Abstract
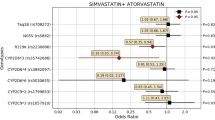
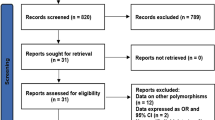
Statins are inhibitors of 3-hydroxy-3-methylglutaryl-CoA reductase, a key enzyme in cholesterol biosynthesis, that are highly effective in reducing plasma low-density lipoprotein (LDL) cholesterol and decreasing the risk of cardiovascular events. In recent years, a multitude of variants in genes involved in pharmacokinetics (PK) and pharmacodynamics (PD) have been suggested to influence the cholesterol-lowering response. However, the vast majority of studies have analyzed the pharmacogenetic associations in populations in Europe and the USA, whereas data in other populations, including Brazil, are mostly lacking. This narrative review provides an update of clinical studies on statin pharmacogenomics in Brazilian cohorts exploring lipid-lowering response, adverse events and pleiotropic effects. We find that variants in drug transporter genes (SLCO1B1 and ABCB1) positively impacted atorvastatin and simvastatin response, whereas variants in genes of drug metabolizing enzymes (CYP3A5) decreased response. Furthermore, multiple associations of variants in PD genes (HMGCR, LDLR and APOB) with statin response were identified. Few studies have explored statin-related adverse events, and only ABCB1 but not SLCO1B1 variants were robustly associated with increased risk in Brazil. Statin-related pleiotropic effects were shown to be influenced by variants in PD (LDLR, NR1H2) and antioxidant enzyme (NOS3, SOD2, MTHFR, SELENOP) genes. The findings of these studies indicate that statin pharmacogenomic associations are distinctly different in Brazil compared to other populations. This review also discusses the clinical implications of pharmacogenetic studies and the rising importance of investigating rare variants to explore their association with statin response.



Similar content being viewed by others
Abbreviations
- AD:
-
Alzheimer disease
- ADR:
-
Adverse drug reactions
- Apo:
-
Apolipoprotein
- ASCVD:
-
Atherosclerotic cardiovascular disease
- AUC:
-
Area under the curve
- CAC:
-
Coronary artery calcium
- CAR:
-
Constitutive androstane receptor
- CD36:
-
Scavenger receptor Class B2
- CETP:
-
Cholesteryl ester transfer protein
- CK:
-
Creatine kinase
- CoQ10:
-
Ubiquinone
- CPIC:
-
Clinical Pharmacogenetics Implementation Consortium
- CVD:
-
Cardiovascular disease
- eNOS:
-
Endothelial nitric oxide synthase
- ERα:
-
Estrogen receptor α
- GPX:
-
Glutathione peroxidase
- HC:
-
Hypercholesterolemia
- FH:
-
Familial hypercholesterolemia
- HDL:
-
High-density lipoprotein
- HL:
-
Hepatic lipase
- HMGR:
-
3-Hydroxy-3-methylglutaryl-CoA reductase
- GRS:
-
Genetic risk score
- LCAT:
-
Lecithin:cholesterol acyltransferase
- LDL:
-
Low-density lipoprotein
- LDLR:
-
LDL receptor
- MACE:
-
Major atherosclerotic cardiovascular events
- MTHFR:
-
Methylenetetrahydrofolate reductase
- MYLIP:
-
Myosin regulatory light chain interacting protein
- PCSK9:
-
Proprotein convertase subtilisin/kexin type 9
- PD:
-
Pharmacodynamics
- PK:
-
Pharmacokinetics
- PON1:
-
Paraoxonase 1
- PPARα:
-
Peroxisome proliferator-activated receptor
- PXR:
-
Pregnane X receptor
- RXRα:
-
Retinoid X receptor alpha
- SAMS:
-
Statin-associated muscle symptoms
- SCAP:
-
SREBP cleavage-activating protein
- Se:
-
Selenium
- SNVs:
-
Single nucleotide variations
- SOD2:
-
Manganese-dependent superoxide dismutase
- SRAE:
-
Statin-related adverse events
- SR-B1:
-
Scavenger receptor class B1
- SREBP:
-
Sterol regulatory element-binding proteins
- VLDL:
-
Very low-density lipoprotein
References
Gencer B, Marston NA, Im K, Cannon CP, Sever P, Keech A, et al. Efficacy and safety of lowering LDL cholesterol in older patients: a systematic review and meta-analysis of randomised controlled trials. Lancet. 2020;396(10263):1637–43.
Karlson BW, Palmer MK, Nicholls SJ, Barter PJ, Lundman P. Effects of age, gender and statin dose on lipid levels: results from the VOYAGER meta-analysis database. Atherosclerosis. 2017;265:54–9.
Maxwell WD, Ramsey LB, Johnson SG, Moore KG, Shtutman M, Schoonover JH, et al. Impact of pharmacogenetics on efficacy and safety of statin therapy for dyslipidemia. Pharmacotherapy. 2017;37(9):1172–90.
Guan ZW, Wu KR, Li R, Yin Y, Li XL, Zhang SF, et al. Pharmacogenetics of statins treatment: efficacy and safety. J Clin Pharm Ther. 2019;44(6):858–67.
Hirota T, Fujita Y, Ieiri I. An updated review of pharmacokinetic drug interactions and pharmacogenetics of statins. Expert Opin Drug Metab Toxicol. 2020;16(9):809–22.
Chora JR, Bourbon M. Pharmacogenomics of statins and familial hypercholesterolemia. Curr Opin Lipidol. 2021;32(2):96–102.
Cerda A, Hirata MH, Hirata RD. Pharmacogenetics of drug metabolizing enzymes in Brazilian populations. Drug Metabol Drug Interact. 2014;29(3):153–77. https://doi.org/10.1515/dmdi-2013-0067.
Hirata RDC, Cerda A, Genvigir FDV, Hirata MH. Pharmacogenetic implications in the management of metabolic diseases in Brazilian populations. Braz J Pharm Sci. 2018;54(spe):e01005.
