Abstract
Background
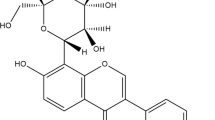
Hexahydrocurcumin (HHC), a major metabolite of curcumin, has been reported to have protective effects against ischemic and reperfusion damage. The goal of the present research was to examine whether HHC could alleviate brain damage and ameliorate functional outcomes by diminishing the blood–brain barrier (BBB) damage that follows cerebral ischemia/reperfusion.
Methods
Middle cerebral artery occlusion was induced for 2 h in rats followed by reperfusion. The rats were divided into three groups: sham-operated, vehicle-treated, and HHC-treated groups. At the onset of reperfusion, the rats were immediately intraperitoneally injected with 40 mg/kg HHC. At 48 h after reperfusion, the rats were evaluated for neurological deficits and TTC staining. At 24 h and 48 h after reperfusion, animals were sacrificed, and their brains were extracted.
Results
Treatment with HHC reduced neurological scores, infarct volume, morphological changes, Evans blue leakage and immunoglobulin G extravasation. Moreover, HHC treatment reduced BBB damage and neutrophil infiltration, downregulated myeloperoxidase, ICAM-1, and VCAM-1, upregulated tight junction proteins (TJPs), and reduced aquaporin 4 expression and brain water content.
Conclusion
These results revealed that HHC treatment preserved the BBB from cerebral ischemia/reperfusion injury by regulating TJPs, attenuating neutrophil infiltration, and reducing brain edema formation.
Graphic abstract








Similar content being viewed by others
Abbreviations
- AQP4:
-
Aquaporin 4
- AS:
-
Astrocytic swelling
- BBB:
-
Blood–brain barrier
- BM:
-
Basement membrane
- BSA:
-
Bovine serum albumin
- CBF:
-
Cerebral blood flow
- CCA:
-
Common carotid artery
- CNS:
-
Central nervous system
- COX-2:
-
Cyclooxygenase-2
- EB:
-
Evans blue
- ECA:
-
External carotid artery
- ECM:
-
Extracellular matrix
- GI:
-
Gastrointestinal
- H&E:
-
Hematoxylin and eosin
- HHC:
-
Hexahydrocurcumin
- HRP:
-
Horseradish peroxidase
- I/R:
-
Ischemia reperfusion
- ICA:
-
Internal carotid artery
- IgG:
-
Immunoglobulin G
- MCAO/R:
-
Middle cerebral artery occlusion and reperfusion
- MMPs:
-
Matrix metalloproteases
- MPO:
-
Myeloperoxidase
- NF-κB:
-
Nuclear factor kappa B
- PVDF:
-
Polyvinylidene fluoride
- ROS:
-
Reactive oxygen species
- TEM:
-
Transmission electron microscope
- TJPs:
-
Tight junction proteins
- TTC:
-
2,3,5-Triphenyltetrazolium chloride
- ZO-1:
-
Zona occludens-1
References
Katan M, Luft A. Global burden of stroke. Semin Neurol. 2018;38:208–11.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128.
Musuka TD, Wilton SB, Traboulsi M, Hill MD. Diagnosis and management of acute ischemic stroke: speed is critical. CMAJ. 2015;187:887–93.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133:e38–360.
Alluri H, Stagg HW, Wilson RL, Clayton RO, Sawant DA, Koneru M, et al. Reactive oxygen species-caspase-3 relationship in mediating blood–brain barrier endothelial cell hyperpermeability following oxygen–glucose deprivation and reoxygenation. Microcirculation. 2014;21:187–95.
Fujimura M, Gasche Y, Morita-Fujimura Y, Massengale J, Kawase M, Chan PH. Early appearance of activated matrix metalloproteinase-9 and blood–brain barrier disruption in mice after focal cerebral ischemia and reperfusion. Brain Res. 1999;84:92–100.
Fukuda AM, Badaut J. Aquaporin 4: a player in cerebral edema and neuroinflammation. J Neuroinflammation. 2012;279:2094–9.
