and Parkinson’s disease: an umbrella review of meta-analyses. Parkinsonism Relat Disord 23:1–9
Dinu M, Pagliai G, Casini A, Sofi F (2017) Mediterranean diet and multiple health outcomes: an umbrella review of meta-analyses of observational studies and randomized trials. Nutr Metabol Cardiovasc Dis 27:e21
Kyrgiou M, Kalliala I, Markozannes G, Gunter MJ, Paraskevaidis E, Gabra H, Martin-Hirsch P, Tsilidis KK (2017) Adiposity and cancer at major anatomical sites: umbrella review of the literature. BMJ 356:j477
Li X, Meng X, Timofeeva M, Tzoulaki I, Tsilidis KK, Ioannidis PA, Campbell H, Theodoratou E (2017) Serum uric acid levels and multiple health outcomes: umbrella review of evidence from observational studies, randomised controlled trials, and Mendelian randomisation studies. BMJ 357:j2376
Theodoratou E, Tzoulaki I, Zgaga L, Ioannidis JPA (2014) Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomised trials. BMJ 348:g2035
Veronese N, Solmi M, Caruso MG, Giannelli G, Osella AR, Evangelou E, Maggi S, Fontana L, Stubbs B, Tzoulaki I (2018) Dietary fiber and health outcomes: an umbrella review of systematic reviews and meta-analyses. Am J Clin Nutr 107:436–444
Machado MO, Veronese N, Sanches M et al (2018) The association of depression and all-cause and cause-specific mortality: an umbrella review of systematic reviews and meta-analyses. BMC Med 16:112
Veronese N, Demurtas J, Celotto S et al (2018) Is chocolate consumption associated with health outcomes? An umbrella review of systematic reviews and meta-analyses. Clin Nutr 38(3):1101–1108
Veronese N, Demurtas J, Pesolillo G et al (2019) Magnesium and health outcomes: an umbrella review of systematic reviews and meta-analyses of observational and intervention studies. Eur J Nutr. https://doi.org/10.1007/s00394-019-01905-w
Köhler CA, Evangelou E, Stubbs B et al (2018) Mapping risk factors for depression across the lifespan: an umbrella review of evidence from meta-analyses and Mendelian randomization studies. J Psychiatr Res 103:189–207
Smith L, Luchini C, Demurtas J et al (2019) Telomere length and health outcomes: an umbrella review of systematic reviews and meta-analyses of observational studies. Ageing Res Rev 51:1–10
Iseli R, Nguyen VTV, Sharmin S, Reijnierse EM, Lim WK, Maier AB (2019) Orthostatic hypotension and cognition in older adults: a systematic review and meta-analysis. Exp Gerontol 120:40–49
Min M, Shi T, Sun C, Liang M, Zhang Y, Wu Y, Sun Y (2018) The association between orthostatic hypotension and dementia: a meta-analysis of prospective cohort studies. Int J Geriatr Psychiatry 33:1541–1547
Mol A, Hoang PTSB, Sharmin S, Reijnierse EM, van Wezel RJ, Meskers CG, Maier AB (2018) Orthostatic hypotension and falls in older adults: a systematic review and meta-analysis. J Am Med Dir Assoc 20(5):589–597
Ricci F, Fedorowski A, Radico F, Romanello M, Tatasciore A, Di Nicola M, Zimarino M, De Caterina R (2015) Cardiovascular morbidity and mortality related to orthostatic hypotension: a meta-analysis of prospective observational studies. Eur Heart J 36:1609–1617
Xin W, Lin Z, Li X (2013) Orthostatic hypotension and the risk of congestive heart failure: a meta-analysis of prospective cohort studies. PLoS One 8:e63169
Xin W, Lin Z, Mi S (2014) Orthostatic hypotension and mortality risk: a meta-analysis of cohort studies. Heart 100:406–413
Xin W, Mi S, Lin Z, Wang H, Wei W (2016) Orthostatic hypotension and the risk of incidental cardiovascular diseases: a meta-analysis of prospective cohort studies. Prev Med 85:90–97
Smit AA, Halliwill JR, Low PA, Wieling W (1999) Pathophysiological basis of orthostatic hypotension in autonomic failure. J Physiol 519(Pt 1):1–10
Mattace-Raso FU, van der Cammen TJ, Knetsch AM, van den Meiracker AH, Schalekamp MA, Hofman A, Witteman JC (2006) Arterial stiffness as the candidate underlying mechanism for postural blood pressure changes and orthostatic hypotension in older adults: the Rotterdam study. J Hypertens 24:339–344
Fedorowski A, Ostling G, Persson M, Struck J, Engstrom G, Nilsson PM, Hedblad B, Melander O (2012) Orthostatic blood pressure response, carotid intima-media thickness, and plasma fibrinogen in older nondiabetic adults. J Hypertens 30:522–529