Rocha KCE, Pereira BMV, Rodrigues AC. An update on efflux and uptake transporters as determinants of statin response. Expert Opin Drug Metab Toxicol. 2018;14(6):613–24.
Kameyama Y, Yamashita K, Kobayashi K, Hosokawa M, Chiba K. Functional characterization of SLCO1B1 (OATP-C) variants, SLCO1B1*5, SLCO1B1*15 and SLCO1B1*15+C1007G, by using transient expression systems of HeLa and HEK293 cells. Pharmacogenet Genomics. 2005;15(7):513–22.
Pasanen MK, Neuvonen M, Neuvonen PJ, Niemi M. SLCO1B1 polymorphism markedly affects the pharmacokinetics of simvastatin acid. Pharmacogenet Genomics. 2006;16(12):873–9.
Mori D, Kashihara Y, Yoshikado T, Kimura M, Hirota T, Matsuki S, et al. Effect of OATP1B1 genotypes on plasma concentrations of endogenous OATP1B1 substrates and drugs, and their association in healthy volunteers. Drug Metab Pharmacokinet. 2019;34(1):78–86.
Kitzmiller JP, Mikulik EB, Dauki AM, Murkherjee C, Luzum JA. Pharmacogenomics of statins: understanding susceptibility to adverse effects. Pharmgenomics Pers Med. 2016;9:97–106.
Fu Q, Li YP, Gao Y, Yang SH, Lu PQ, Jia M, et al. Lack of association between SLCO1B1 polymorphism and the lipid-lowering effects of atorvastatin and simvastatin in Chinese individuals. Eur J Clin Pharmacol. 2013;69(6):1269–74.
Giannakopoulou E, Ragia G, Kolovou V, Tavridou A, Tselepis AD, Elisaf M, et al. No impact of SLCO1B1 521T>C, 388A>G and 411G>A polymorphisms on response to statin therapy in the Greek population. Mol Biol Rep. 2014;41(7):4631–8.
Maeda K, Ieiri I, Yasuda K, Fujino A, Fujiwara H, Otsubo K, et al. Effects of organic anion transporting polypeptide 1B1 haplotype on pharmacokinetics of pravastatin, valsartan, and temocapril. Clin Pharmacol Ther. 2006;79(5):427–39.
Nies AT, Niemi M, Burk O, Winter S, Zanger UM, Stieger B, et al. Genetics is a major determinant of expression of the human hepatic uptake transporter OATP1B1, but not of OATP1B3 and OATP2B1. Genome Med. 2013;5(1):1.
Rodrigues AC, Perin PM, Purim SG, Silbiger VN, Genvigir FD, Willrich MA, et al. Pharmacogenetics of OATP transporters reveals that SLCO1B1 c.388A>G variant is determinant of increased atorvastatin response. Int J Mol Sci. 2011;12(9):5815–27.
Sortica VA, Fiegenbaum M, Lima LO, Van der Sand CR, Van der Sand LC, Ferreira ME, et al. SLCO1B1 gene variability influences lipid-lowering efficacy on simvastatin therapy in Southern Brazilians. Clin Chem Lab Med. 2012;50(3):441–8.
Rodrigues AC, Sobrino B, Genvigir FD, Willrich MA, Arazi SS, Dorea EL, Bernik MM, Bertolami M, Faludi AA, Brion MJ, Carracedo A, Hirata MH, Hirata RD. Genetic variants in genes related to lipid metabolism and atherosclerosis, dyslipidemia and atorvastatin response. Clin Chim Acta. 2013;417:8–11.
Dagli-Hernandez C, de Freitas RCC, Marçal EDSR, Gonçalves RM, Faludi AA, Borges JB, et al. Late response to rosuvastatin and statin-related myalgia due to SLCO1B1, SLCO1B3, ABCB11, and CYP3A5 variants in a patient with familial hypercholesterolemia: a case report. Ann Transl Med. 2021;9(1):76.
Hoenig MR, Walker PJ, Gurnsey C, Beadle K, Johnson L. The C3435T polymorphism in ABCB1 influences atorvastatin efficacy and muscle symptoms in a high-risk vascular cohort. J Clin Lipidol. 2011;5(2):91–6.
Su J, Xu H, Yang J, Yu Q, Yang S, Zhang J, et al. ABCB1 C3435T polymorphism and the lipid-lowering response in hypercholesterolemic patients on statins: a meta-analysis. Lipids Health Dis. 2015;14:122.
Becker ML, Visser LE, van Schaik RH, Hofman A, Uitterlinden AG, Stricker BH. Common genetic variation in the ABCB1 gene is associated with the cholesterol-lowering effect of simvastatin in males. Pharmacogenomics. 2009;10(11):1743–51.
Rebecchi IM, Rodrigues AC, Arazi SS, Genvigir FD, Willrich MA, Hirata MH, et al. ABCB1 and ABCC1 expression in peripheral mononuclear cells is influenced by gene polymorphisms and atorvastatin treatment. Biochem Pharmacol. 2009;77(1):66–75.
Rodrigues AC, Rebecchi IM, Bertolami MC, Faludi AA, Hirata MH, Hirata RD. High baseline serum total and LDL cholesterol levels are associated with MDR1 haplotypes in Brazilian hypercholesterolemic individuals of European descent. Braz J Med Biol Res. 2005;38(9):1389–97.
Fiegenbaum M, da Silveira FR, Van der Sand CR, Van der Sand LC, Ferreira ME, Pires RC, et al. The role of common variants of ABCB1, CYP3A4, and CYP3A5 genes in lipid-lowering efficacy and safety of simvastatin treatment. Clin Pharmacol Ther. 2005;78(5):551–8.