Wicha P, Tocharus J, Janyou A, Jittiwat J, Changtam C, Suksamrarn A, et al. Hexahydrocurcumin protects against cerebral ischemia/reperfusion injury, attenuates inflammation, and improves antioxidant defenses in a rat stroke model. PLoS ONE. 2017;12:e0189211.
Wang G, Guo Q, Hossain M, Fazio V, Zeynalov E, Janigro D, et al. Bone marrow-derived cells are the major source of MMP-9 contributing to blood–brain barrier dysfunction and infarct formation after ischemic stroke in mice. Brain Res. 2009;1294:183–92.
Kwon I, Kim EH, del Zoppo GJ, Hoe HoJ. Ultrastructural and temporal changes of the microvascular basement membrane and astrocyte interface following focal cerebral ischemia. J Neurosci Res. 2009;87:668–76.
Candelario-Jalil E, Yang Y, Rosenberg GA. Diverse roles of matrix metalloproteinases and tissue inhibitors of metalloproteinases in neuroinflammation and cerebral ischemia. Neuroscience. 2009;15:983–94.
Yang C, Hawkins KE, Doré S, Candelario-Jalil E. Neuroinflammatory mechanisms of blood–brain barrier damage in ischemic stroke. Am J Physiol Cell Physiol. 2019;316:C135–53.
Gidday JM, Gasche YG, Copin JC, Shah AR, Perez RS, Shapiro SD, et al. Leukocyte-derived matrix metalloproteinase-9 mediates blood–brain barrier breakdown and is proinflammatory after transient focal cerebral ischemia. Am J Physiol Heart Circ Physiol. 2005;289:H558–68.
Liu W, Hendren J, Qin XJ, Shen J, Liu KJ. Normobarichyperoxia attenuates early blood–brain barrier disruption by inhibiting MMP-9-mediated occludin degradation in focal cerebral ischemia. J Neurochem. 2009;108:811–20.
Papadopoulos MC, Krishna S, Verkman AS. Aquaporin water channels and brain edema. Mt Sinai J Med. 2002;69:242–8.
Orlando RA, Gonzales AM, Royer RE, Deck LM, Vander Jagt DL. A chemical analog of curcumin as an improved inhibitor of amyloid Abeta oligomerization. PLoS ONE. 2012;7:e31869.
Srimuangwong K, Tocharus C, Tocharus J, Suksamrarn A, Chintana PY. Effects of hexahydrocurcumin in combination with 5-fluorouracil on dimethylhydrazine-induced colon cancer in rats. World J Gastroenterol. 2012;18:6951–9.
Srimuangwong K, Tocharus C, Chintana PY, Suksamrarn A, Tocharus J. Hexahydrocurcumin enhances inhibitory effect of 5-fluorouracil on HT-29 human colon cancer cells. World J Gastroenterol. 2012;18:2383–9.
Pagano E, Romano B, Izzo AA, Borrelli F. The clinical efficacy of curcumin-containing nutraceuticals: an overview of systematic reviews. Pharmacol Res. 2018;134:79–91.
Aggarwal BB, Sung B. Pharmacological basis for the role of curcumin in chronic diseases: an age-old spice with modern targets. Trends Pharmacol Sci. 2009;30:85–94.
Tuorkey M, Karolin K. Anti-ulcer activity of curcumin on experimental gastric ulcer in rats and its effect on oxidative stress/antioxidant, IL-6 and enzyme activities. Biomed Environ Sci. 2009;22:488–95.
Yang F, Lim GP, Begum AN, Ubeda OJ, Simmons MR, Ambegaokar SS, et al. Curcumin inhibits formation of amyloid beta oligomers and fibrils, binds plaques, and reduces amyloid in vivo. J Biol Chem. 2005;280:5892–901.
Zhang HS, Ruan Z, Sang WW. HDAC1/NF-κB pathway is involved in curcumin inhibiting of Tat-mediated long terminal repeat transactivation. J Cell Physiol. 2011;226:3385–91.