Fan XH, Wang Y, Sun K, Zhang W, Wang H, Wu H, Zhang H, Zhou X, Hui R (2010) Disorders of orthostatic blood pressure response are associated with cardiovascular disease and target organ damage in hypertensive patients. Am J Hypertens 23:829–837
Pepersack T, Gilles C, Petrovic M, Spinnewine A, Baeyens H, Beyer I, Boland B, Dalleur O, De Lepeleire J, Even-Adin D, Van Nes MC, Samalea-Suarez A, Somers A, Working Group Clinical Pharmacology, Pharmacotherapy and Pharmaceutical Care, Belgian Society for Gerontology and Geriatrics (2013) Prevalence of orthostatic hypotension and relationship with drug use amongst older patients. Acta Clin Belg 68:107–112
Mager DR (2012) Orthostatic hypotension: pathophysiology, problems, and prevention. Home Healthc Nurse 30:525–530
Aoki M, Tanaka K, Wakaoka T, Kuze B, Hayashi H, Mizuta K, Ito Y (2013) The association between impaired perception of verticality and cerebral white matter lesions in the elderly patients with orthostatic hypotension. J Vestib Res 23:85–93
Humm AM, Bostock H, Troller R, Z’Graggen WJ (2011) Muscle ischaemia in patients with orthostatic hypotension assessed by velocity recovery cycles. J Neurol Neurosurg Psychiatry 82:1394–1398
Chisholm P, Anpalahan M (2017) Orthostatic hypotension: pathophysiology, assessment, treatment and the paradox of supine hypertension. Intern Med J 47:370–379
Elmstahl S, Rosen I (1997) Postural hypotension and EEG variables predict cognitive decline: results from a 5-year follow-up of healthy elderly women. Dement Geriatr Cogn Disord 8:180–187
Toyry JP, Kuikka JT, Lansimies EA (1997) Regional cerebral perfusion in cardiovascular reflex syncope. Eur J Nucl Med 24:215–218
Brown WR, Thore CR (2011) Review: cerebral microvascular pathology in ageing and neurodegeneration. Neuropathol Appl Neurobiol 37:56–74
Liu H, Zhang J (2012) Cerebral hypoperfusion and cognitive impairment: the pathogenic role of vascular oxidative stress. Int J Neurosci 122:494–499
Foster-Dingley JC, Moonen JEF, de Ruijter W, van der Mast RC, van der Grond J (2018) Orthostatic hypotension in older persons is not associated with cognitive functioning, features of cerebral damage or cerebral blood flow. J Hypertens 36:1201–1206
Flachenecker P, Wolf A, Krauser M, Hartung H-P, Reiners K (1999) Cardiovascular autonomic dysfunction in multiple sclerosis: correlation with orthostatic intolerance. J Neurol 246:578–586
Lim SY, Lang AE (2010) The nonmotor symptoms of Parkinson’s disease: an overview. Mov Disord 25(Suppl 1):S123–S130
Gaspar L, Kruzliak P, Komornikova A et al (2016) Orthostatic hypotension in diabetic patients: 10-year follow-up study. J Diabetes Complicat 30:67–71
Isik AT, Kocyigit SE, Smith L, Aydin AE, Soysal P (2019) A comparison of the prevalence of orthostatic hypotension between older patients with Alzheimer’s disease, Lewy body dementia, and without dementia. Exp Gerontol 124:110628. https://doi.org/10.1016/j.exger.2019.06.001
Xin W, Lin Z, Mi S (2014) Orthostatic hypotension and mortality risk: a meta-analysis of cohort studies. Heart 100:406–413
Robertson D (2008) The pathophysiology and diagnosis of orthostatic hypotension. Clin Auton Res 18(Suppl 1):2–7
Sabbah HN (2012) Baroreflex activation for the treatment of heart failure. Curr Cardiol Rep 14:326–333
Schwartz PJ, La Rovere MT (1998) ATRAMI: a mark in the quest for the prognostic value of autonomic markers. Autonomic tone and reflexes after myocardial infarction. Eur Heart J 19:1593–1595
La Rovere MT, Bigger JT Jr, Marcus FI, Mortara A, Schwartz PJ (1998) Baroreflex sensitivity and heart-rate variability in prediction of total cardiac mortality after myocardial infarction. ATRAMI (autonomic tone and reflexes after myocardial infarction) investigators. Lancet 351:478–484
Ioannidis JP (2016) The mass production of redundant, misleading, and conflicted systematic reviews and meta-analyses. Milbank Q 94:485–514
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
It was not requested being a revision of already published literature. This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
No patients were included in this review.
Sponsor’s role
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Soysal, P., Veronese, N., Smith, L. et al. Orthostatic hypotension and health outcomes: an umbrella review of observational studies. Eur Geriatr Med 10, 863–870 (2019). https://doi.org/10.1007/s41999-019-00239-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-019-00239-4