Behdad N, Kojuri J, Azarpira N, Masoomi A, Namazi S. Association of ABCB1 (C3435T) and ABCC1 (G2012T) polymorphisms with clinical response to atorvastatin in Iranian patients with primary hyperlipidemia. Iran Biomed J. 2017;21(2):120–5.
Fujikura K, Ingelman-Sundberg M, Lauschke VM. Genetic variation in the human cytochrome P450 supergene family. Pharmacogenet Genomics. 2015;25(12):584–94.
Becker ML, Visser LE, van Schaik RH, Hofman A, Uitterlinden AG, Stricker BH. Influence of genetic variation in CYP3A4 and ABCB1 on dose decrease or switching during simvastatin and atorvastatin therapy. Pharmacoepidemiol Drug Saf. 2010;19(1):75–81.
Kajinami K, Brousseau ME, Ordovas JM, Schaefer EJ. CYP3A4 genotypes and plasma lipoprotein levels before and after treatment with atorvastatin in primary hypercholesterolemia. Am J Cardiol. 2004;93(1):104–7.
Wang D, Guo Y, Wrighton SA, Cooke GE, Sadee W. Intronic polymorphism in CYP3A4 affects hepatic expression and response to statin drugs. Pharmacogenomics J. 2011;11(4):274–86.
Elens L, Becker ML, Haufroid V, Hofman A, Visser LE, Uitterlinden AG, et al. Novel CYP3A4 intron 6 single nucleotide polymorphism is associated with simvastatin-mediated cholesterol reduction in the Rotterdam Study. Pharmacogenet Genomics. 2011;21(12):861–6.
Willrich MA, Rodrigues AC, Cerda A, Genvigir FD, Arazi SS, Dorea EL, et al. Effects of atorvastatin on CYP3A4 and CYP3A5 mRNA expression in mononuclear cells and CYP3A activity in hypercholeresterolemic patients. Clin Chim Acta. 2013;421:157–63.
Bailey KM, Romaine SP, Jackson BM, Farrin AJ, Efthymiou M, Barth JH, et al. Hepatic metabolism and transporter gene variants enhance response to rosuvastatin in patients with acute myocardial infarction: the GEOSTAT-1 study. Circ Cardiovasc Genet. 2010;3(3):276–85.
Kitzmiller JP, Luzum JA, Baldassarre D, Krauss RM, Medina MW. CYP3A4*22 and CYP3A5*3 are associated with increased levels of plasma simvastatin concentrations in the cholesterol and pharmacogenetics study cohort. Pharmacogenet Genomics. 2014;24(10):486–91.
Kolovou G, Kolovou V, Ragia G, Mihas C, Diakoumakou O, Vasiliadis I, et al. CYP3A5 genotyping for assessing the efficacy of treatment with simvastatin and atorvastatin. Genet Mol Biol. 2015;38(2):129–37.
Kuehl P, Zhang J, Lin Y, Lamba J, Assem M, Schuetz J, et al. Sequence diversity in CYP3A promoters and characterization of the genetic basis of polymorphic CYP3A5 expression. Nat Genet. 2001;27(4):383–91.
Kivistö KT, Niemi M, Schaeffeler E, Pitkälä K, Tilvis R, Fromm MF, et al. Lipid-lowering response to statins is affected by CYP3A5 polymorphism. Pharmacogenetics. 2004;14(8):523–5.
Kim KA, Park PW, Lee OJ, Kang DK, Park JY. Effect of polymorphic CYP3A5 genotype on the single-dose simvastatin pharmacokinetics in healthy subjects. J Clin Pharmacol. 2007;47(1):87–93.
Rosales A, Alvear M, Cuevas A, Saavedra N, Zambrano T, Salazar LA. Identification of pharmacogenetic predictors of lipid-lowering response to atorvastatin in Chilean subjects with hypercholesterolemia. Clin Chim Acta. 2012;413(3–4):495–501.
Willrich MA, Hirata MH, Genvigir FD, Arazi SS, Rebecchi IM, Rodrigues AC, et al. CYP3A53A allele is associated with reduced lowering-lipid response to atorvastatin in individuals with hypercholesterolemia. Clin Chim Acta. 2008;398(1–2):15–20.
Alessandrini M, Asfaha S, Dodgen TM, Warnich L, Pepper MS. Cytochrome P450 pharmacogenetics in African populations. Drug Metab Rev. 2013;45(2):253–75.
Hirvensalo P, Tornio A, Neuvonen M, Kiander W, Kidron H, Paile-Hyvärinen M, et al. Enantiospecific pharmacogenomics of fluvastatin. Clin Pharmacol Ther. 2019;106(3):668–80.
Xiang Q, Zhang X, Ma L, Hu K, Zhang Z, Mu G, et al. The association between the SLCO1B1, apolipoprotein E, and CYP2C9 genes and lipid response to fluvastatin: a meta-analysis. Pharmacogenet Genomics. 2018;28(12):261–7.
Mangravite LM, Medina MW, Cui J, Pressman S, Smith JD, Rieder MJ, Guo X, Nickerson DA, Rotter JI, Krauss RM. Combined influence of LDLR and HMGCR sequence variation on lipid-lowering response to simvastatin. Arterioscler Thromb Vasc Biol. 2010;30(7):1485–92.
Leduc V, Bourque L, Poirier J, Dufour R. Role of rs3846662 and HMGCR alternative splicing in statin efficacy and baseline lipid levels in familial hypercholesterolemia. Pharmacogenet Genomics. 2016;26(1):1–11.
Cano-Corres R, Candás-Estébanez B, Padró-Miquel A, Fanlo-Maresma M, Pintó X, Alía-Ramos P. Influence of 6 genetic variants on the efficacy of statins in patients with dyslipidemia. J Clin Lab Anal. 2018;32(8):e22566.
Afonso MS, Machado RM, Lavrador MS, Quintao ECR, Moore KJ, Lottenberg AM. Molecular pathways underlying cholesterol homeostasis. Nutrients. 2018;10(6):760.