Akbar MU, Rehman K, Zia KM, Qadir MI, Akash MSH, Ibrahim M. Critical review on curcumin as a therapeutic agent: from traditional herbal medicine to an ideal therapeutic agent. Crit Rev Eukaryot Gene Expr. 2018;28:17–24.
Mantzorou M, Pavlidou E, Vasios G, Tsagalioti E, Giaginis C. Effects of curcumin consumption on human chronic diseases: a narrative review of the most recent clinical data. Phytother Res. 2018;32:957–75.
Huang L, Chen C, Zhang X, Li X, Chen Z, Yang C, et al. Neuroprotective effect of curcumin against cerebral ischemia-reperfusion via mediating autophagy and inflammation. J Mol Neurosci. 2018;64:129–39.
Li L, Li H, Li M. Curcumin protects against cerebral ischemia-reperfusion injury by activating JAK2/STAT3 signaling pathway in rats. Int J Clin Exp Med. 2015;8:14985–91.
Liu L, Zhang W, Wang L, Li Y, Tan B, Lu X, et al. Curcumin prevents cerebral ischemia reperfusion injury via increase of mitochondrial biogenesis. Neurochem Res. 2014;39:1322–31.
Dempe JS, Scheerle RK, Pfeiffer E, Metzler M. Metabolism and permeability of curcumin in cultured Caco-2 cells. Mol Nutr Food Res. 2013;57:1543–9.
Deters M, Knochenwefel H, Lindhorst D, Koal T, Mayer HH, Hänsel W. Different curcuminoids inhibit T-lymphocyte proliferation independently of their radical scavenging activities. Pharm Res. 2008;25:1822–7.
Somparn P, Phisalaphong C, Nakornchai S, Unchern S, Morales NP. Comparative antioxidant activities of curcumin and its demethoxy and hydrogenated derivatives. Biol Pharm Bull. 2007;30:74–7.
Ansari S, Azari H, McConnell DJ, Afzal A, Mocco J. Intraluminal middle cerebral artery occlusion (MCAO) model for ischemic stroke with laser doppler flowmetry guidance in mice. J Vis Exp. 2011;8:2879.
Longa EZ, Weinstein PR, Carlson S, Cummins R. Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke. 1989;20:84–91.
Ashwal S, Tone B, Tian HR, Cole DJ, Liwnicz BH, Pearce WJ. Core and penumbral nitric oxide synthase activity during cerebral ischemia and reperfusion in the rat pup. Pediatr Res. 1999;46:390–400.
Park S, Yamaguchi M, Zhou C, Calvert JW, Tang J, Zhang JH. Neurovascular protection reduces early brain injury after subarachnoid hemorrhage. Stroke. 2004;35:2412–27.
Shen F, Walker EJ, Jiang L, Degos V, Li J, Sun B, et al. Coexpression of angiopoietin-1 with VEGF increases the structural integrity of the blood–brain barrier and reduces atrophy volume. J Cereb Blood Flow Metab. 2011;31:2343–51.
Zhu MX, Lu C, Xia CM, Qiao ZW, Zhu DN. Simvastatin pretreatment protects cerebrum from neuronal injury by decreasing the expressions of phosphor-CaMK II and AQP4 in ischemic stroke rats. J Mol Neurosci. 2014;54:591–601.
Cui L, Zhang X, Yang R, Wang L, Liu L, Li M, et al. Neuroprotection of early and short-time applying atorvastatin in the acute phase of cerebral ischemia: down-regulated 12/15-LOX, p38MAPK and cPLA2 expression, ameliorated BBB permeability. Brain Res. 2010;1325:164–73.
Anand P, Kunnumakkara AB, Newman RA, Aggarwal BB. Bioavailability of curcumin: problems and promises. Mol Pharm. 2007;4:807–18.
Pan M, Huang TM, Lin JK. Biotransformation of curcumin through reduction and glucuronidation in mice. Drug Metab Dispos. 1999;27:486–94.
Yang Y, Estrada EY, Thompson JF, Liu W, Rosenberg GA. Matrix metalloproteinase-mediated disruption of tight junction proteins in cerebral vessels is reversed by synthetic matrix metalloproteinase inhibitor in focal ischemia in rat. J Cereb Blood Flow Metab. 2007;24:697–709.