Luo J, Yang H, Song BL. Mechanisms and regulation of cholesterol homeostasis. Nat Rev Mol Cell Biol. 2020;21(4):225–45.
Miltiadous G, Xenophontos S, Bairaktari E, Ganotakis M, Cariolou M, Elisaf M. Genetic and environmental factors affecting the response to statin therapy in patients with molecularly defined familial hypercholesterolaemia. Pharmacogenet Genomics. 2005;15(4):219–25.
Berge KE, Ose L, Leren TP. Missense mutations in the PCSK9 gene are associated with hypocholesterolemia and possibly increased response to statin therapy. Arterioscler Thromb Vasc Biol. 2006;26(5):1094–100.
Humphries SE, Whittall RA, Hubbart CS, Maplebeck S, Cooper JA, Soutar AK, et al. Genetic causes of familial hypercholesterolaemia in patients in the UK: relation to plasma lipid levels and coronary heart disease risk. J Med Genet. 2006;43(12):943–9.
Polisecki E, Muallem H, Maeda N, Peter I, Robertson M, McMahon AD, et al. Genetic variation at the LDL receptor and HMG-CoA reductase gene loci, lipid levels, statin response, and cardiovascular disease incidence in PROSPER. Atherosclerosis. 2008;200(1):109–14.
Thompson JF, Hyde CL, Wood LS, Paciga SA, Hinds DA, Cox DR, et al. Comprehensive whole-genome and candidate gene analysis for response to statin therapy in the treating to new targets (TNT) cohort. Circ Cardiovasc Genet. 2009;2(2):173–81.
Chasman DI, Giulianini F, MacFadyen J, Barratt BJ, Nyberg F, Ridker PM. Genetic determinants of statin-induced low-density lipoprotein cholesterol reduction: the Justification for the use of statins in prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER) trial. Circ Cardiovasc Genet. 2012;5(2):257–64.
Salazar LA, Hirata MH, Quintão EC, Hirata RD. Lipid-lowering response of the HMG-CoA reductase inhibitor fluvastatin is influenced by polymorphisms in the low-density lipoprotein receptor gene in Brazilian patients with primary hypercholesterolemia. J Clin Lab Anal. 2000;14(3):125–31.
Zambrano T, Hirata MH, Cerda A, Dorea EL, Pinto GA, Gusukuma MC, et al. Impact of 3′UTR genetic variants in PCSK9 and LDLR genes on plasma lipid traits and response to atorvastatin in Brazilian subjects: a pilot study. Int J Clin Exp Med. 2015;8(4):5978–88.
Santos PC, Morgan AC, Jannes CE, Turolla L, Krieger JE, Santos RD, et al. Presence and type of low density lipoprotein receptor (LDLR) mutation influences the lipid profile and response to lipid-lowering therapy in Brazilian patients with heterozygous familial hypercholesterolemia. Atherosclerosis. 2014;233(1):206–10.
Miname MH, Bittencourt MS, Moraes SR, Alves RIM, Silva PRS, Jannes CE, et al. Coronary artery calcium and cardiovascular events in patients with familial hypercholesterolemia receiving standard lipid-lowering therapy. JACC Cardiovasc Imaging. 2019;12(9):1797–804.
Coutinho ER, Miname MH, Rocha VZ, Bittencourt MS, Jannes CE, Tada MT, et al. Familial hypercholesterolemia and cardiovascular disease in older individuals. Atherosclerosis. 2021;318:32–7.
Guzmán EC, Hirata MH, Quintão EC, Hirata RD. Association of the apolipoprotein B gene polymorphisms with cholesterol levels and response to fluvastatin in Brazilian individuals with high risk for coronary heart disease. Clin Chem Lab Med. 2000;38(8):731–6.
Anderson JM, Cerda A, Hirata MH, Rodrigues AC, Dorea EL, Bernik MM, et al. Influence of PCSK9 polymorphisms on plasma lipids and response to atorvastatin treatment in Brazilian subjects. J Clin Lipidol. 2014;8(3):256–64.
Marais AD. Apolipoprotein E in lipoprotein metabolism, health and cardiovascular disease. Pathology. 2019;51(2):165–76.
Fiegenbaum M, da Silveira FR, Van der Sand CR, Van der Sand LC, Ferreira ME, Pires RC, et al. Pharmacogenetic study of apolipoprotein E, cholesteryl ester transfer protein and hepatic lipase genes and simvastatin therapy in Brazilian subjects. Clin Chim Acta. 2005;362(1–2):182–8.
Cerda A, Genvigir FD, Willrich MA, Arazi SS, Bernik MM, Dorea EL, et al. Apolipoprotein E mRNA expression in mononuclear cells from normolipidemic and hypercholesterolemic individuals treated with atorvastatin. Lipids Health Dis. 2011;10:206.
Issa MH, Cerda A, Genvigir FD, Cavalli SA, Bertolami MC, Faludi AA, et al. Atorvastatin and hormone therapy effects on APOE mRNA expression in hypercholesterolemic postmenopausal women. J Steroid Biochem Mol Biol. 2012;128(3–5):139–44.
Brown AJ, Hsieh J. Foiling IDOL to help control cholesterol. Circ Res. 2016;118(3):371–3.
Weissglas-Volkov D, Calkin AC, Tusie-Luna T, Sinsheimer JS, Zelcer N, Riba L, et al. The N342S MYLIP polymorphism is associated with high total cholesterol and increased LDL receptor degradation in humans. J Clin Invest. 2011;121(8):3062–71.
Adi D, Abuzhalihan J, Wang YH, Baituola G, Wu Y, Xie X, et al. IDOL gene variant is associated with hyperlipidemia in Han population in Xinjiang, China. Sci Rep. 2020;10(1):14280.
Santos PC, Morgan AC, Jannes CE, Krieger JE, Santos RD, Pereira AC. The MYLIP p.N342S polymorphism is associated with response to lipid-lowering therapy in Brazilian patients with familial hypercholesterolemia. Pharmacogenet Genomics. 2014;24(11):548–55.
Radhakrishnan A, Goldstein JL, McDonald JG, Brown MS. Switch-like control of SREBP-2 transport triggered by small changes in ER cholesterol: a delicate balance. Cell Metab. 2008;8(6):512–21.
Lee SH, Lee JH, Im SS. The cellular function of SCAP in metabolic signaling. Exp Mol Med. 2020;52(5):724–9.
Fiegenbaum M, Silveira FR, Van der Sand CR, Van der Sand LC, Ferreira ME, Pires RC, et al. Determinants of variable response to simvastatin treatment: the role of common variants of SCAP, SREBF-1a and SREBF-2 genes. Pharmacogenomics J. 2005;5(6):359–64.
Arazi SS, Genvigir FD, Willrich MA, Hirata MH, Dorea EL, Bernik M, et al. Atorvastatin effects on SREBF1a and SCAP gene expression in mononuclear cells and its relation with lowering-lipids response. Clin Chim Acta. 2008;393(2):119–24.
Gao J, Xie W. Pregnane X receptor and constitutive androstane receptor at the crossroads of drug metabolism and energy metabolism. Drug Metab Dispos. 2010;38(12):2091–5.
Xiao L, Wang J, Jiang M, Xie W, Zhai Y. The emerging role of constitutive androstane receptor and its cross talk with liver X receptors and peroxisome proliferator-activated receptor A in lipid metabolism. Vitam Horm. 2013;91:243–58.
Yu XH, Zheng XL, Tang CK. Peroxisome proliferator-activated receptor α in lipid metabolism and atherosclerosis. Adv Clin Chem. 2015;71:171–203.
Omiecinski CJ, Vanden Heuvel JP, Perdew GH, Peters JM. Xenobiotic metabolism, disposition, and regulation by receptors: from biochemical phenomenon to predictors of major toxicities. Toxicol Sci. 2011;120(Suppl 1):S49–75.
Lima LO, Bruxel EM, Hutz MH, Van der Sand CR, Van der Sand LC, Ferreira ME, et al. Influence of PPARA, RXRA, NR1I2 and NR1I3 gene polymorphisms on the lipid-lowering efficacy and safety of statin therapy. Arq Bras Endocrinol Metabol. 2013;57(7):513–9.
Casazza K, Page GP, Fernandez JR. The association between the rs2234693 and rs9340799 estrogen receptor alpha gene polymorphisms and risk factors for cardiovascular disease: a review. Biol Res Nurs. 2010;12(1):84–97.
Smiderle L, Fiegenbaum M, Hutz MH, Van Der Sand CR, Van Der Sand LC, Ferreira ME, et al. ESR1 polymorphisms and statin therapy: a sex-specific approach. Pharmacogenomics J. 2016;16(6):507–13.
Ouimet M, Barrett TJ, Fisher EA. HDL and reverse cholesterol transport. Circ Res. 2019;124(10):1505–18.
Marques LR, Diniz TA, Antunes BM, Rossi FE, Caperuto EC, Lira FS, et al. Reverse cholesterol transport: molecular mechanisms and the non-medical approach to enhance HDL cholesterol. Front Physiol. 2018;9:526.
González FEM, Ponce-Ruíz N, Rojas-García AE, Bernal-Hernández YY, Mackness M, Ponce-Gallegos J, et al. PON1 concentration and high-density lipoprotein characteristics as cardiovascular biomarkers. Arch Med Sci Atheroscler Dis. 2019;4:e47–54.
Sorkin SC, Forestiero FJ, Hirata MH, Guzmán EC, Cavalli SA, Bertolami MC, et al. APOA1 polymorphisms are associated with variations in serum triglyceride concentrations in hypercholesterolemic individuals. Clin Chem Lab Med. 2005;43(12):1339–45.
Genvigir FD, Soares SA, Hirata MH, Willrich MA, Arazi SS, Rebecchi IM, et al. Effects of ABCA1 SNPs, including the C-105T novel variant, on serum lipids of Brazilian individuals. Clin Chim Acta. 2008;389(1–2):79–86.
Cerda A, Genvigir FD, Arazi SS, Hirata MH, Dorea EL, Bernik MM, et al. Influence of SCARB1 polymorphisms on serum lipids of hypercholesterolemic individuals treated with atorvastatin. Clin Chim Acta. 2010;411(9–10):631–7.
de Souza JA, Menin A, Lima LO, Smiderle L, Hutz MH, Van Der Sand CR, et al. PON1 polymorphisms are predictors of ability to attain HDL-C goals in statin-treated patients. Clin Biochem. 2015;48(16–17):1039–44.
Zhao L, Varghese Z, Moorhead JF, Chen Y, Ruan XZ. CD36 and lipid metabolism in the evolution of atherosclerosis. Br Med Bull. 2018;126(1):101–12.
Oesterle A, Laufs U, Liao JK. Pleiotropic effects of statins on the cardiovascular system. Circ Res. 2017;120(1):229–43.
Nagassaki S, Sertório JT, Metzger IF, Bem AF, Rocha JB, Tanus-Santos JE. eNOS gene T-786C polymorphism modulates atorvastatin-induced increase in blood nitrite. Free Radic Biol Med. 2006;41(7):1044–9.
Crawford A, Fassett RG, Geraghty DP, Kunde DA, Ball MJ, Robertson IK, et al. Relationships between single nucleotide polymorphisms of antioxidant enzymes and disease. Gene. 2012;501(2):89–103.
Duarte T, da Cruz IB, Barbisan F, Capelleto D, Moresco RN, Duarte MM. The effects of rosuvastatin on lipid-lowering, inflammatory, antioxidant and fibrinolytics blood biomarkers are influenced by Val16Ala superoxide dismutase manganese-dependent gene polymorphism. Pharmacogenomics J. 2016;16(6):501–6.