Asahi M, Wang X, Mori T, Sumii T, Jung JC, Moskowitz MA, et al. Effects of matrix metalloproteinase-9 gene knock-out on the proteolysis of blood–brain barrier and white matter components after cerebral ischemia. J Neurosci. 2001;21:7724–32.
Luissint AC, Artus C, Glacial F, Ganeshamoorthy K, Couraud PO. Tight junctions at the blood brain barrier: physiological architecture and disease-associated dysregulation. Fluids Barriers CNS. 2012;9:23.
Bavarsad K, Barreto GE, Hadjzadeh MA, Sahebkar A. Protective effects of curcumin against ischemia-reperfusion injury in the nervous system. Mol Neurobiol. 2018;56:1391–404.
Moxon-Emre I, Schlichter LC. Neutrophil depletion reduces blood–brain barrier breakdown, axon injury, and inflammation after intracerebral hemorrhage. J Neuropathol Exp Neurol. 2011;70:218–35.
Manley GT, Binder DK, Papadopoulos MC, Verkman AS. New insights into water transport and edema in the central nervous system from phenotype analysis of aquaporin-4 null mice. Neuroscience. 2004;129:983–91.
Tang Y, Wu P, Su J, Xiang J, Cai D, Dong Q. Effects of aquaporin-4 on edema formation following intracerebral hemorrhage. Exp Neurol. 2010;223:485–95.
Amiry-Moghaddam M, Ottersen OP. The molecular basis of water transport in the brain. Nat Rev Neurosci. 2003;4:991–1001.
Mamtilahun M, Tang G, Zhang Z, Wang Y, Tang Y, Yang GY. Targeting water in the brain: role of aquaporin-4 in ischemic brain edema. Curr Drug Targets. 2019;20:748–55.
Yao X, Derugin N, Manley GT, Verkman AS. Reduced brain edema and infarct volume in aquaporin-4 deficient mice after transient focal cerebral ischemia. Neurosci Lett. 2015;584:368–72.
Yang C, Liu Z, Li H, Zhai F, Liu J, Bian J. Aquaporin-4 knockdown ameliorates hypoxic-ischemic cerebral edema in newborn piglets. IUBMB Life. 2015;67:182–90.
Katada R, Akdemir G, Asavapanumas N, Ratelade J, Zhang H, Verkman AS. Greatly improved survival and neuroprotection in aquaporin-4-knockout mice following global cerebral ischemia. FASEB J. 2014;28:705–14.
Akdemir G, Ratelade J, Asavapanumas N, Verkman AS. Neuroprotective effect of aquaporin-4 deficiency in a mouse model of severe global cerebral ischemia produced by transient 4-vessel occlusion. Neurosci Lett. 2014;574:70–5.
Acknowledgements
This study was supported by Functional Food Research Center for Well-being, Chiang Mai University and Faculty of Medicine Chiang Mai University. We also gratefully acknowledge support from the Thailand Research Fund (DBG6180030) and the Center of Excellence for Innovation in Chemistry, Office of the Higher Education Commission. PW acknowledges the financial support of the Royal Golden Jubilee (RGJ) PhD program (Grant No. PHD/0008/2558). We thank the staff of the Medical Science Research Equipment Center, Faculty of Medicine, Chiang Mai University for their help in the preparation of the tissue to be analyzed by Transmission Electron Microscopy.
Author information
Authors and Affiliations
Contributions
Conception: CT. Data curation: PW, JT, and CT. Funding acquisition: AS, CT. Methodology: PW, JT, AJ, JJ, and WC. Project administration: CT. Resources: AS. Supervision: CT. Writing—original draft: PW. Writing—review and editing: AS and CT.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wicha, P., Tocharus, J., Janyou, A. et al. Hexahydrocurcumin alleviated blood–brain barrier dysfunction in cerebral ischemia/reperfusion rats. Pharmacol. Rep 72, 659–671 (2020). https://doi.org/10.1007/s43440-019-00050-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-019-00050-9