Moriguchi Watanabe L, Bueno AC, de Lima LF, Ferraz-Bannitz R, Dessordi R, Guimarães MP, et al. Genetically determined variations of selenoprotein P are associated with antioxidant, muscular, and lipid biomarkers in response to Brazil nut consumption by patients using statins. Br J Nutr. 2021. https://doi.org/10.1017/S000711452100146X (Epub ahead of print).
Sposito AC, Faria Neto JR, Carvalho LS, Lorenzatti A, Cafferata A, Elikir G, et al. Statin-associated muscle symptoms: position paper from the Luso-Latin American Consortium. Curr Med Res Opin. 2017;33(2):239–51.
Turner RM, Pirmohamed M. Statin-related myotoxicity: a comprehensive review of pharmacokinetic, pharmacogenomic and muscle components. J Clin Med. 2019;9(1):22.
Stroes ES, Thompson PD, Corsini A, Vladutiu GD, Raal FJ, Ray KK, et al. Statin-associated muscle symptoms: impact on statin therapy—European Atherosclerosis Society Consensus Panel Statement on Assessment, Aetiology and Management. Eur Heart J. 2015;36(17):1012–22.
Do Nascimento RCRM, Guerra Jr AA, Alvares J, Gomes IC, Godman B, Bennie M, et al. Statin use in Brazil: findings and implications. Curr Med Res Opin. 2018;34(10):1809–17.
Nogueira AA, Strunz CM, Takada JY, Mansur AP. Biochemical markers of muscle damage and high serum concentration of creatine kinase in patients on statin therapy. Biomark Med. 2019;13(8):619–26.
Kee PS, Chin PKL, Kennedy MA, Maggo SDS. Pharmacogenetics of statin-induced myotoxicity. Front Genet. 2020;11:575678.
SEARCH Collaborative Group, Link E, Parish S, Armitage J, Bowman L, Heath S, et al. SLCO1B1 variants and statin-induced myopathy—a genomewide study. N Engl J Med. 2008;359(8):789–99.
Hou Q, Li S, Li L, Li Y, Sun X, Tian H. Association between SLCO1B1 gene T521C polymorphism and statin-related myopathy risk: a meta-analysis of case–control studies. Medicine (Baltimore). 2015;94(37):e1268.
Ramsey LB, Johnson SG, Caudle KE, Haidar CE, Voora D, Wilke RA, et al. The clinical pharmacogenetics implementation consortium guideline for SLCO1B1 and simvastatin-induced myopathy: 2014 update. Clin Pharmacol Ther. 2014;96(4):423–8.
Santos PC, Gagliardi AC, Miname MH, Chacra AP, Santos RD, Krieger JE, et al. SLCO1B1 haplotypes are not associated with atorvastatin-induced myalgia in Brazilian patients with familial hypercholesterolemia. Eur J Clin Pharmacol. 2012;68(3):273–9.
Mohammad S, Nguyen H, Nguyen M, Abdel-Rasoul M, Nguyen V, Nguyen CD, et al. Pleiotropic effects of statins: untapped potential for statin pharmacotherapy. Curr Vasc Pharmacol. 2019;17(3):239–61.
Botelho PB, Fioratti CO, Rogero MM, Barroso LP, Bertolami MC, Castro IA. Association between diet and polymorphisms in individuals with statin-controlled dyslipidaemia grouped according to oxidative stress biomarkers. Braz J Pharm Sci. 2012;48:39–49.
Cozma A, Fodor A, Orasan OH, Vulturar R, Samplelean D, Negrean V, Muresan C, Suharoschi R, Sitar-Taut A. Pharmacogenetic implications of eNOS polymorphisms (Glu298Asp, T786C, 4b/4a) in cardiovascular drug therapy. In Vivo. 2019;33(4):1051–8.
Souza-Costa DC, Sandrim VC, Lopes LF, Gerlach RF, Rego EM, Tanus-Santos JE. Anti-inflammatory effects of atorvastatin: modulation by the T-786C polymorphism in the endothelial nitric oxide synthase gene. Atherosclerosis. 2007;193(2):438–44.
Nagassaki S, Herculano RD, Graeff CF, Tanus-Santos JE. eNOS T-786C polymorphism affects atorvastatin-induced changes in erythrocyte membrane fluidity. Eur J Clin Pharmacol. 2009;65(4):385–92.
Andrade VL, Sertório JT, Eleuterio NM, Tanus-Santos JE, Fernandes KS, Sandrim VC. Simvastatin treatment increases nitrite levels in obese women: modulation by T(-786)C polymorphism of eNOS. Nitric Oxide. 2013;33:83–7.
Maitland-van der Zee AH, Lynch A, Boerwinkle E, Arnett DK, Davis BR, Leiendecker-Foster C, et al. Interactions between the single nucleotide polymorphisms in the homocysteine pathway (MTHFR 677C>T, MTHFR 1298 A>C, and CBSins) and the efficacy of HMG-CoA reductase inhibitors in preventing cardiovascular disease in high-risk patients of hypertension: the GenHAT study. Pharmacogenet Genomics. 2008;18(8):651–6.
Villela MP, Andrade VL, Eccard B, Jordão AA, Sertório JT, Tanus-Santos JE, et al. Homocysteine and nitrite levels are modulated by MTHFR 677C>T polymorphism in obese women treated with simvastatin. Clin Exp Pharmacol Physiol. 2014;41(10):744–7.
de Oliveira FF, Berretta JM, de Almeida Junior GV, de Almeida SS, Chen ES, Smith MC, et al. Pharmacogenetic analyses of variations of measures of cardiovascular risk in Alzheimer’s dementia. Indian J Med Res. 2019;150(3):261–71.
de Oliveira FF, Chen ES, Smith MC, Bertolucci PHF. Selected LDLR and APOE polymorphisms affect cognitive and functional response to lipophilic statins in Alzheimer’s disease. J Mol Neurosci. 2020;70(10):1574–88.
Faludi AA, Izar MCO, Saraiva JFK, Chacra APM, Bianco HT, Afiune AN, et al. Atualização da Diretriz Brasileira de Dislipidemias e Prevenção da Aterosclerose—2017. Arq Bras Cardiol. 2017;109(2 Suppl 1):1–76.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–88.
Brasil. Ministério da Saúde. Protocolo Clínico e Diretrizes Terapêuticas da Dislipidemia: prevenção de eventos cardiovasculares e pancreatite. Brasil. 2019. Available at: https://www.in.gov.br/web/dou/-/portaria-conjunta-n-8-de-30-de-julho-de-2019-209272888. Accessed 15 Apr 2021.
Karlson BW, Wiklund O, Palmer MK, Nicholls SJ, Lundman P, Barter PJ. Variability of low-density lipoprotein cholesterol response with different doses of atorvastatin, rosuvastatin, and simvastatin: results from VOYAGER. Eur Heart J Cardiovasc Pharmacother. 2016;2(4):212–7.
Postmus I, Trompet S, Deshmukh HA, Barnes MR, Li X, Warren HR, et al. Pharmacogenetic meta-analysis of genome-wide association studies of LDL cholesterol response to statins. Nat Commun. 2014;5:5068.
Guglielmi V, Bellia A, Pecchioli S, Della-Morte D, Parretti D, Cricelli I, et al. Effectiveness of adherence to lipid lowering therapy on LDL-cholesterol in patients with very high cardiovascular risk: a real-world evidence study in primary care. Atherosclerosis. 2017;263:36–41.
Cohen JD, Brinton EA, Ito MK, Jacobson TA. Understanding Statin Use in America and Gaps in Patient Education (USAGE): an internet-based survey of 10,138 current and former statin users. J Clin Lipidol. 2012;6(3):208–15.
Travassos C, Laguardia J, Marques PM, Mota JC, Szwarcwald CL. Comparison between two race/skin color classifications in relation to health-related outcomes in Brazil. Int J Equity Health. 2011;10:35.
Suarez-Kurtz G. Pharmacogenetics in the Brazilian population. Front Pharmacol. 2010;1:118.
Suarez-Kurtz G, Pena SD, Struchiner CJ, Hutz MH. Pharmacogenomic diversity among Brazilians: influence of ancestry, self-reported color, and geographical origin. Front Pharmacol. 2012;3:191.
Rodrigues-Soares F, Kehdy FSG, Sampaio-Coelho J, Andrade PXC, Céspedes-Garro C, Zolini C, et al. Genetic structure of pharmacogenetic biomarkers in Brazil inferred from a systematic review and population-based cohorts: a RIBEF/EPIGEN-Brazil initiative. Pharmacogenomics J. 2018;18(6):749–59.
Mega JL, Stitziel NO, Smith JG, Chasman DI, Caulfield M, Devlin JJ, et al. Genetic risk, coronary heart disease events, and the clinical benefit of statin therapy: an analysis of primary and secondary prevention trials. Lancet. 2015;385(9984):2264–71.
Natarajan P, Young R, Stitziel NO, Padmanabhan S, Baber U, Mehran R, et al. Polygenic risk score identifies subgroup with higher burden of atherosclerosis and greater relative benefit from statin therapy in the primary prevention setting. Circulation. 2017;135(22):2091–101.
Tennessen JA, Bigham AW, O’Connor TD, Fu W, Kenny EE, Gravel S, et al. Evolution and functional impact of rare coding variation from deep sequencing of human exomes. Science. 2012;337(6090):64–9.
1000 Genomes Project Consortium, Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, et al. A global reference for human genetic variation. Nature. 2015;526(7571):68–74.
Gordon AS, Tabor HK, Johnson AD, Snively BM, Assimes TL, Auer PL, et al. Quantifying rare, deleterious variation in 12 human cytochrome P450 drug-metabolism genes in a large-scale exome dataset. Hum Mol Genet. 2014;23(8):1957–63.
Schaller L, Lauschke VM. The genetic landscape of the human solute carrier (SLC) transporter superfamily. Hum Genet. 2019;138(11–12):1359–77.
Zhang B, Lauschke VM. Genetic variability and population diversity of the human SLCO (OATP) transporter family. Pharmacol Res. 2019;139:550–9.
Xiao Q, Zhou Y, Lauschke VM. Ethnogeographic and inter-individual variability of human ABC transporters. Hum Genet. 2020;139(5):623–46.
Zhou Y, Mägi R, Milani L, Lauschke VM. Global genetic diversity of human apolipoproteins and effects on cardiovascular disease risk. J Lipid Res. 2018;59(10):1987–2000.
Ingelman-Sundberg M, Mkrtchian S, Zhou Y, Lauschke VM. Integrating rare genetic variants into pharmacogenetic drug response predictions. Hum Genomics. 2018;12(1):26.
Santos M, Niemi M, Hiratsuka M, Kumondai M, Ingelman-Sundberg M, Lauschke VM, et al. Novel copy-number variations in pharmacogenes contribute to interindividual differences in drug pharmacokinetics. Genet Med. 2018;20(6):622–9.
Ramsey LB, Bruun GH, Yang W, Treviño LR, Vattathil S, Scheet P, et al. Rare versus common variants in pharmacogenetics: SLCO1B1 variation and methotrexate disposition. Genome Res. 2012;22(1):1–8.
Kozyra M, Ingelman-Sundberg M, Lauschke VM. Rare genetic variants in cellular transporters, metabolic enzymes, and nuclear receptors can be important determinants of interindividual differences in drug response. Genet Med. 2017;19(1):20–9.
Lauschke VM, Ingelman-Sundberg M. Emerging strategies to bridge the gap between pharmacogenomic research and its clinical implementation. NPJ Genomic Med. 2020;5:9.
Zhou Y, Fujikura K, Mkrtchian S, Lauschke VM. Computational methods for the pharmacogenetic interpretation of next generation sequencing data. Front Pharmacol. 2018;9:1437.
Zhou Y, Mkrtchian S, Kumondai M, Hiratsuka M, Lauschke VM. An optimized prediction framework to assess the functional impact of pharmacogenetic variants. Pharmacogenomics J. 2019;19(2):115–26.
Zhou Y, Dagli-Hernandez C, Lauschke VM. Population-scale predictions of DPD and TPMT phenotypes using a quantitative pharmacogene-specific ensemble classifier. Br J Cancer. 2020;123(12):1782–9.
Russell LE, Zhou Y, Lauschke VM, Kim RB. In vitro functional characterization and in silico prediction of rare genetic variation in the bile acid and drug transporter, Na+-taurocholate cotransporting polypeptide (NTCP, SLC10A1). Mol Pharm. 2020;17(4):1170–81.
Davis JP, Huyghe JR, Locke AE, Jackson AU, Sim X, Stringham HM, et al. Common, low-frequency, and rare genetic variants associated with lipoprotein subclasses and triglyceride measures in Finnish men from the METSIM study. PLoS Genet. 2017;13(10):e1007079.
Igartua C, Mozaffari SV, Nicolae DL, Ober C. Rare non-coding variants are associated with plasma lipid traits in a founder population. Sci Rep. 2017;7(1):16415.
Neřoldová M, Stránecký V, Hodaňová K, Hartmannová H, Piherová L, Přistoupilová A, et al. Rare variants in known and novel candidate genes predisposing to statin-associated myopathy. Pharmacogenomics. 2016;17(13):1405–14.
Floyd JS, Bloch KM, Brody JA, Maroteau C, Siddiqui MK, Gregory R, et al. Pharmacogenomics of statin-related myopathy: meta-analysis of rare variants from whole-exome sequencing. PLoS ONE. 2019;14(6):e0218115.
Maitland-van der Zee AH, Klungel OH, Stricker BH, Veenstra DL, Kastelein JJ, Hofman A, et al. Pharmacoeconomic evaluation of testing for angiotensin-converting enzyme genotype before starting beta-hydroxy-beta-methylglutaryl coenzyme A reductase inhibitor therapy in men. Pharmacogenetics. 2004;14(1):53–60.
Kemp LK, Doran CM, Vos T, Hall W. Cost-effectiveness analysis of genetic screening for the Taq1B polymorphism in the secondary prevention of coronary heart disease. Expert Rev Pharmacoecon Outcomes Res. 2007;7(2):119–28.
Parthan A, Leahy KJ, O’Sullivan AK, Iakoubova OA, Bare LA, Devlin JJ, et al. Cost effectiveness of targeted high-dose atorvastatin therapy following genotype testing in patients with acute coronary syndrome. Pharmacoeconomics. 2013;31(6):519–31.
Sorich MJ, Wiese MD, O’Shea RL, Pekarsky B. Review of the cost effectiveness of pharmacogenetic-guided treatment of hypercholesterolaemia. Pharmacoeconomics. 2013;31(5):377–91.
Vassy JL, Chun S, Advani S, Ludin SA, Smith JG, Alligood EC. Impact of SLCO1B1 pharmacogenetic testing on patient and healthcare outcomes: a systematic review. Clin Pharmacol Ther. 2019;106(2):360–73.
Jansen ME, Rigter T, Rodenburg W, Fleur TMC, Houwink EJF, Weda M, et al. Review of the reported measures of clinical validity and clinical utility as arguments for the implementation of pharmacogenetic testing: a case study of statin-induced muscle toxicity. Front Pharmacol. 2017;8:555.
Zhou Y, Krebs K, Milani L, Lauschke VM. Global frequencies of clinically important HLA alleles and their implications for the cost-effectiveness of preemptive pharmacogenetic testing. Clin Pharmacol Ther. 2021;109(1):160–74.
Dong OM, Wheeler SB, Cruden G, Lee CR, Voora D, Dusetzina SB, et al. Cost-effectiveness of multigene pharmacogenetic testing in patients with acute coronary syndrome after percutaneous coronary intervention. Value Health. 2020;23(1):61–73.
Zhu Y, Moriarty JP, Swanson KM, Takahashi PY, Bielinski SJ, Weinshilboum R, et al. A model-based cost-effectiveness analysis of pharmacogenomic panel testing in cardiovascular disease management: preemptive, reactive, or none? Genet Med. 2021;23(3):461–70.
Acknowledgements
CDH is a recipient of a fellowship from FAPESP, Brazil. MHH and RDCH are recipients of fellowships from CNPq, Brazil. FDVG and TDCH were recipients of fellowships from FAPESP, Brazil.
Author information
Authors and Affiliations
Contributions
CDH contributed to the conception, design, data collection, analysis and interpretation, and drafting of the article. YZ and VML contributed to the sections that evaluate the cost-effectiveness of genotyping and describe the effects of rare variants and their clinical implications. FDVG and TDCH contributed to data collection, figure preparation, drafting and critical revision of the article. MHH and RDCH contributed to the conception, design, data interpretation and critical revision of the article.
Corresponding author
Ethics declarations
Conflict of interest
CDH, FDVG, TDCH, MHH, and RDCH declare no conflict of interest. YZ is co-founder and CEO of PersoMedix AB. VML is CEO and shareholder of HepaPredict AB, co-founder and chairman of the board of PersoMedix AB, and consultant for Enginzyme AB.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dagli-Hernandez, C., Zhou, Y., Lauschke, V.M. et al. Pharmacogenomics of statins: lipid response and other outcomes in Brazilian cohorts. Pharmacol. Rep 74, 47–66 (2022). https://doi.org/10.1007/s43440-021-00319-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-021-00319-y